Abstract
Aims
Mild Cognitive impairment (MCI) is common in type 2 diabetes mellitus (T2DM) patients. The impaired cognitive function had harmful effect on patients’ diabetic conditions. This study aimed to estimate the prevalence of MCI in T2DM (T2DM-MCI) patients by conducting a systematic review and meta-analysis of observational studies.
Methods
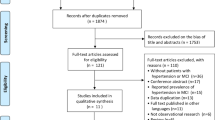
We carried out a literature search until June 1, 2020, for all observational studies in the following databases: Medline (PubMed), Web of Science, and Embase. Two independent reviewers initially screened the eligible articles. Then, a meta-analysis (random effects model) was conducted to estimate the prevalence of MCI in people with T2DM with STATA 16.
Results
A total of 1808 articles were first considered after reading title and abstract, 12 of which remained after reviewing the full text. The combined prevalence of MCI in T2DM patients was estimated to be 45.0% (95% CI=36.0, 54.0). There was no significant heterogeneity through meta-regression and sensitivity analysis. Overall, Europe (n=2, r=36.6%, 95% CI=26.3, 46.9, I2=82.3%) had a lower prevalence than Asia (n=10, r=46.4%, 95% CI=36.2, 56.6, I2=98%). The overall prevalence in female patients (n=14, r=46.9%, 95% CI=34, 59.8, I2=98.3%) was higher than that in male patients (n=14, r=38.8%, 95% CI=27, 50.7, I2=98%). Subgroup analysis based on age demonstrated a lower prevalence in patients older than 60 years (n=9, r=44.3%, 95% CI=33.1, 55.6, I2=98.3%) than patients younger than 60 years (n=3, r=46.4%, 95% CI=33.3, 59.5, I2=91.2%).
Conclusion
Our results demonstrate that the pooled estimated prevalence of mild cognitive impairment in type 2 diabetes mellitus patients is high worldwide, especially in China Asia. Primary care clinicians should pay more attention to the cognitive function of T2DM patients, as mild cognitive impairment is one of the risk factors for Alzheimer's disease.












Similar content being viewed by others
Reference
Saeedi P, Petersohn I, Salpea P et al (2019) Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract 157:107843. https://doi.org/10.1016/j.diabres.2019.107843
Reijmer YD, Brundel M, de Bresser J et al (2013) Microstructural white matter abnormalities and cognitive functioning in type 2 diabetes: a diffusion tensor imaging study. Diabetes Care 36(1):137–144. https://doi.org/10.2337/dc12-0493
Geijselaers SLC, Sep SJS, Stehouwer CDA, Biessels GJ (2015) Glucose regulation, cognition, and brain MRI in type 2 diabetes: a systematic review. Lancet Diabetes Endocrinol 3(1):75–89. https://doi.org/10.1016/S2213-8587(14)70148-2
Koekkoek PS, Kappelle LJ, van den Berg E, Rutten GE, Biessels GJ (2015) Cognitive function in patients with diabetes mellitus: guidance for daily care. Lancet Neurol 14(3):329–340. https://doi.org/10.1016/S1474-4422(14)70249-2
Langa KM, Levine DA (2014) The diagnosis and management of mild cognitive impairment: a clinical review. JAMA 312(23):2551–2561. https://doi.org/10.1001/jama.2014.13806
Petersen RC (2004) Mild cognitive impairment as a diagnostic entity. J intern med 256(3):183–194. https://doi.org/10.1111/j.1365-2796.2004.01388.x
Winblad B, Palmer K, Kivipelto M et al (2004) Mild cognitive impairment–beyond controversies, towards a consensus: report of the international working group on mild cognitive impairment. J Intern Med 256(3):240–246. https://doi.org/10.1111/j.1365-2796.2004.01380.x
Albert MS, DeKosky ST, Dickson D et al (2011) The diagnosis of mild cognitive impairment due to alzheimer’s disease: recommendations from the national institute on aging-alzheimer’s association workgroups on diagnostic guidelines for alzheimer’s disease. Alzheimer’s Dement : J Alzheimer’s Assoc 7(3):270–279. https://doi.org/10.1016/j.jalz.2011.03.008
Sachs-Ericsson N, Blazer DG (2015) The new DSM-5 diagnosis of mild neurocognitive disorder and its relation to research in mild cognitive impairment. Aging Ment Health 19(1):2–12. https://doi.org/10.1080/13607863.2014.920303
Sanford AM (2017) Mild cognitive impairment. Clin Geriatr Med 33(3):325–337. https://doi.org/10.1016/j.cger.2017.02.005
Mitchell AJ, Shiri-Feshki M (2009) Rate of progression of mild cognitive impairment to dementia–meta-analysis of 41 robust inception cohort studies. Acta psychiatrica Scandinavica 119(4):252–265. https://doi.org/10.1111/j.1600-0447.2008.01326.x
Roberts RO, Knopman DS, Mielke MM et al (2014) Higher risk of progression to dementia in mild cognitive impairment cases who revert to normal. Neurology 82(4):317–325. https://doi.org/10.1212/WNL.0000000000000055
Groeneveld O, Reijmer Y, Heinen R et al (2018) Brain imaging correlates of mild cognitive impairment and early dementia in patients with type 2 diabetes mellitus. Nutr Metab Cardiovasc Dis 28(12):1253–1260. https://doi.org/10.1016/j.numecd.2018.07.008
Vagelatos NT, Eslick GD (2013) Type 2 diabetes as a risk factor for Alzheimer’s disease: the confounders, interactions, and neuropathology associated with this relationship. Epidemiol rev 35:152–160. https://doi.org/10.1093/epirev/mxs012
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):e1-34. https://doi.org/10.1016/j.jclinepi.2009.06.006
Harlow SD, Linet MS (1989) Agreement between questionnaire data and medical records. The evidence for accuracy of recall. Am J Epidemiol 129(2):233–248. https://doi.org/10.1093/oxfordjournals.aje.a115129
von Elm E, Altman DG, Egger M et al (2014) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg (Lond, Eng) 12(12):1495–1499. https://doi.org/10.1016/j.ijsu.2014.07.013
Nyaga VN, Arbyn M, Aerts M (2014) Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Pub Health 72(1):39. https://doi.org/10.1186/2049-3258-72-39
Ma F, Wu T, Miao R et al (2015) Conversion of mild cognitive impairment to dementia among subjects with diabetes: a population-based study of incidence and risk factors with five years of follow-up. J Alzheimer’s Dis : JAD 43(4):1441–1449. https://doi.org/10.3233/jad-141566
Wang P, Huang R, Lu S et al (2016) RAGE and AGEs in mild cognitive impairment of diabetic patients: a cross-sectional study. PloS one 11(1):e0145521. https://doi.org/10.1371/journal.pone.0145521
Albai O, Frandes M, Timar R, Roman D, Timar B (2019) Risk factors for developing dementia in type 2 diabetes mellitus patients with mild cognitive impairment. Neuropsychiatr Dis Treat 15:167–175. https://doi.org/10.2147/NDT.S189905
Atif M, Saleem Q, Scahill S (2018) Depression and mild cognitive impairment (MCI) among elderly patients with type 2 diabetes mellitus in Pakistan: possible determinants. Int J Diabetes Dev C 38(3):312–320. https://doi.org/10.1007/s13410-017-0600-3
Gao Y, Xiao Y, Miao R et al (2016) The prevalence of mild cognitive impairment with type 2 diabetes mellitus among elderly people in China: a cross-sectional study. Arch Gerontol Geriatr 62:138–142. https://doi.org/10.1016/j.archger.2015.09.003
Gorska-Ciebiada M, Saryusz-Wolska M, Ciebiada M, Loba J (2014) Mild cognitive impairment and depressive symptoms in elderly patients with diabetes prevalence risk factors and comorbidity. J Diabetes Res. https://doi.org/10.1155/2014/179648
Huang R, Tian S, Han J et al (2019) U-shaped association between serum uric acid levels and cognitive functions in patients with type 2 diabetes: a cross-sectional study. J Alzheimer’s Dis : JAD 69(1):135–144. https://doi.org/10.3233/jad-181126
Li W, Sun L, Li G, Xiao S (2019) Prevalence, influence factors and cognitive characteristics of mild cognitive impairment in type 2 diabetes mellitus. Front Aging Neurosci 11:180. https://doi.org/10.3389/fnagi.2019.00180
Liu S, Lu Y, Cai X et al (2019) Glycemic control is related to cognitive dysfunction in elderly people with type 2 diabetes mellitus in a rural chinese population. Curr Alzheimer Res 16(10):950–962. https://doi.org/10.2174/1567205016666191023110712
Xia SS, Xia WL, Huang JJ et al (2020) The factors contributing to cognitive dysfunction in type 2 diabetic patients. Ann Transl Med 8(4):104. https://doi.org/10.21037/atm.2019.12.113
Yang J, Zhang Z, Zhang L et al (2020) Relationship between self-care behavior and cognitive function in hospitalized adult patients with type 2 diabetes: a cross-sectional study. Diabetes, Metab Syndr Obes: Targets Ther 13:207–214. https://doi.org/10.2147/dmso.S236966
Zhang JB, Cong YN, Li ZG, Sun HR, Zhang JS, Wang PF, Wu QZ (2017) Plasma phospholipids are associated with mild cognitive impairment in type 2 diabetic patients. Curr Alzheimer Res 14(6):592–597. https://doi.org/10.2174/1567205013666161201200722
Petersen RC, Roberts RO, Knopman DS et al (2010) Prevalence of mild cognitive impairment is higher in men. The mayo clinic study of aging. Neurology 75(10):889–897. https://doi.org/10.1212/WNL.0b013e3181f11d85
Plassman BL, Langa KM, Fisher GG et al (2008) Prevalence of cognitive impairment without dementia in the United States. Ann Intern Med 148(6):427–434. https://doi.org/10.7326/0003-4819-148-6-200803180-00005
Bartley M, Bokde AL, O’Neill D (2011) Mild cognitive impairment. New Eng J Med 365(14):1357–1358. https://doi.org/10.1056/NEJMc1108238
Kautzky-Willer A, Harreiter J, Pacini G (2016) Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr Rev 37(3):278–316. https://doi.org/10.1210/er.2015-1137
Phillips C (2017) Lifestyle modulators of neuroplasticity: how physical activity, mental engagement, and diet promote cognitive health during aging. Neural Plast 2017:3589271. https://doi.org/10.1155/2017/3589271
Petersen RC, Lopez O, Armstrong MJ et al (2018) Practice guideline update summary: mild cognitive impairment: report of the guideline development, dissemination, and implementation subcommittee of the American academy of neurology. Neurology 90(3):126–135. https://doi.org/10.1212/wnl.0000000000004826
Lee YS (2005) Gender differences in physical activity and walking among older adults. J Women Aging 17(1–2):55–70. https://doi.org/10.1300/J074v17n01_05
Pelimanni E, Jehkonen M (2018) Type 2 diabetes and cognitive functions in middle age a meta-analysis. J Int Neuropsychol Soc 25(2):215–216. https://doi.org/10.1017/s1355617718001042
Ciesielska N, Sokoowski R, Mazur E et al (2016) Is the montreal cognitive assessment (MoCA) test better suited than the mini-mental state examination (MMSE) in mild cognitive impairment (MCI) detection among people aged over 60? Meta-anal Psychiatria polska 50(5):1039–1052. https://doi.org/10.12740/pp/45368
Tombaugh TN, McIntyre NJ (1992) The mini-mental state examination: a comprehensive review. J Am Geriatrics Soc 40(9):922–935. https://doi.org/10.1111/j.1532-5415.1992.tb01992.x
Lam B, Middleton LE, Masellis M et al (2013) Criterion and convergent validity of the Montreal cognitive assessment with screening and standardized neuropsychological testing. J Am Geriatr Soc 61(12):2181–2185. https://doi.org/10.1111/jgs.12541
Alagiakrishnan K, Zhao N, Mereu L, Senior P, Senthilselvan A (2013) Montreal cognitive assessment is superior to standardized mini-mental status exam in detecting mild cognitive impairment in the middle-aged and elderly patients with type 2 diabetes mellitus. BioMed Res Int 2013:186106. https://doi.org/10.1155/2013/186106
Muggeo M (1998) Accelerated complications in Type 2 diabetes mellitus: the need for greater awareness and earlier detection. Diabetic Med: J Br. Diabetic Assoc 15(Suppl 4):S60-62. https://doi.org/10.1002/(sici)1096-9136(1998120)15:4+%3cs60::aid-dia736%3e3.3.co;2-a
Mirahmadizadeh A, Fathalipour M, Mokhtari AM, Zeighami S, Hassanipour S, Heiran A (2020) The prevalence of undiagnosed type 2 diabetes and prediabetes in Eastern Mediterranean region (EMRO): a systematic review and meta-analysis. Diabetes Res Clin Pract 160:107931. https://doi.org/10.1016/j.diabres.2019.107931
Virally M, Blicklé JF, Girard J, Halimi S, Simon D, Guillausseau PJ (2007) Type 2 diabetes mellitus: epidemiology, pathophysiology, unmet needs and therapeutical perspectives. Diab Metabol 33 (4):231–244. https://doi.org/10.1016/j.diabet.2007.07.001
Dankner R, Geulayov G, Olmer L, Kaplan G (2008) Undetected type 2 diabetes in older adults. Age Ageing 38(1):56–62. https://doi.org/10.1093/ageing/afn218
Leahy S, O’ Halloran AM, O’ Leary N, Healy M, McCormack M, Kenny RA, O’ Connell J (2015) Prevalence and correlates of diagnosed and undiagnosed type 2 diabetes mellitus and pre-diabetes in older adults: findings from the Irish Longitudinal Study on Ageing (TILDA). Diab Res Clin Pract 110(3):241–249. https://doi.org/10.1016/j.diabres.2015.10.015
Mendola ND, Chen TC, Gu Q, Eberhardt MS, Saydah S (2018) Prevalence of total, diagnosed, and undiagnosed diabetes among adults: United States, 2013-2016. NCHS Data Brief (319):1–8
Rawlings AM, Sharrett AR, Albert MS, Coresh J, Windham BG, Power MC, Knopman DS, Walker K, Burgard S, Mosley TH, Gottesman RF, Selvin E (2019) The association of late-life diabetes status and hyperglycemia with incident mild cognitive impairment and dementia: the ARIC study. Diab Care 42(7):1248–1254. https://doi.org/10.2337/dc19-0120
Funding
This work was supported by the Key Research and Development Project funded by the Ministry of Science and Technology of the People’s Republic of China (grant number: 2019YFC1710301) and Science and Technology Platform Construction Project of Fujian science and Technology Department(Grant No.2018Y2002)
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by YC, YX, SG, JQ, and JH. The first draft of the manuscript was written by YY and ZL. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to the topical collection Health Education and Psycho-Social Aspects, managed by Massimo Porta and Marina Trento.
Appendices
Appendix: Retrieval strategy
pubmed:
#1 ((((((((((((((Diabetes[Title/Abstract]) OR Diabetes mellitus[Title/Abstract]) OR Diabetes mellitus type 2[Title/Abstract]) OR Diabetes mellitus type II [Title/Abstract]) OR type II Diabetes mellitus[Title/Abstract]) OR type 2 Diabetes mellitus[Title/Abstract]) OR type 2 Diabetes[Title/Abstract]) OR Non-Insulin-Dependent Diabetes Mellitus[Title/Abstract]) OR NIDDM[Title/Abstract]) OR Maturity Onset Diabetes Mellitus[Title/Abstract]) OR Slow-Onset Diabetes Mellitus[Title/Abstract]) OR Adult-Onset Diabetes Mellitus[Title/Abstract]) OR Noninsulin Dependent Diabetes Mellitus[Title/Abstract]) OR Ketosis-Resistant Diabetes Mellitus[Title/Abstract]) OR Maturity Onset Diabetes[Title/Abstract]
#2 ((((((((((Cognitive Dysfunctions[Title/Abstract]) OR Cognitive Impairments[Title/Abstract]) OR Cognitive Impairment[Title/Abstract]) OR Mild Cognitive Impairment[Title/Abstract]) OR Mild Cognitive Impairments[Title/Abstract]) OR Mild Neurocognitive Disorder[Title/Abstract]) OR Mild Neurocognitive Disorders[Title/Abstract]) OR Cognitive Decline[Title/Abstract]) OR Cognitive Declines[Title/Abstract]) OR Mental Deterioration[Title/Abstract]) OR Mental Deteriorations[Title/Abstract]
#3 ((((((((((((Cross Sectional Studies[Title/Abstract]) OR Cross-Sectional Study[Title/Abstract]) OR Cross Sectional Analysis[Title/Abstract]) OR Cross Sectional Analyses[Title/Abstract]) OR Disease Frequency Surveys[Title/Abstract]) OR Cross-Sectional Survey[Title/Abstract]) OR Cross Sectional Survey[Title/Abstract]) OR Cross-Sectional Surveys[Title/Abstract]) OR Disease Frequency Survey[Title/Abstract]) OR Cross-Sectional Analyses[Title/Abstract]) OR Cross-Sectional Analysis[Title/Abstract]) OR Prevalence Studies[Title/Abstract]) OR Prevalence Study[Title/Abstract]
#4:#1+#2+#3
Web of science Core collection
#1 TS=(Diabetes OR Diabetes mellitus OR Diabetes mellitus type 2 OR Diabetes mellitus type OR type Diabetes mellitus OR type 2 Diabetes mellitus OR type 2 Diabetes OR Non-Insulin-Dependent Diabetes Mellitus OR NIDDM OR Maturity Onset Diabetes Mellitus OR Slow-Onset Diabetes Mellitus OR Noninsulin Dependent Diabetes Mellitus OR Maturity Onset Diabetes OR Adult-Onset Diabetes Mellitus OR Ketosis-Resistant Diabetes Mellitus)
#2 TS=(Cognitive Dysfunctions OR Cognitive Impairments OR Cognitive Impairment OR Mild Cognitive Impairment OR Mild Cognitive Impairments OR Mild Neurocognitive Disorder OR Mild Neurocognitive Disorders OR Cognitive Decline OR Cognitive Declines OR Mental Deterioration OR Mental Deteriorations)
#3 TS=: (Cross Sectional Studies OR Cross-Sectional Study OR Cross Sectional Analysis TOPIC Cross Sectional Analyses OR Disease Frequency Surveys OR Cross-Sectional Survey OR Cross Sectional Survey OR Cross-Sectional Surveys OR Disease Frequency Survey OR Cross-Sectional Analyses OR Cross-Sectional Analysis OR Prevalence Studies OR Prevalence Study)
#4:#1+#2+#3
Embase
(Diabetes OR "Diabetes mellitus" OR "Diabetes mellitus type 2" OR "Diabetes mellitus type II" OR "type II Diabetes mellitus" OR "type 2 Diabetes mellitus" OR "type 2 Diabetes" OR "Non-Insulin-Dependent Diabetes Mellitus" OR NIDDM OR "Maturity Onset Diabetes Mellitus" OR "Slow-Onset Diabetes Mellitus" OR "Noninsulin Dependent Diabetes Mellitus" OR "Maturity Onset Diabetes" OR "Adult-Onset Diabetes Mellitus" OR "Ketosis-Resistant Diabetes Mellitus"):ab,ti AND ("Cognitive Dysfunctions" OR "Cognitive Impairments" OR "Cognitive Impairment" OR "Mild Cognitive Impairment" OR "Mild Cognitive Impairments" OR "Mild Neurocognitive Disorder" OR "Mild Neurocognitive Disorders" OR "Cognitive Decline" OR "Cognitive Declines" OR "Mental Deterioration" OR "Mental Deteriorations"):ab,ti AND ("Cross Sectional Studies" OR "Cross-Sectional Study" OR "Cross Sectional Analysis" OR "Cross Sectional Analyses" OR "Disease Frequency Surveys" OR "Cross-Sectional Survey" OR "Cross Sectional Survey" OR "Cross-Sectional Surveys" OR "Disease Frequency Survey" OR "Cross-Sectional Analyses" OR "Cross-Sectional Analysis" OR "Prevalence Studies" OR "Prevalence Study"):ab,ti
Limits including "human", "embase database"
(diabetes:ab,ti OR 'diabetes mellitus':ab,ti OR 'diabetes mellitus type 2':ab,ti OR 'diabetes mellitus type II ':ab,ti OR 'type II diabetes mellitus':ab,ti OR 'type 2 diabetes mellitus':ab,ti OR 'type 2 diabetes':ab,ti OR 'non-insulin-dependent diabetes mellitus':ab,ti OR niddm:ab,ti OR 'maturity onset diabetes mellitus':ab,ti OR 'slow-onset diabetes mellitus':ab,ti OR 'noninsulin dependent diabetes mellitus':ab,ti OR 'maturity onset diabetes':ab,ti OR 'adult-onset diabetes mellitus':ab,ti OR 'ketosis-resistant diabetes mellitus':ab,ti) AND ('cognitive dysfunctions':ab,ti OR 'cognitive impairments':ab,ti OR 'cognitive impairment':ab,ti OR 'mild cognitive impairment':ab,ti OR 'mild cognitive impairments':ab,ti OR 'mild neurocognitive disorder':ab,ti OR 'mild neurocognitive disorders':ab,ti OR 'cognitive decline':ab,ti OR 'cognitive declines':ab,ti OR 'mental deterioration':ab,ti OR 'mental deteriorations':ab,ti) AND ('cross sectional studies':ab,ti OR 'cross-sectional study':ab,ti OR 'cross sectional analysis':ab,ti OR 'cross sectional analyses':ab,ti OR 'disease frequency surveys':ab,ti OR 'cross-sectional survey':ab,ti OR 'cross sectional survey':ab,ti OR 'cross-sectional surveys':ab,ti OR 'disease frequency survey':ab,ti OR 'cross-sectional analyses':ab,ti OR 'cross-sectional analysis':ab,ti OR 'prevalence studies':ab,ti OR 'prevalence study':ab,ti) AND [humans]/lim AND [embase]/lim
Rights and permissions
About this article
Cite this article
You, Y., Liu, Z., Chen, Y. et al. The prevalence of mild cognitive impairment in type 2 diabetes mellitus patients: a systematic review and meta-analysis. Acta Diabetol 58, 671–685 (2021). https://doi.org/10.1007/s00592-020-01648-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-020-01648-9