Abstract
Aim
Main failure of diabetic tractional retinal detachment (TRD) surgery is the development of proliferative vitreoretinopathy (PVR), causing higher re-detachment rates. We investigated whether the use of dexamethasone (DEX) implant at the end of pars plana vitrectomy (PPV) with silicone oil tamponade might have an impact on these outcomes.
Design
Comparative, nonrandomized, retrospective study.
Participants
A total of 148 eyes from 148 patients that underwent PPV with silicone oil tamponade for diabetic TRD (with DEX implant, n = 52; without DEX implant, n = 96).
Methods
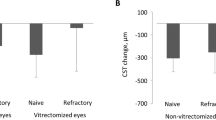
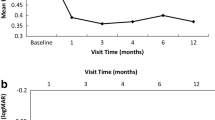
Consecutive patients’ records were reviewed for time between TRD diagnosis and surgery; lens status before surgery and after 6, 12, and 24 months; retina attachment rate after primary PPV; change in postoperative PVR severity; rate of re-detachment at 6, 12, and 24 months; use of IOP lowering treatment after 6, 12, and 24 months; surgery details; intra- and postoperative complications. Correlations between outcome measures, postoperative PVR severity, and re-detachment rates were analyzed.
Main outcome measures
Change in postoperative PVR severity and retinal re-detachment rates with and without the adjuvant use of DEX implant.
Results
Retinal re-detachment rates were significantly higher in the group of patients that did not receive DEX implant [11/96 (11.5%) vs. 0/52 (0%), p = 0.049; 11/84 (12.9%) vs. 4/52 (7.7%), p = 0.007; 14/71 (19.7%) vs. 5/52 (10%) p < 0.001 at 6, 12, and 24 months, respectively]. PVR severity correlated with retinal status at 12 and 24 months (p = 0.018 and p = 0.027, respectively). The difference in PVR severity between the two groups was statistically significant at 6, 12, and 24 months (p < 0.001).
Conclusions
DEX implant at the end of PPV in patients with diabetic TRD improves PVR severity and decreases re-detachment rates. This should be considered as an option in the customized treatment of TRD.

Similar content being viewed by others
References
Guariguata L, Whiting DR, Hambleton I et al (2014) Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 103:137–149
Antonetti DA, Klein R, Gardner TW (2015) Diabetic retinopathy. Med (Baltim) 43:13–19
Sternfeld A, Axer-Siegel R, Stiebel-Kalish H et al (2015) Advantages of diabetic tractional retinal detachment repair. Clin Ophthalmol 9:1989–1994
Dikopf MS, Patel KH, Setlur VJ, Lim JI (2015) Surgical outcomes of 25-gauge pars plana vitrectomy for diabetic tractional retinal detachment. Eye 29:1213–1219
Storey PP, Ter-Zakarian A, Philander SA et al (2017) Visual and anatomical outcomes after diabetic traction and traction-rhegmatogenous retinal detachment repair. Retina 38:1913–1919
Shroff CM, Gupta C, Shroff D et al (2018) Bimanual microincision vitreous surgery for severe proliferative diabetic retinopathy: outcome in more than 300 eyes. Retina 38:S134–S145
El Rami H, Barham R, Sun JK, Silva PS (2017) Evidence-based treatment of diabetic retinopathy. Semin Ophthalmol 32:67–74
Aiello LP, Avery RL, Arrigg PG et al (1994) Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med 331:1480–1487
Vujosevic S, Simó R (2017) Local and systemic inflammatory biomarkers of diabetic retinopathy: an integrative approach. Invest Ophthalmol Vis Sci 58:68–75. https://doi.org/10.1167/iovs.17
Funatsu H, Yamashita H, Noma H et al (2005) Aqueous humor levels of cytokines are related to vitreous levels and progression of diabetic retinopathy in diabetic patients. Graefe’s Arch Clin Exp Ophthalmol 243:3–8
Schwartzman ML, Iserovich P, Gotlinger K et al (2010) Profile of lipid and protein autacoids in diabetic vitreous correlates with the progression of diabetic retinopathy. Diabetes 59:1780–1788. https://doi.org/10.2337/db10-0110
Goldberg RB (2009) Cytokine and cytokine-like inflammation markers, endothelial dysfunction, and imbalanced coagulation in development of diabetes and its complications. J Clin Endocrinol Metab 94:3171–3182
dell’Omo R, Semeraro F, Bamonte G et al (2013) Vitreous mediators in retinal hypoxic diseases. Mediat Inflamm 2013:935301
Tang J, Kern TS (2011) Inflammation in diabetic retinopathy. Prog Retin Eye Res 30:343–358
Iglicki M, Zur D, Busch C et al (2018) Progression of diabetic retinopathy severity after treatment with dexamethasone implant: a 24-month cohort study the ‘DR-Pro-DEX Study’. Acta Diabetol. https://doi.org/10.1007/s00592-018-1117-z
Moon SW, Sun Y, Warther D et al (2018) New model of proliferative vitreoretinopathy in rabbit for drug delivery and pharmacodynamic studies. Drug Deliv 25:600–610. https://doi.org/10.1080/10717544.2018.1440664
Hilton G, Machemer R, Michels R, Okun E, Schepens C, Schwartz A (1983) The classification of retinal detachment with proliferative vitreoretinopathy. Ophthalmology 90:121–125
Deuchler S, Ackermann H, Singh P et al (2017) Key factors to improve the outcome of retinal reattachment surgery in proliferative vitreoretinopathy and proliferative diabetic retinopathy. J Ophthalmol. https://doi.org/10.1155/2017/2323897
Goezinne F, La Heij EC, Berendschot TTJM et al (2007) Risk factors for redetachment and worse visual outcome after silicone oil removal in eyes with complicated retinal detachment. Eur J Ophthalmol 17:627–637
Scott IU, Flynn HW, Murray TG et al (2005) Outcomes of complex retinal detachment repair using 1000- vs 5000-centistoke silicone oil. Arch Ophthalmol 123:473–478. https://doi.org/10.1001/archopht.123.4.473
Soheilian M, Mazareei M, Mohammadpour M, Rahmani B (2006) Comparison of silicon oil removal with various viscosities after complex retinal detachment surgery. BMC Ophthalmol 6:1–6. https://doi.org/10.1186/1471-2415-6-21
Altan T, Acar N, Kapran Z et al (2008) Transconjunctival 25-gauge sutureless vitrectomy and silicone oil injection in diabetic tractional retinal detachment. Retina 28:1201–1206
Hou H, Huffman K, Rios S et al (2015) A novel approach of daunorubicin application on formation of proliferative retinopathy using a porous silicon controlled delivery system: pharmacodynamics. Invest Ophthalmol Vis Sci 56:2755–2763
Schaub F, Hoerster R, Schiller P et al (2018) Prophylactic intravitreal 5-fluorouracil and heparin to prevent proliferative vitreoretinopathy in high-risk patients with retinal detachment: study protocol for a randomized controlled trial. Trials 19:384
London NJS, Kaiser RS, Khan MA et al (2018) Determining the effect of low-dose isotretinoin on proliferative vitreoretinopathy: the DELIVER trial. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2018-312839
Kaneko H, Terasaki H (2017) Biological Involvement of microRNAs in proliferative vitreoretinopathy. Transl Vis Sci Technol 6:5
Bhaskaranand M, Ramachandra C, Bhat S et al (2016) Automated diabetic retinopathy screening and monitoring using retinal fundus image analysis. J Diabetes Sci Technol 10:254–261. https://doi.org/10.1177/1932296816628546
Banerjee PJ, Quartilho A, Bunce C et al (2017) Slow-release dexamethasone in proliferative vitreoretinopathy: a prospective, randomized controlled clinical trial. Ophthalmology 124:757–767
Moysidis SN, Thanos A, Vavvas DG (2012) Mechanisms of inflammation in proliferative vitreoretinopathy: from bench to bedside. Mediat Inflamm 2012:815937
Pastor JC, Rojas J, Pastor-Idoate S et al (2016) Proliferative vitreoretinopathy: a new concept of disease pathogenesis and practical consequences. Prog Retin Eye Res 51:125–155
Chen W, Chen H, Hou P et al (2011) Midterm results of low-dose intravitreal triamcinolone as adjunctive treatment for proliferative vitreoretinopathy. Retina 31:1137–1142
Cheema RA, Peyman GA, Fang T et al (2007) Triamcinolone acetonide as an adjuvant in the surgical treatment of retinal detachment with proliferative vitreoretinopathy. Ophthalmic Surg Lasers Imaging 38:365–370
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
The study was approved by the Tel Aviv Sourasky Medical Center Institutional Review Board (Helsinki Committee), nr. 0745-18-TLV.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Managed by Massimo Porta.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Iglicki, M., Zur, D., Fung, A. et al. TRActional DIabetic reTInal detachment surgery with co-adjuvant intravitreal dexamethasONe implant: the TRADITION STUDY. Acta Diabetol 56, 1141–1147 (2019). https://doi.org/10.1007/s00592-019-01357-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-019-01357-y