Abstract
Purpose
Early diagnosis and treatment of scaphoid fractures is critical to achieve union and prevent wrist degenerative arthritis. Plain radiographic measurements can guide the early approach to suspected fractures. Specifically, the ability to predict fracture or fracture stability from plain radiographs may allow the traumatologist to expand initial referral to three-dimensional imaging. We evaluated the ability of four measured angles to predict presence of a scaphoid fracture and stability.
Methods
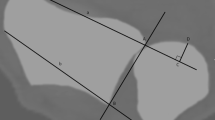
Fifty patients with a scaphoid fracture and 50 patients without fracture were evaluated for the cortical ring sign, scapho-lunate gapping, lateral scapholunate (SL), radio-scaphoid (RS), radio-lunate (RL), and radio-capitate (RC) angles by two-blinded observers.
Results
Measurement of an increased SL interval was associated with the presence of a scaphoid fracture as diagnosed on three-dimensional imaging [odds ratio (OR) 3.0, confidence interval (CI) 1.53–5.87, p = < 0.01]. The measured RL angle was associated with fracture displacement (OR 1.13, 95% CI 1.02–1.25, p = 0.02).
Conclusions
Scapholunate gapping on plain radiographs in the context of a clinically suspected scaphoid fracture should increase suspicion for a fracture and may prompt earlier 3-dimensional imaging, while the presence of an abnormal radiolunate angle should increase wariness for instability and can be used in preoperative planning.



Similar content being viewed by others
References
Garala K, Taub NA, Dias JJ (2016) The epidemiology of fractures of the scaphoid: impact of age, gender, deprivation and seasonality. Bone Joint J 98-B(5):654–659. https://doi.org/10.1302/0301-620X.98B5.36938
Bain GI, Bennett JD, MacDermid JC, Slethaug GP, Richards RS, Roth JH (1998) Measurement of the scaphoid humpback deformity using longitudinal computed tomography: intra- and interobserver variability using various measurement techniques. J Hand Surg Am 23(1):76–81. https://doi.org/10.1016/S0363-5023(98)80093-2
Toms AP, Chojnowski A, Cahir JG (2011) Midcarpal instability: a radiological perspective. Skeletal Radiol 40(5):533–541. https://doi.org/10.1007/s00256-010-0941-1
Kani KK, Mulcahy H, Chew FS (2016) Understanding carpal instability: a radiographic perspective. Skeletal Radiol 45(8):1031–1043. https://doi.org/10.1007/s00256-016-2390-y
Pirela-Cruz MA, Hilton ME, Faillace J (2003) Frequency and characteristics of the scaphoid cortical ring sign. Surg Radiol Anat 25(5–6):451–454. https://doi.org/10.1007/s00276-003-0165-3
Abe Y, Doi K, Hattori Y (2008) The clinical significance of the scaphoid cortical ring sign: a study of normal wrist X-rays. J Hand Surg Eur 33(2):126–129. https://doi.org/10.1177/1753193407087572
MacDermid JC, McClure JA, Richard L, Faber KJ, Jaglal S (2021) Fracture profiles of a 4-year cohort of 266,324 first incident upper extremity fractures from population health data in Ontario. BMC Musculoskelet Disord 22(1):996. https://doi.org/10.1186/s12891-021-04849-7
Shah CM, Stern PJ (2013) Scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) wrist arthritis. Curr Rev Musculoskelet Med 6(1):9–17. https://doi.org/10.1007/s12178-012-9149-4
Schormans PMJ, Brink PRG, Poeze M, Hannemann PFW (2018) Angular stable miniplate fixation of chronic unstable scaphoid nonunion. J Wrist Surg 7(1):24–30. https://doi.org/10.1055/s-0037-1603202
Sander AL, Sommer K, Schaf D, Braun C, Marzi I, Pohlemann T, Frank J (2018) Clinical outcome after alternative treatment of scaphoid fractures and nonunions. Eur J Trauma Emerg Surg 44(1):113–118. https://doi.org/10.1007/s00068-017-0773-y
Mandaleson A, Tham SK, Lewis C, Ackland DC, Ek ET (2018) Scaphoid fracture fixation in a nonunion model: a biomechanical study comparing 3 types of fixation. J Hand Surg Am 43(3):221–228. https://doi.org/10.1016/j.jhsa.2017.10.005
Megerle K, Pohlmann S, Kloeters O, Germann G, Sauerbier M (2011) The significance of conventional radiographic parameters in the diagnosis of scapholunate ligament lesions. Eur Radiol 21(1):176–181. https://doi.org/10.1007/s00330-010-1910-8
Said J, Baker K, Fernandez L, Komatsu DE, Gould E, Hurst LC (2018) The optimal location to measure scapholunate diastasis on screening radiographs. Hand (N Y) 13(6):671–677. https://doi.org/10.1177/1558944717729219
Black DM, Watson HK, Vender MI (1987) Scapholunate gap with scaphoid nonunion. Clin Orthop Relat Res 224:205–209
Cooney WP, Linscheid RL, Dobyns JH, Wood MB (1988) Scaphoid nonunion: role of anterior interpositional bone grafts. J Hand Surg Am 13(5):635–650. https://doi.org/10.1016/s0363-5023(88)80116-3
Schadel-Hopfner M, Junge A, Bohringer G (2005) Scapholunate ligament injury occurring with scaphoid fracture–A rare coincidence? J Hand Surg Br 30(2):137–142. https://doi.org/10.1016/j.jhsb.2004.09.017
Garcia-Elias M, An KN, Amadio PC, Cooney WP, Linscheid RL (1989) Reliability of carpal angle determinations. J Hand Surg Am 14(6):1017–1021. https://doi.org/10.1016/s0363-5023(89)80053-x
Sahu A, Kuek DK, MacCormick A, Gozzard C, Ninan T, Fullilove S, Suresh P (2021) Prospective comparison of magnetic resonance imaging and computed tomography in diagnosing occult scaphoid fractures. Acta Radiol. https://doi.org/10.1177/02841851211064595
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare.
Human and animal rights
All human and animal studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Becker, J., Luria, S., Huang, S. et al. Wrist angle measurements in predicting the presence of a displaced scaphoid fracture. Eur J Orthop Surg Traumatol 33, 2271–2276 (2023). https://doi.org/10.1007/s00590-022-03418-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-022-03418-5