Abstract
Background
Combined ipsilateral femoral neck and shaft fractures are rare and present a challenging management dilemma. This study aims to assess the outcome of concomitant fixation of the ipsilateral femoral neck and shaft fracture using single versus dual surgical implants.
Methods
A single-center retrospective analysis of patients who underwent fixation of ipsilateral femoral neck and shaft fractures was performed over a 13-year period. Different techniques were employed to fix the complex injury. Both the reduction and the union time were assessed radiographically.
Results
A total of 36 patients with ipsilateral femoral neck and shaft fractures were retrospectively identified and included in the study. Twenty-four patients (66.6%) were managed with a single cephalomedullary nail, while the remaining cases were treated with two devices. All cases were operated on within an average of 3.7 ± 7.1 days. Eight patients (22.2%) developed postoperative complications. The average follow-up period was 7.3 ± 6.8 months. Although there was no statistically significant difference between the two groups, the femoral neck fractures showed shorter union time in patients treated with one implant compared to patients treated with two implants (3.0 ± 2.3 months vs. 4.2 ± 2.6 months). Another observation was that higher percentages of implant removal/failure and malunion/nonunion were seen in patients who had one implant compared to the two implants group (12.5% vs. 8.3%).
Conclusion
Early surgical fixation of both fractures is associated with good outcome results. No difference in outcome was observed between both groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Combined ipsilateral femoral neck and shaft fractures are rare and present a challenging management dilemma. The incidence ranges between three and ten percent [1] and usually occurs due to high energy trauma. The diagnosis of associated neck fracture can be missed easily or delayed, in up to one-third of the cases [2, 3], and therefore, it is essential to perform a thorough evaluation of polytrauma patients with diaphyseal femoral fracture[4,5,6]. Currently with the improvement of trauma care and increased survival rate of polytrauma patients, the incidence is more likely to increase.
The mechanism of injury usually involves axial compression against the acetabulum, with concomitant adduction or abduction of the hip [7]. The femoral shaft fracture usually is more comminuted as it absorbs most of the energy, while the neck usually sustains less displacement [2]. Regarding the ideal management strategy, there has been a lot of controversy about the optimal fixation technique of these combined injuries. The increased risk of avascular necrosis with delayed fixation of the femoral neck has driven surgeons to prioritize early anatomical fixation of the neck fracture [8]. Whether this was achieved using a single versus dual implants is still controversial. This study aimed to assess the outcome of concomitant fixation of the ipsilateral femoral neck and shaft fracture using single versus dual surgical implants.
Methods
Data acquisition
This study has been reported in line with strengthening the reporting of observational studies in epidemiology (STROBE) guidelines [9]. After receiving institutional review board approval with a waiver of consent, during the period from January 2008 and August 2020, all cases who underwent femoral shaft fixation in a single-level 1 trauma center were reviewed. Out of 1861 cases, 36 cases of concomitant ipsilateral femoral neck and shaft fractures were identified and included in the study. The inclusion criteria were patients > 17 who underwent surgical fixation of ipsilateral femoral shaft and neck fractures with at least 6 months of follow-up.
Demographic and surgical characteristics were reviewed and included patients’ age, gender, mechanism of injury, location of femoral neck fracture (basicervical or transcervical), displacement of femoral neck fracture classified as nondisplaced (Garden classification grade one and two) or displaced (Garden classification grade three and four), location of femoral shaft fracture (proximal, midshaft or distal), other associated injuries, time to surgery, surgical positioning, methods of reduction, number of implants used, postoperative complications, postoperative union time, implant removal/failure, malunion/nonunion and duration of follow-up. The decision whether to fix the fractures using one or two implants was made by the primary surgeon. Several factors affected the selection process, including the patient’s general condition, the amount of displacement of a neck fracture and the surgeon’s preference.
The primary outcome was fracture radiographic union defined by evidence of bridging callus on three out of four cortices on anteroposterior and lateral radiographs. The secondary outcome is the accuracy of reduction which was evaluated for both femoral neck and shaft fractures. The reduction of femoral neck fracture was assessed radiographically based on two parameters according to Haidukewych et al. [10]: the degree of residual angulation and the amount of displacement (cortex apposition regardless of direction). Excellent reduction was defined as < two mm of displacement and < five degrees of angulation in any plane, good as two to five mm displacement and/or five to ten degrees of angulation, fair as > five to ten mm of displacement and/or > 10–20° of angulation and poor as > 10 mm of displacement and/or > 20° of angulation. Similarly, femoral shaft malreduction was defined as > 5° of angulation in the coronal plane or > 10° of angulation in the sagittal plane [11]. In addition, implant failure was defined as femoral neck screws cut out, breakage of nail or breakage of proximal or distal locking screws. All radiographs were reviewed using the picture archiving and communication system (PACS) by one orthopedic surgery resident and a trauma fellowship trained orthopedic surgeon, and any conflict was resolved by the senior author (G.A.)
Statistical analysis
Continuous variables were reported as a mean ± SD and categorical variables as frequency (%). A p-value of ≤ 0.05 was considered statistically significant. Comparison between one implant group and two implants group was done using an independent t test. The rate of complications and union rate between one implant versus two implants were analyzed using Mann–Whitney U test. Data were analyzed using SPSS version 11.0 statistic software package.
Results
A total of 36 cases of ipsilateral femoral neck and shaft fractures were retrospectively identified and included in the study (Table 1). In our sample, the mean age was 37.5 ± 11.1 years, with males representing most of the cases (83.3%). The mechanism of injury was fall from height in 30 cases (83.3%), while 6 cases (16.7%) had fractures secondary to motor vehicle collisions. Among the studied cases, one patient had bilateral neck and shaft fractures, while the rest sustained unilateral injuries. Twenty-nine patients (80.6%) sustained other associated musculoskeletal, head, chest and abdominal injuries. All cases were operated on within an average of 3.7 ± 7.1 days.
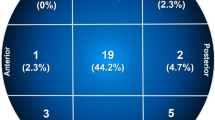
The fracture characteristics of our cohort are summarized in Table 2. Femoral neck fractures were basicervical in 17 cases (47.2%) and transcervical in 19 cases (52.8%). Displacement was found in 14 cases of neck fractures (38.9%), while the remaining 22 (61.1%) were either Garden’s grade I or II. The mean Pauwels’s angle was 65.8 ± 14.8 degrees. Regarding the shaft fractures, they were located in the midshaft in the majority of the cases (77.8%). The average neck-shaft angle was 128.6 ± 5.2 degrees.
Different techniques were used to fix the concomitant ipsilateral femoral neck and shaft fractures (Fig. 1). Twenty-four patients (66.6%) were managed with a single cephalomedullary nail (CMN). The remaining cases were treated with two devices (seven patients received retrograde nailing and cannulated screws, two patients had antegrade nailing and cannulated screws, two patients had a sliding hip screw and retrograde nailing, and one patient had plate fixation and cannulated screws). Although there was no statistically significant difference between the two groups, all patients fixed with two devices had either good or excellent femoral neck reduction, while good or excellent reduction of neck fracture was noted in 84.7% of patients managed with one device. Femoral shaft malreduction was observed in three patients treated by one implant method and only one patient from the two devices group.
Different surgical techniques for the management of ipsilateral femoral neck and shaft fractures. A Antegrade femoral nailing with cancellous screws placed around the nail for the neck fracture. B Plate fixation of the diaphyseal fracture with cancellous screw. C Retrograde nailing with dynamic hip screw. D Retrograde nailing with cannulated screws. E Cephalomedullary nail
Upon comparing the patients who were fixed with one implant (N = 24) versus two implants (N = 12), none of our prognostic factors showed statistical significance (Table 3). However, the femoral neck fractures showed a shorter union time in patients treated with one implant compared to patients treated with two implants (3.0 ± 2.3 months vs. 4.2 ± 2.6 months). Another observation was that higher percentages of implant removal/failure and malunion/nonunion were seen in patients who had one implant compared to the two implants group (12.5% vs. 8.3%).
Eight patients (22.2%) developed postoperative complications. In the single device group, one case developed wound infection, three cases developed nonunion, and three cases developed malunion. Only one case from the dual devices group developed malunion. The average follow-up period was 7.3 ± 6.8 months.
Discussion
In this retrospective analysis of 36 cases of ipsilateral femoral neck and shaft fractures, no difference in the radiological outcomes and complications for patients treated with single versus dual construct was reported. Although higher rate of excellent reduction of both the femoral neck and shaft was found in the two device group, this did not reach statistical significant. On the other hand, single construct fixation showed and average 1.2 months faster time to union when compared to dual construct fixation with no statistical significance. Our results were consistent with the available literature with no solid conclusions can be made on the optimal construct for these injuries. We believe that the treatment plan should be tailored for each case depending mainly on the femoral neck fracture displacement and the surgeon’s’ experience with the available implants.
Mohapatra et al. reported satisfactory results using both single versus dual constructs in 18 cases of ipsilateral femoral neck and shaft fractures [1]. Similarly, Wei et al. reported no significant difference in fractures reduction or complications in 22 patients treated with single versus dual implants [12].
The complexity of ipsilateral femoral neck and shaft fractures mandates careful preoperative planning on an individual basis. Both fractures should be treated with an implant(s) that optimizes fracture healing while simultaneously prioritizing the femoral neck fracture to avoid avascular necrosis [1, 4, 6, 13]. In one of the largest series on the topic, Oh et al. reported on 74 cases of ipsilateral femoral neck and shaft fractures. The rate of avascular necrosis was 6.8% with higher risk with displaced femoral neck fractures. The authors also reported a high rate of femoral shaft nonunion of 20% [14]. Although Hung et al. [15] reported that the order of fixation of the fractures may not be important, others gave priority to fixation of the femoral neck fractures first especially if displaced. Some authors even support fixing the femoral shaft fracture first as it will aid in the fixation of the femoral neck [16,17,18]. Recently, The American Academy of Orthopedic Surgeons published an article in which they described a preferred approach to guide surgeons in fixing ipsilateral femoral neck and shaft fractures [16]. If the femoral neck fracture was displaced, it is preferred to use two implants to fix the fractures starting with fixing the neck of femur. Regarding femoral shaft fracture, after fixation, surgeons should take radiographs of the contralateral side to evaluate for length, alignment and malreduction. If there is no obvious neck of femur fracture preoperatively, an intraoperative fluoroscopic examination should be done to assess for fracture. Prophylactic measures should be taken if there is no femur neck fracture.
Multiple surgical fixation techniques are used based on patients’ factors, fracture characteristics and surgeon preference, with controversial clinical outcomes reported in the literature. Treatment options include single constructs (e.g. CMN, long sliding hip screw) and dual constructs (e.g. retrograde nail with sliding hip screw, proximal femoral locking plate or cannulated screws) [16]. While each has its own merits and demerits, the goal of any treatment plan should be an anatomic reduction of neck fracture and stable fixation of both fractures so patients can be early mobilized [19].
The CMN is a one implant option used to fix both fractures. The advantages of CMN include using a single incision to fix both fractures and saving the bony stock for the insertion of proximal screws for hip fractures [7]. In addition, the infection rate and blood loss can be reduced with the closed reduction technique. The CMN is known to be a load-sharing device that allows early rehabilitation postoperatively [7]. This construct, however, is technically demanding and associated with high malreduction rates [11, 20]. Bedi et al. found a statistically significant higher rate of malreduction of either femoral neck or shaft fracture when CMN is used to address both fractures simultaneously. They advised using two implants rather than one to avoid malreduction [11]. The most important finding of the current study is that there was no statistically significant difference between the two groups regarding fracture union, the accuracy of reduction and implant failure.
Limitations
This study is limited by its retrospective nature, single-site perspective, small cohort due to the rarity of the injury and the short-term follow-up period. Although we assessed the radiological outcomes postoperatively, the functional outcomes could not be assessed due to incomplete data available for analysis. In addition, our results may not be generalized to other practice settings due to the different surgeons’ preferences and various surgical implants available.
Conclusions
Ipsilateral femoral neck and shaft fractures are rare high-energy trauma that required a high level of suspicion and planned early management. Early surgical fixation of both fractures was associated with good outcome results. Single versus dual implant fixation was not found to significantly affect the radiological outcomes or complications. High-level multicenter studies with long-term follow-up would be needed to further investigate the optimal management of such injuries.
Data availability
Data available on request from the authors.
Code availability
Not applicable.
Change history
15 October 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00590-022-03411-y
References
Mohapatra G, Sethy RR (2017) Ipsilateral fracture neck and shaft of femur: a prospective analysis of two methods. J Orthop Traumatol Rehabil 9:17–20. https://doi.org/10.4103/jotr.jotr_16_16
Daine OC (2017) Ipsilateral femoral neck and shaft fractures. Ortho Rheum Open Access 5(3):555661. https://doi.org/10.19080/OROAJ.2017.05.555661
Hak DJ, Mauffrey C, Hake M, Hammerberg EM, Stahel PF (2015) Ipsilateral femoral neck and shaft fractures: current diagnostic and treatment strategies. Orthopedics 38(4):247–251. https://doi.org/10.3928/01477447-20150402-05
Tornetta P 3rd, Kain MS, Creevy WR (2007) Diagnosis of femoral neck fractures in patients with a femoral shaft fracture. Improvement with a standard protocol. J Bone Joint Surg 89(1):39–43. https://doi.org/10.2106/JBJS.F.00297
Wolinsky PR, Johnson KD (1995) Ipsilateral femoral neck and shaft fractures. Clin Orthop Relat Res 318:81–90
Riemer BL et al (1993) Clandestine femoral neck fractures with ipsilateral diaphyseal fractures. J Orthop Trauma 7(5):443–449. https://doi.org/10.1097/00005131-199310000-00007
Sengodan VC et al (2015) Management of ipsilateral fracture of hip and shaft of femur. IJCRR 7(17):7
Barei DP et al (2003) Noncontiguous fractures of the femoral neck, femoral shaft, and distal femur. J Trauma 55(1):80–86. https://doi.org/10.1097/01.TA.0000046259.43886.25
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative STROBE (2008) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61(4):344–349. https://doi.org/10.1016/j.jclinepi.2007.11.008
Haidukewych GJ, Rothwell WS, Jacofsky DJ, Torchia ME, Berry DJ (2004) Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J Bone Joint Surg 86(8):1711–1716
Bedi A, Karunakar MA, Caron T, Sanders RW, Haidukewych GJ (2009) Accuracy of reduction of ipsilateral femoral neck and shaft fractures–an analysis of various internal fixation strategies. J Orthop Trauma 23(4):249–253
Wei YP, Lin KC (2021) Dual-construct fixation is recommended in ipsilateral femoral neck fractures with infra-isthmus shaft fracture: A STROBE compliant study: a STROBE compliant study. Medicine (Baltimore) 100(17):e25708. https://doi.org/10.1097/MD.0000000000025708
Reikerås O, Høiseth A (1982) Femoral neck angles in osteoarthritis of the hip. Acta Orthop Scand 53(5):781–784. https://doi.org/10.3109/17453678208992292
Oh C-W, Kim J-W, Park KC, Apivatthakakul T, Luo C-F, Wong MK et al (2022) Clinical outcomes and affecting factors of ipsilateral femoral neck and shaft fractures - Multination, multicenter analysis. J Orthop Sci. https://doi.org/10.1016/j.jos.2021.12.021
Hung S-H et al (2004) Surgical treatment for ipsilateral fractures of the hip and femoral shaft. Injury 35(2):165–169. https://doi.org/10.1016/s0020-1383(03)00278-x
Jones CB, Walker JB (2018) Diagnosis and management of ipsilateral femoral neck and shaft fractures. J Am Acad Orthop Surg 26(21):e448–e454. https://doi.org/10.5435/jaaos-d-17-00497
Swiontkowski MF et al (1984) Ipsilateral fractures of the femoral neck and shaft. A treatment protocol. J Bone Joint Surg 66(2):260
James P, Waddell (2011) Fractures of the proximal femur: improving outcomes, pp 91–96
Alho A, Ekeland A, Grøgaard B, Dokke JR (1996) A locked hip screw-intramedullary nail (cephalomedullary nail) for the treatment of fractures of the proximal part of the femur combined with fractures of the femoral shaft. J Trauma 40(1):10–16. https://doi.org/10.1097/00005373-199601000-00003
Singh R, Rohilla R, Magu NK, Siwach R, Kadian V, Sangwan SS (2008) Ipsilateral femoral neck and shaft fractures: a retrospective analysis of two treatment methods. J Orthop Traumatol: Off J Ital Soc Orthop Traumatol 9(3):141–147. https://doi.org/10.1007/s10195-008-0025-3
Funding
Open Access funding provided by the Qatar National Library.
Author information
Authors and Affiliations
Contributions
Yahya Alborno contributed to data collection, analysis, and writing the initial and the final version of the manuscript. Abdullah Abunimer and Motasem Salameh contributed to the final version of the manuscript. Yousef Abuodeh contributed to data analysis. Hammam Kayali contributed to editing of the final version of the manuscript. Ghalib Ahmed supervised the project.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Our local research council approved the study.
Informed consent
Not needed as this is retrospective study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alborno, Y., Abunimer, A., Abuodeh, Y. et al. The surgical outcomes of fixing ipsilateral femoral neck and shaft fractures: single versus double implants fixation. Eur J Orthop Surg Traumatol 33, 1613–1618 (2023). https://doi.org/10.1007/s00590-022-03312-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-022-03312-0