Abstract
Background
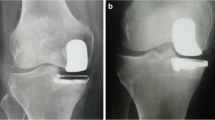
All-polyethylene tibias (APT) are under-utilized in most of the Western countries, due to a shift from the original all-polyethylene design to metal-backed tibia (MBT) components. Only few total knee prostheses allow direct comparison between APT and MBT components, due to different geometric designs in many systems. The Depuy PFC Sigma prostheses have a similar geometric design in both the MBT and the APT, and with the same corresponding femoral component, thus allowing an assessment and comparison between APT and MBT components.
Methods
This is a retrospective analysis of a consecutive series of osteoarthritic patients who underwent total knee arthroplasties with at least 10-year follow-up comparing a modern congruent APT component to a modular MBT component of the same design.
Results
Seventy-three patients (81 knees, mean age 73 years) were available for assessment. Among the cohort, three patients had revision surgery (one from the APT group). In total, 73 patients were available for follow-up (59 MBT prostheses and 22 APT prostheses). There were no differences in knee function (Knee Society score, range of motion, stability) or radiographic parameters between the groups. Of the three revisions due to tibial tray loosening, only one was performed in the APT group and two were performed in the MBT group; another revision in the MBT group was due to loosening of both components; none of the revisions were due to septic complications. Ten-year survivorship of both designs was 92 %.
Conclusions
While function of both designs appears similar, the APT design shows a trend toward requiring fewer revisions and is more cost-effective.

Similar content being viewed by others
References
Muller SD, Deehan DJ, Holland JP, Outterside SE, Kirk LM, Gregg PJ et al (2006) Should we reconsider all-polyethylene tibial implants in total knee replacement? J Bone Joint Surg Br 88:1596–1602
Cuckler JM, Lemons J, Tamarapalli JR, Beck P (2003) Polyethylene damage on the nonarticular surface of modular total knee prostheses. Clin Orthop Relat Res 410:248–253
Edwards SA, Pandit HG, Ramos JL, Grover ML (2002) Analysis of polyethylene thickness of tibial components in total knee replacement. J Bone Joint Surg Am 84(3):369–371
Adalberth G, Nilsson KG, Bystrom S, Kolstad K, Milbrink J (2000) Low-conforming all-polyethylene tibial component not inferior to metal-backed component in cemented total knee arthroplasty: prospective, randomized radiostereometric analysis study of the AGC total knee prosthesis. J Arthroplasty 15:783–792
Altay MA, Erturk C, Altay N, Akmese R, Isikan UE (2012) Patellar denervation in total knee arthroplasty without patellar resurfacing: a prospective, randomized controlled study. Orthop Traumatol Surg Res 98:421–425
Bieger R, Huch K, Kocak S, Jung S, Reichel H, Kappe T (2014) The influence of joint line restoration on the results of revision total knee arthroplasty: comparison between distance and ratio-methods. Arch Orthop Traumatol Surg 134:537–541
Servien E, Viskontas D, Giuffre BM, Coolican MR, Parker DA (2008) Reliability of bony landmarks for restoration of the joint line in revision knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 16:263–269
Gioe TJ, Sinner P, Mehle S, Ma W, Killeen KK (2007) Excellent survival of all-polyethylene tibial components in a community joint registry. Clin Orthop Relat Res 464:88–92
Mohan V, Inacio MC, Namba RS, Sheth D, Paxton EW (2013) Monoblock all-polyethylene tibial components have a lower risk of early revision than metal-backed modular components. Acta Orthop 84:530–536
Rodriguez JA, Baez N, Rasquinha V, Ranawat CS (2001) Metal-backed and all-polyethylene tibial components in total knee replacement. Clin Orthop Relat Res 392:174–183
Mont MA, Pivec R, Issa K, Kapadia BH, Maheshwari A, Harwin SF (2013) Long-term implant survivorship of cementless total knee arthroplasty: a systematic review of the literature and meta-analysis. J Knee Surg 27:369–376. doi:10.1055/s-0033-1361952
Pijls BG, der Linden-Van Van, der Zwaag HM, Nelissen RG (2012) Polyethylene thickness is a risk factor for wear necessitating insert exchange. Int Orthop 36:1175–1180
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yassin, M., Garti, A., Weissbrot, M. et al. All-polyethylene tibial components are not inferior to metal-backed tibial components in long-term follow-up of knee arthroplasties. Eur J Orthop Surg Traumatol 25, 1087–1091 (2015). https://doi.org/10.1007/s00590-015-1645-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-015-1645-y