Abstract
Background
Clinical application of electric stimulation and electromagnetic field stimulation include the treatment of delayed union and nonunion. In the literature success rates up to 90% are reported for the treatment of delayed union and nonunion with pulsed electromagnetic stimulation. We report our experience with pulsed electromagnetic stimulation in the treatment of nonunion.
Methods
All patients treated with pulsed electromagnetic stimulation for a nonunion between January 1996 and January 2000 were included.
Results
A total of 93 patients were included. One group was treated for long bone fractures (LBF) (64 patients). The other group consisted of patients treated for non long bone fractures (NLBF). We evaluated our findings according to clinical and radiographic criteria. The success rate of our treatment of a nonunion with pulsed electromagnetic field was 76% for the LBF group and 79% for the NLBF group.
Conclusion
Pulsed electromagnetic field stimulation of a nonunion showed to be an effective treatment in our study.
Résumé
Problème posé
L’application clinique de la stimulation électrique et de la stimulation par champ électromagnétique correspond au traitement des retards de consolidation et celui des pseudarthroses. Dans la littérature des succès dans 90 % des cas grâce à ces traitements sont décrits. Nous rapportons notre propre expérience dans le traitement des pseudarthroses.
Méthodes
Tous les patients ainsi traités pour pseudarthrose entre janvier 1996 et janvier 2000 ont été inclus dans l’étude.
Résultats
Au total 93 patients ont été inclus. Un groupe de 64 patients a été traité pour fracture d’os longs (LBF). Un autre groupe correspond à des patients ne présentant pas une fracture d’un os long (NLBF). Nous avons étudié les paramètres radio-cliniques. Le taux de succès du traitement des pseudarthroses par application de champ électromagnétique pulsé a été de 76% dans le groupe LBF et de 79% dans le groupe NLBF.
Conclusion
La stimulation par champ électromagnétique pulse des pseudarthrose s’avère être un traitement efficace.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
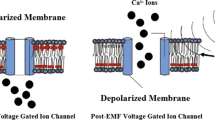
The first successful use of faradic stimulation in the treatment of delayed bone union was reported in the ninetieth century. For unclear reasons this treatment was neglected until the fifties. The early work of Fukada and Yasuda [12] in 1957 demonstrated that mechanical loading of a bone produced electrical potentials in bone tissue. This was followed by a series of fundamental research by Basset and Becker [2] and Friedenburg and Brighton [10], who demonstrated that osteogenesis could be modulated by bioelectric potentials. Bassett et al. [3] implanted iridium electrodes on dog femurs. Through the electrodes a small direct current was induced and an extensive callus formation occurred around the cathode. In 1971 it was Friedenburg [11] and his colleagues who were the first to use this technique in clinical practice. They successfully treated a nonunion of the medial malleolus with electric stimulation. Since the 1950s and 1960s, clinical applications of this technique also include the treatment of delayed union and nonunion. In the literature success rates up to 90% are reported for the treatment of delayed union and nonunion with pulsed electromagnetic stimulation. There are several observational studies that demonstrate the positive effect of electric or electromagnetic stimulation in the treatment of delayed unions and nonunions [4, 6–9, 14]. To our knowledge four double-blind randomized controlled trials of electrical or electromagnetic stimulation versus placebo have been reported [1, 15–17].
The purpose of our study is to provide valid clinical evidence of the effectiveness of pulsed electromagnetic field (PEMF) stimulation in the treatment of nonunions of bone fractures.
Materials and methods
The study was a retrospective open non-blinded study, designed to collect information on patients treated with pulsed electromagnetic fields in the management of their nonunions. Patients served as self-controls. Their pre-PEMF treatment failure was compared to their post-PEMF results. Self-pairing, as a study design, is valid because the constancy of the individual patient’s biological mechanisms and other patient-specific factors essentially eliminates differences between the treatment and the control. It is scientifically valid and medically appropriate to use a paired design technique to study the therapy effect in a medical condition such as nonunion, which has a predictable outcome (e.g., unfavorable in case of no treatment). All patients treated with pulsed electromagnetic stimulation between January 1996 and January 2000 were included irrespective of fracture type or location, length of follow up or outcome.
Skeletally mature patients with a nonunion diagnosis were included in the study. A nonunion was diagnosed when a traumatic fracture had not healed within eight months since the original injury and there was no evidence of healing activity for the last three months. Patients were excluded in the event of a surgical intervention at the nonunion site within the three months prior to initiation of the pulsed electromagnetic stimulation. Other exclusion criteria were non-traumatic fracture, synovial or congenital nonunion, active osteomylitis, fracture gap >10 mm, pregnancy and pacemaker.
The device we used in our study is a pulsed electromagnetic field bone growth stimulator. The signal specifications are shown in Table 1. Two versions of this device were used in the clinical study. One was termed the Orthopulse® I, the other was referred to as Orthopulse® II. The data in Table 1 applies to both devices.
Data were collected from the case report forms (CRF). These CRFs were designed specifically for the study and reflect those data items that were determined to be most relevant to the outcome determination for the patient treated with electromagnetic stimulation.
The clinical evaluation includes an assessment of pain and motion at the fracture site. Pain evaluation was a patient self reported parameter. A Visual Analog Scale was used to describe the patients’ pain intensity. Pain was rated on a scale of 1–5 where 1 represented no pain and 5 represented extreme pain. The treating physician used standard manual examination techniques to evaluate motion at the fracture site.
Motion at the fracture site was categorized as follows none, 1–10 degrees, 11–25 degrees and >25 degrees. Radiographic evaluation was done by the treating surgeon, who reviewed the X-rays for evidence of the following items number of cortices bridged by callus, continuity of cancellous bone across the fracture site, fracture line presence or absence. The same X-rays were reviewed by an independent surgeon. The identity of the patient, the treating surgeon and the facility were blinded. Clinical and radiographic evaluation took place at 3 months prior to stimulation, at time of stimulation, 6 and 12 weeks after start of stimulation and 6 months post removal of stimulation.
In our clinical study the endpoint was to establish efficiency by pre- and post-treatment comparison of physical examinations and radiographic reviews for each patient in the study. Each investigator conducted the clinical and radiographic evaluations for his own patients. Additionally, an independent evaluator examined X-rays. Table 2 depicts the criteria for success or failure in the study.
Statistical methods
Results were presented descriptively by patient population and for selected sub-populations. Since the sample sizes decrease slightly at later evaluations, post application visit data were compared to the bone growth stimulation (BGS) application visit data pair wise based on the number of patients completing each evaluation. The percentage of patients with positive responses (immobilization and presence of fracture line) was compared to baseline using sign tests. Numerical or ordered categorical data (number of cortices bridged, anterior/posterior (A/P) and medial/lateral (M/L) continuity, motion and pain scores) were compared to baseline using Wilcoxon signed rank tests. Due to smaller sample sizes no statistical comparisons were done for sub population analyses, however trends may be noted.
Results
Four hundred and fifteen patients in more than ten hospitals in the Netherlands were treated with pulsed electromagnetic fields for a non-union from January 1996 to January 2000. Ninety-three of the 415 patients met the required criteria: elapsed time since injury, no surgery 3 months before start of stimulation and sufficient follow up. The average time of follow-up was 37 weeks (range 29–61 weeks). The patient age ranged from16 to 83 years with a median age of 38 years. Further screening resulted in a categorization of the 93 patients into two groups. One group was treated for long bone fractures (LBF) such as: humerus, ulna/radius, femur, tibia and fibula (64 patients). The other group consisted of patients treated for non long bone fractures (NLBF) such as: scaphoid, clavicular, metatarsal, metacarpal and calcaneus (29 patients). The elapsed time since injury of these fractures ranged from 8 months to 461 months. Tibial fractures represented the largest number of single, long bone locations (28%). The mean duration of treatment with the BGS was 13 weeks (Table 3). The fracture management at the time of injury was as follows. Internal fixation was used to manage the fracture for 48% of the LBF patients and 24% of the NLBF patients. For those patients who received a bone graft, autograft was the preferred source for both groups. An additional 30% of fractures among the LBF group and 7% among the NLBF group were managed with external fixation. A cast or other form of immobilization was prescribed for 38 and 45% of the LBF and NLBF patients, respectively (Table 4). Immobilization of the injured extremity at the time of injury was prescribed for all but 1 patient in the LBF group and 1 patient in the NLBF group. Sixty-two percent of the LBF group patients and 88% of the NLBF patients did not require immobilization after treatment with the BGS. The type of immobilization included cast (81%) for both groups. Once the BGS was removed, only 22 (38%) of the LBF patients still had prescribed immobilization. At the visit post removal of BGS the number of NLBF patients requiring prescribed immobilization dropped to 3 (13%). Of these, two patients had a cast and one required the use of a brace. Significant differences in the prescribed immobilization occurred for both LBF and NLBF groups from BGS application to a visit post BGS-removal (Table 5). Twenty-seven of the LBF patients and 15 of the NLBF group had surgery other than at the time of their original injury but prior to the installation of the BGS.
Clinical evaluation
The characteristics of motion at the fracture site and the patient’s report of pain were reviewed across time. Of the LBF group, there were 24 patients (38%) presenting with some degree of movement at the site at the time of BGS application. This percentage steadily declined throughout treatment to one patient (2%) post BGS removal (P < 0.001). There were only 5 NLBF patients (18%) who presented with some degree of motion at the site at the time of BGS application. By the post BGS removal evaluation no patients had motion at the fracture site (P = 0.059) (Table 5).
Patients within the LBF group presented with a mean pain score of 2.4 at the time of BGS application. This dropped significantly by the first post application to 1.7 (P < 0.001) with continued significant decreases through the visit post BGS removal (mean = 1.3). The amount of change in pain was most dramatic in the visits immediately following the BGS application.
NLBF patients showed a similar pattern. At the time of BGS application the group had a mean pain score of 2.8, which dropped significantly to 2.0 (P = 0.001) by the first visit post application. The amount of pain reported continued to be significantly less than at BGS application through BGS removal (mean = 1.4, P = 0.001), with the largest change seen at the first post application visit (Table 5).
Radiographic evaluation
The mean number of cortices bridged showed significant increases from the BGS application visit to all subsequent evaluations (P < 0.001) for both the LBF and NLBF groups. LBF group means increased from 1.0 to 3.2 cortices and NLBF means increased from 0.3 to 3.2 cortices from BGS application to post BGS removal (Table 6). The continuity of cancellous bone across the fracture site was evaluated via A/P view and M/L view. The A/P X-ray view for both the LBF and NLBF groups showed significant changes in the appearance from medians of Fuzzy to Dense over the course of treatment (P < = 0.001 at all evaluations). The M/L X-ray view showed similar findings for both the LBF and NLBF groups. Each group showed significant differences from the BGS application at all evaluations (LBF: P < 0.001; NLBF: P = 0.003 to < 0.001) (Table 6).
For the LBF patients, a fracture line was present in 60 of the 62 (97%) patients at the time of BGS application. This line steadily faded over time with only 19 of 50 (38%) of the X-rays showing fracture lines post BGS removal (P < 0.001). For the NLBF group, there was similar improvement, with the initial X-ray showing 100% with a fracture line reduced to only 30% at the post BGS removal visit (P < 0.001) (Table 6).
Figure 1 a shows the radiograph of a patient with nonunion of the tibia, this patient was treated with PEMF for 12 weeks. As seen in Fig. 1b this treatment was successful (Fig. 1). Figure 2 shows a successful treatment of patient with a nonunion of the radius, the duration of this treatment was 8 weeks (Fig. 2).
Success/failure
According to our clinical and radiographic criteria (Table 3) 45 patients out of 59 in the LBF group and 19 patients out of 24 in the NLBF group were treated successfully (success rates, respectively 76 and 79%).
Discussion
Due to our strict inclusion and exclusion criteria only 93 out of 415 patients could be selected for our study. We would like to emphasize that the patients in the present study had an established non-union of at least 8 months, not a delayed union. A difference between long bone nonunion and non long bone nonunion was made to exclude bias by fracture location. A possible limitation of our study may be that it is not randomized. However patients served as self-controls with a median non-healing of the fracture of 14 months and it would be very unlikely for these fractures to heal spontaneously.
Our success rate of 76% for the LBF group and 79% for the NLBF group corresponds with other reported success rates of electromagnetic stimulation in the treatment of delayed union and non-union. In a large review by Gossling [13], 28 studies of ununited tibial fractures treated with PEMF were compared with 14 studies of similar fractures treated with bone graft with or without internal fixation. The overall success rate for the surgical treatment of 569 ununited tibial fractures was 82% (range, 70–100%). By comparison, the overall success rate of PEMF treatment of 1,718 ununited tibial fractures was 81% (range, 13–100%). Many observational studies have been presented suggesting the efficacy of electromagnetic stimulation in the healing of delayed union and nonunion. Using invasive direct coupling techniques, rates of union of 70–90% have been reported [5]. Four randomized controlled trials [1, 15–17] have been reported comparing results of electric and electromagnetic stimulation with placebo. These studies reported an aggregate of 118 patients with success rates of 55–89%, all but one in favor of electric or electromagnetic stimulation. The one study [1] not in favor of electric or electromagnetic stimulation described a very small population of 16 patients with un-united tibial fractures for at least 52 weeks. The study was double blind and patients were randomly allocated to either active or dummy pulsed electromagnetic field stimulators. Fractures in five of the nine patients with working machines united and fractures in five of the seven patients with dummy machines also united. With the small number of patients included, we should be careful with the interpretation of these results. An additional large scale, randomized, controlled, multicenter study would be useful in showing the exact benefit of electric and electromagnetic field exposure on delayed union and nonunion.
In effect, the presence of a nonunion is a failure of the treatment regime applied at the time of injury. For the patients in this study the BGS was an attempt to prevent the need for further invasive surgery and its attendant risks. Some have described it as a salvage procedure. Pulsed electromagnetic field stimulation of a nonunion showed to be an effective treatment in our study and can be an useful tool in the armentarium of the specialist for treating nonunion.
References
Barker AT, Dixon RA, Sharrard WJ, Sutcliff ML (1984) Pulsed magnetic field therapy for tibial non-union. Interim results of a double-blind trial. Lancet 1(8384):994–996
Bassett CA, Becker RO (1962) Generation of electric potentials by bone in response to mechanical stress. Science 137:1063–1064
Bassett CA, Pawluk RJ, Becker RO (1964) Effects of electric currents on bone in vivo. Nature 204:652–654
Bassett CA, Mitchell SN, Gaston SR (1981) Treatment of ununited tibial diaphyseal fractures with pulsing electromagnetic fields. J Bone Joint Surg [Am] 63(4):511–523
Black J (1987) Electrical stimulation: it’s role in growth, repair, and remodeling of the musculoskeletal system. Praeger, New York
Brighton CT, Black J, Friedenberg ZB, Esterhai JL, Day LJ, Connol JF (1981) A multicenter study of the treatment of non-union with constant direct current. J Bone Joint Surg [Am] 63(1):2–13
Brighton CT, Pollack SR (1985) Treatment of recalcitrant non-union with a capacitively coupled electrical field. A preliminary report. J Bone Joint Surg [Am] 67(4):577–585
De Haas WG, Beaupre A, Cameron H, English E (1986) The Canadian experience with pulsed magnetic fields in the treatment of ununited tibial fractures. Clin Orthop 208:55–58
Dunn AW, Rush GA III (1984) Electrical stimulation in treatment of delayed union and nonunion of fractures and osteotomies. South Med J 77(12):1530–1534
Friedenberg ZB, Brighton CT (1966) Bioelectric potentials in bone. J Bone Joint Surg [Am] 48(5):915–923
Friedenberg ZB, Harlow MC, Brighton CT (1971) Healing of nonunion of the medial malleolus by means of direct current: a case report. J Trauma 11(10):883–885
Fukada E, Yasuda I (1957) On the piezoelectric effects of bone. J Physiol Soc Japan 12:1158–1169
Gossling HR, Bernstein RA, Abbott J (1992) Treatment of ununited tibial fractures: a comparison of surgery and pulsed electromagnetic fields (PEMF). Orthopedics 15(6):711–719
Heckman JD, Ingram AJ, loyd RD, Luck JV Jr, Mayer PW (1981) Nonunion treatment with pulsed electromagnetic fields. Clin Orthop 161:58–66
Scott G, King JB (1994) A prospective double-blind trial of electrical capacitive coupling in the treatment of non-union of long bones. J Bone Joint Surg [Am] 76(6):820–826
Sharrard WJ (1990) A double blind-trial of pulsed electromagnetic fields for delayed union of tibial fractures. J Bone Joint Surg [Br] 72(3):347–355
Simonis RB, Parnell EJ, Ray PS, Paecock JL (2003) Electrical treatment of tibial non-union: a prospective, randomised, double-blind trial. Injury 34(5):357–362
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Punt, B.J., den Hoed, P.T. & Fontijne, W.P.J. Pulsed electromagnetic fields in the treatment of nonunion. Eur J Orthop Surg Traumatol 18, 127–133 (2008). https://doi.org/10.1007/s00590-007-0271-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-007-0271-8