Abstract
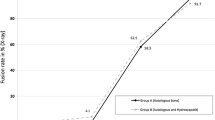
The aim of this report is to analyze the validity of allograft in anterior lumbar interbody fusion. Forty-three patients underwent anterior lumbar interbody fusion using allograft in the period between 1995 and 1998. All suffered from crippling chronic low back pain with or without sciatica. Discogenic disease was verified in 40 cases by discography. All patients were investigated preoperatively with magnetic resonance imaging (MRI). The surgical technique is described. Follow-up radiographs were performed postoperatively, then at 1.5, 3, 6 and 12 months, as required. Radiological fusion was confirmed in all single-level fusions (100%, n=24). In two-level fusions the rate was 93% (n=28/30). However, radiological union could only be confirmed in 11 of the 12 levels in the three-level fusions. Allograft offers a better alternative to autograft for anterior lumbar interbody fusion. Donor site morbidity is avoided, hospital stay is shorter and fusion rates are satisfactory.
Similar content being viewed by others
Author information
Authors and Affiliations
Additional information
Electronic Publication
Rights and permissions
About this article
Cite this article
Sarwat, A., O'Brien, J., Renton, P. et al. The use of allograft (and avoidance of autograft) in anterior lumbar interbody fusion: a critical analysis. Eur Spine J 10, 237–241 (2001). https://doi.org/10.1007/s005860000236
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s005860000236