Abstract
Purpose
Only a few publications considered the influence of the spinopelvic parameters on below-hip anatomy. There is a lack of evidence about the relationship between the anatomic spinopelvic parameters and the posterior tibial slope (PTS). Therefore, the aim of this study was to analyze the association between fixed anatomic spinopelvic parameters and PTS.
Methods
Adult patients presenting with lumbar, thoracic, or cervical complaints together with knee pain at a single hospital between 2017 to 2022 with available standing full-spine lateral radiograph and lateral knee radiograph were retrospectively reviewed. The measured parameters included the pelvic incidence (PI), the sacral kyphosis (SK), the pelvisacral angle, the sacral anatomic orientation (SAO), the sacral table angle, the sacropelvic angle and the PTS. Pearson’s correlations and linear regression analyses were conducted.
Results
A total of 80 patients (44 women), median age 63 years were analyzed. A strong positive correlation was identified between PI and PTS (r = 0.70, p < 0.001). A strong negative correlation was observed between PI and SAO (r = − 0.74, p < 0.001). A strong positive correlation was observed between PI and SK (r = 0.81, p < 0.001). A univariable linear regression analysis showed that PTS can be deduced from PI according to the following formula: PTS = 0.174 × PI − 1.138.
Conclusion
This study is the first to support a positive correlation between the PI and the PTS. We demonstrate that knee anatomy is individually correlated to pelvic shape and therefore influences spinal posture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In order to maintain a horizontal gaze in the erect posture, a complex interplay of hip, pelvic, and spinal alignment is required [1]. Current studies addressing sagittal spinal alignment are mainly focused on the alignment of structures above the hip [2], and only a few publications considered the influence of the spinopelvic parameters on below-hip anatomy. Knee flexion is documented as an important compensatory mechanism to maintain standing balance in spinopelvic malalignment cases [3]. Any alignment alterations due to degenerative changes in the spine, hip or knee produce compensatory changes at other localizations to maintain a balanced posture [1].
However, the relationship between the anatomic spinopelvic parameters and knee parameters is not well understood. The anatomic parameters are independent of the position and orientation of the subjects and constant for an individual at a certain time [4]. The pelvic incidence (PI) is recognized as a key parameter that dictates the morphological characteristics of the pelvis and affects sagittal spinal alignment [1]. During childhood, the pelvic incidence is observed to increase parallel to the acquisition of walking [1]. In adulthood, it is found to remain unchanged as long as the sacroiliac joints remained stable [1]. However, in the last decade, several authors demonstrated increasing PI in older age as a consequence of a twisting in the sacroiliac joints [5, 6]. The posterior tibial slope (PTS) is defined as the angle between the longitudinal axis of the tibia and the posterior inclination of the tibia plateau [7]. The PTS is a key parameter in knee joint stability and biomechanics [8]. PTS affects anterior cruciate ligament tension, flexion gap width and posterior femoral rollback, and consequently influences surgical decisions and outcomes of reconstructive as well as joint preserving knee surgery [9]. There is a lack of evidence about the relationship between the anatomic spinopelvic parameters and the PTS. Therefore, the aim of the present study was to analyze the association between fixed anatomic spinopelvic parameters and PTS.
Materials and methods
Patient population
This study was a retrospective analysis of adult patients presenting with lumbar, thoracic, or cervical complaints in addition to knee pain, at a single university hospital’s orthopedic department from 2017 to 2022. This study was approved by the local ethics committee under rule no. 428/20. An upright standing full-spine lateral radiograph with both femoral heads and anterosuperior iliac spine visible and a strictly lateral knee radiograph had to be present for inclusion. Furthermore, in the lateral knee radiograph the distance between the posterior femoral condyles had to be maximum 5 mm to avoid femoral rotation and the diaphyseal axis had to be visible at least 16 cm below the tibial plateau [10, 11]. Exclusion criteria were (1) patients younger than 18 years old, (2) history of a previous surgical intervention or injury (e.g., tumors or fractures) at the spine, knee or hips leading to modification of the shape of the sacrum, the position of the acetabulae within the pelvis or the femoral condyles, (3) incomplete/missing radiographs, (4) patients with isthmic spondylolysis, (5) non-Caucasian patients, and (6) patients with severe osteoarthritis (OA) leading to a severe modification of the knee, hips and spine were also excluded. The Kellgren–Lawrence classification was used to assess the severity of knee OA in patients with available antero-posterior (a.p.) knee radiograph [12]. Patients with Grade 4 OA were excluded. It is worth noting that in other studies, PI value was not observed to be different in case of degenerative spinal diseases [13]. Patients with isthmic spondylolysis were excluded because cases of isthmic spondylolysis have been associated with significantly higher values of pelvic incidence (PI), which have been shown to be proportional to the degree of slipping [14]. Collected demographic information included age, gender, and ethnicity. Only Caucasian patients were included in this study because several studies demonstrated that sagittal pelvic parameters were different among different ethnicities [15]. The study flow of patient inclusion and exclusion is depicted in Fig. 1.
Pelvic measurements
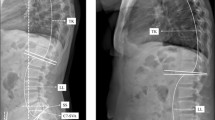
The evaluation of pelvic parameters is based on the bicoxofemoral axis and the superior end plate of the first sacral segment (S1). The hip axis, determined by the midpoint of the bicoxofemoral axis, represents the zero point, and the center, anterior or posterior corner of the S1 end plate represents the end point of the measurements. The pelvic incidence (PI) represents the angle between the line joining the center of the hip axis and the center of the S1 end plate and the line orthogonal to the S1 endplate [16] (Fig. 2). The pelvisacral angle (PSA) is the angle between the line joining the center of the hip axis and the center of the S1 end plate and the line along the S1 endplate [4] (Fig. 2). The sacral anatomic orientation (SAO) represents the angle between the line joining the anterosuperior iliac spine and the anterosuperior edge of the symphysis pubis and the line along the S1 end plate [17] (Fig. 2). The sacral table angle (STA) is the angle between the line along the S1 end plate and the line along the posterior border of the S1 body [18] (Fig. 2). The sacropelvic angle (PRS1) is the angle between the line joining the center of the hip axis and the posterior corner of the S1 end plate and the line along the S1 end plate [4] (Fig. 2). The femorosacral posterior angle (FSPA) represents the angle between the line joining the center of the hip axis and the posterior corner of the S1 end plate and the line along the posterior border of the S1 body [4] (Fig. 2). Sacral kyphosis (SK) has been defined as the angle between a line joining the midpoint of the superior and the inferior borders of S1 and the line joining the inferior borders of S2 and S4 [19] (Fig. 2).
Measurements on a lateral radiograph of the spinopelvic region of a recruited patient. Measurement of sacral table angle (STA) (black angle), sacropelvic angle (PRS1) (red angle), femorosacral posterior angle (FSPA) (green angle), sacral anatomic orientation (SAO) (blue angle). B. Measurement of sacral kyphosis (SK) (black angle), pelvic incidence (PI) (red angle), pelvisacral angle (PSA) (green angle). The circles represent the femoral heads
Knee measurements
The posterior tibial slope (PTS) was determined on a lateral knee radiograph as follows: angle between the tangent of the medial and lateral tibial plateau and the perpendicular line to the diaphyseal tibial axis (Fig. 3). The axis was defined as the connection of two points equidistant between the anterior and posterior border of the tibia, one just below the tibial tubercle and the other 16 cm below the most proximal point [10] (Fig. 3).
Measurement of the posterior tibial slope (PTS) on a lateral knee radiograph of a recruited patient (blue angle). The axis was defined as the connection of two points equidistant between the anterior and posterior border of the tibia, one just below the tibial tubercle and the other 16 cm below the most proximal point (yellow arrows)
Statistical analyses
All parameters were measured by two blinded observers and one of the observers measured twice with a time interval of 3 months for intra- and interrater agreement. All continuous variables were checked first for normal distribution by applying the Shapiro–Wilk Test. Mean and standard deviation (SD) or median and interquartile range [IQR] were reported depending on the distribution of the continuous data. Because all parameters in exception of age were normally distributed, parametric tests were performed. The correlation of PI, PSA, SAO, STA, PRS1, FSPA, SK, and PTS were evaluated with Pearson’s correlation. A Pearson’s coefficient between 0.00 and 0.10 is considered as a negligible correlation, between 0.10 and 0.39 as week, 0.40–0.69 as moderate, between 0.70 and 0.89 as strong and between 0.90 and 1.00 as very strong correlation. For the comparison of two groups, the paired two-sample t-test was performed. Univariable linear regression analysis and multivariable linear regression analysis with adjustment for age were conducted. The intrarater and interrater reliability were evaluated using the intraclass correlation coefficient (ICC) two-way random effects model. ICCs are generally interpreted as follows: < 0.5 is poor, between 0.5 and 0.75 is moderate, between 0.75 and 0.90 is good, and more than 0.90 is excellent. In addition, a power analysis was performed. Statistical analysis was conducted using the software R (version 4.2.2; The R Project for Statistical Computing). Statistical significance was set to p < 0.05.
Results
Among the screened patients, 80 patients (44 women), median age 63 years, fulfilled all the inclusion criteria and were analyzed in this study. Patient demographics and the severity of knee OA assessed by Kellgren–Lawrence are illustrated in Table 1.
Measurement of the anatomic spinopelvic parameters and PTS
Statistically, there was so significant differences between either sex in anatomic spinopelvic parameters and PTS in our patient’s cohort (Table 2).
Pearson’s Correlations between the anatomic spinopelvic parameters and PTS
A strong positive correlation was identified between PI and PTS and reciprocally between PSA and PTS. Furthermore, a strong positive correlation was observed between PI and SK, and reciprocally between PSA and SK. Additionally, a strong positive correlation was identified between FSPA and SK. A strong negative correlation was observed between PI and SAO, and reciprocally between PSA and SAO. There was a strong positive correlation between PRS1 and SAO. A strong negative correlation was observed between PRS1 and SK and between PRS1 and PTS. Table 3 summarize the Pearson’s correlation coefficients of spinopelvic parameters and PTS.
Linear regression analysis
Univariable and multivariable linear regression analysis after adjustment for age showed a significant positive correlation between PI and PTS. PTS can be deduced from PI according to the following formula: PTS = 0.174 × PI − 1.138. Age was not significant in the multivariable linear regression analysis.
Univariable and multivariable linear regression analysis after adjustment for age showed a significant positive correlation between PI and SAO. SAO can be deduced from PI according to the following formula: SAO = − 0.707 × PI + 90.649. Age was not significant in the multivariable linear regression analysis. Univariable and multivariable linear regression analysis after adjustment for age showed a significant positive correlation between PI and SK. SK can be deduced from PI according to the following formula: SK = 0.871 × PI − 15.037. Age was not significant in the multivariable linear regression analysis. Table 4 summarizes the estimate, 95% CI, r-squared and p values for the univariable and multivariable linear regression analysis. Figure 4 showed the graphical representations of the correlations between PI and PTS, PI and SAO, and PI and SK.
Intra- and interrater reliability
The ICC revealed a moderate to excellent intra- and interobserver agreement (Table 5).
Discussion
The aim of the present study was to analyze the correlation between PTS and anatomic spinopelvic parameters. A strong positive correlation was identified between PI and PTS, a strong negative correlation between PI and SAO and a strong positive correlation between PI and SK.
Only a few prior studies insisted on the relationship between anatomic spinopelvic parameters and anatomic parameters of the lower extremity [20, 21]. This study is the first to support a positive correlation between most of the measured pelvic parameters, including the PI and the PTS. Since PI seems to be a major determinant if spinal posture [1], we postulate that everyone has a specific combination of interlinked and anatomically fixed parameters defining their physiologic whole-body posture. Even knee anatomy is individually correlated to pelvic shape and therefore influences spinal posture. Therefore, this study confirms that physiological sagittal alignment and spinal posture is related to a balance between spinopelvic and the lower extremities anatomy [1, 22].
Our findings have clinical implications for knee surgery. Physiologically PTS reconstruction should be a goal of total knee arthroplasty (TKA). The reconstructed PTS plays s significant role in restoring knee kinematic in TKA [23]. However, the optimal PTS angle for postoperative knee function continues to be controversial [23]. Typically, the goal of the reconstructed PTS in TKA corresponds to an arbitrary angle based on the recommendation of prosthesis manufacturers and design [23]. Anatomic pelvic parameters could potentially help calculating the ideal individual PTS. We could deduce a formula between PI and PTS as PTS = 0.174 × PI − 1.138. Our formula could be used to calculate the ideal individual PTS based on anatomic pelvic parameters. In prior studies, investigators have demonstrated increased PI in older age as a consequence of a twisting of the sacroiliac joints [5, 6]. In our patient cohort, however, the variable age was not significant in the multivariable linear regression analysis. Therefore, future studies with larger samples sizes are required to account for a patient’s age in our proposed PTS formula.
A strong correlation between PI and SK means that PI is reflected in sacral anatomy. McKay et al. showed that the pelvis can compensate the kyphotic anatomy of the sacrum by increasing the value of the pelvic tilt and therefore increasing the capacity to position the pelvis through a wider spectrum of angles [24]. The authors showed that if a patient has a pronounced SK, it is likely that they also have a relatively high PI, resulting in favorable ratios of sacral slope (SS) to pelvic incidence. Our data supports previous results of McKay et al. A highly statistically significant positive correlation between the PI and SK was identified r = 0.636, p < 0.0001 [24].
We found a strong negative correlation between PI and SAO in both male and female patients, which supports similar findings in prior studies [17, 25]. Peleg et al. [17] demonstrated that SAO and PI measurements were highly correlated with a coefficient r = − 0.824, p < 0.001 for skeletal material and r = − 0.828, p < 0.001 for adult living individuals. These findings highlight the significance of sacral orientation in determining the proper alignment of the spine.
This study had several limitations. First, selection bias exists due to our cohort consisting of patients who have been referred to our hospital’s spine service with pathology of varying natures. We sought to limit this by excluding patients with isthmic spondylolysis, severe osteoarthrosis, or previous surgery. Second, the sample size was limited, however, the power analysis revealed that the minimum case number required for a significant Pearson correlation is 46. Therefore, the sample size of this study was considered sufficient by power analysis. Third, the PTS was measured on a lateral knee radiograph. The PTS is defined as the angle of the tibial plateau in relation to the mechanical axis of the tibia, which is defined as the connection between the midpoints of the tibial plateau and the distal tibial joint. For this study, the diaphyseal axis was defined between 6 and 16 cm below the tibial plateau. Faschingbauer et al. [10] showed that a reference axis connecting mid-diaphyseal points at 6 and 10 cm below the tibial plateau will overestimate the PTS of 3°, on average, and that the measurement between 6 and 16 cm is more accurate, with an error of 1,5° on average. Additionally, Gwinner et al. [11] demonstrated that lateral knee radiograph may be good alternative if the radiograph contains a sufficient tibial length and femoral rotation is avoided. Furthermore, this study did not include clinical assessment. Lastly, because this study only included Caucasian patients, further studies are needed to confirm the identified correlations in other ethnicities.
Conclusion
This is the first study to identify a positive correlation between pelvic incidence and posterior tibial slope. This study shows that there is an anatomic association between fixed spinopelvic parameters and alignment of below-hip structures. This confirms that the physiologic sagittal alignment of the spine is related to a balance between spinopelvic and lower extremities anatomical parameters, and that each individual patient has a specific combination of interlinked, anatomically fixed, parameters that defines their physiologic whole-body posture.
Availability of data and materials
Data will be available upon request.
Code availability
Not applicable.
References
Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A (2019) Sagittal balance of the spine. Eur Spine J 28(9):1889–1905. https://doi.org/10.1007/s00586-019-06083-1
Offierski CM, Macnab I (1983) Hip-spine syndrome. Spine 8(3):316–321. https://doi.org/10.1097/00007632-198304000-00014
Obeid I, Hauger O, Aunoble S, Bourghli A, Pellet N, Vital J-M (2011) Global analysis of sagittal spinal alignment in major deformities: correlation between lack of lumbar lordosis and flexion of the knee. Eur Spine J 20(S5):681–685. https://doi.org/10.1007/s00586-011-1936-x
Vrtovec T, Janssen MMA, Likar B, Castelein RM, Viergever MA, Pernuš F (2012) A review of methods for evaluating the quantitative parameters of sagittal pelvic alignment. Spine J 12(5):433–446. https://doi.org/10.1016/j.spinee.2012.02.013
Jean L (2014) Influence of age and sagittal balance of the spine on the value of the pelvic incidence. Eur Spine J 23(7):1394–1399. https://doi.org/10.1007/s00586-014-3207-0
Hasegawa K et al (2022) Pelvic thickness, sex, ethnicity, and age affect pelvic incidence in healthy volunteers of Multi-Ethnic Alignment Normative Study (MEANS) database. Eur Spine J 31(6):1421–1430. https://doi.org/10.1007/s00586-022-07134-w
Giffin JR, Vogrin TM, Zantop T, Woo SL-Y, Harner CD (2004) Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 32(2):376–382. https://doi.org/10.1177/0363546503258880
Ahmad R, Patel A, Mandalia V, Toms A (2016) Posterior tibial slope: effect on, and interaction with knee kinematics. JBJS Rev 4(4):15. https://doi.org/10.2106/JBJS.RVW.O.00057
Bernhardson AS et al (2019) Tibial slope and its effect on graft force in posterior cruciate ligament reconstructions. Am J Sports Med 47(5):1168–1174. https://doi.org/10.1177/0363546519827958
Faschingbauer M, Sgroi M, Juchems M, Reichel H, Kappe T (2014) Can the tibial slope be measured on lateral knee radiographs? Knee Surg Sports Traumatol Arthrosc 22(12):3163–3167. https://doi.org/10.1007/s00167-014-2864-1
Gwinner C et al (2019) Assessment of the tibial slope is highly dependent on the type and accuracy of the preceding acquisition. Arch Orthop Trauma Surg 139(12):1691–1697. https://doi.org/10.1007/s00402-019-03201-y
Kohn MD, Sassoon AA, Fernando ND (2016) Classifications in brief: Kellgren–Lawrence classification of osteoarthritis. Clin Orthop Relat Res 474(8):1886–1893. https://doi.org/10.1007/s11999-016-4732-4
Barrey C, Jund J, Noseda O, Roussouly P (2007) Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J 16(9):1459–1467. https://doi.org/10.1007/s00586-006-0294-6
Marty C et al (2002) The sagittal anatomy of the sacrum among young adults, infants, and spondylolisthesis patients. Eur Spine J 11(2):119–125. https://doi.org/10.1007/s00586-001-0349-7
Merrill RK et al (2018) Differences in fundamental sagittal pelvic parameters based on age, sex, and race. Clin Spine Surg A Spine Publ 31(2):E109–E114. https://doi.org/10.1097/BSD.0000000000000555
Legaye J, Duval-Beaupre G, Marty C, Hecquet J (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7(2):99–103. https://doi.org/10.1007/s005860050038
Peleg S, Dar G, Steinberg N, Peled N, Hershkovitz I, Masharawi Y (2007) Sacral orientation revisited. Spine 32(15):E397–E404. https://doi.org/10.1097/BRS.0b013e318074d676
Strube P et al (2018) Association between lumbar spinal degeneration and anatomic pelvic parameters. Clin Spine Surg A Spine Publ 31(6):263–267. https://doi.org/10.1097/BSD.0000000000000660
Wang Z, Parent S, Mac-Thiong J-M, Petit Y, Labelle H (2008) Influence of sacral morphology in developmental spondylolisthesis. Spine 33(20):2185–2191. https://doi.org/10.1097/BRS.0b013e3181857f70
Govil G, Tomar L, Dhawan P (2022) Knee-spine syndrome: management dilemma when knee osteoarthritis coexists with spine degeneration. Cureus. https://doi.org/10.7759/cureus.24939
Oshima Y, Watanabe N, Iizawa N, Majima T, Kawata M, Takai S (2019) Knee–hip–spine syndrome: improvement in preoperative abnormal posture following total knee arthroplasty. Adv Orthop 2019:1–9. https://doi.org/10.1155/2019/8484938
Weng W-J, Wang W-J, Wu M-D, Xu Z-H, Xu L-L, Qiu Y (2015) Characteristics of sagittal spine–pelvis–leg alignment in patients with severe hip osteoarthritis. Eur Spine J 24(6):1228–1236. https://doi.org/10.1007/s00586-014-3700-5
Kang K-T, Koh Y-G, Son J, Kwon O-R, Lee J-S, Kwon S-K (2018) Influence of increased posterior tibial slope in total knee arthroplasty on knee joint biomechanics: a computational simulation study. J Arthroplasty 33(2):572–579. https://doi.org/10.1016/j.arth.2017.09.025
McKay G, Torrie PA, Dempster G, Bertram W, Harding I (2018) The relationship between sacral kyphosis and pelvic incidence. Asian Spine J 12(1):74–79. https://doi.org/10.4184/asj.2018.12.1.74
Maalouly J et al (2020) Sacral anatomical orientation in the lebanese population. Adv Orthop 2020:1–5. https://doi.org/10.1155/2020/4292384
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Conceptualization: TZ, MF. Methodology: MF, TZ. Formal analysis and investigation: TC, HAM, BL, OD. Supervision: HR, TZ, MF, PS, DD. The first draft of the manuscript was written by Thomas Caffard and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of University Ulm rule no. 428/20.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Caffard, T., Awan Malik, H., Lutz, B. et al. Association between posterior tibial slope and anatomic spinopelvic parameters: a retrospective cross-sectional study. Eur Spine J 32, 3616–3623 (2023). https://doi.org/10.1007/s00586-023-07830-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07830-1