Abstract
Introduction
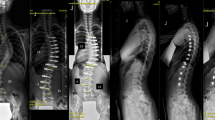
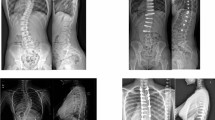
Multiple studies have analyzed the outcome after thoracic Vertebral Body Tethering (VBT). The results seem reproducible with most studies reporting coronal correction rates around 50% and a tether breakage rate near 20% at two years follow-up. There is a paucity of data on lumbar VBT, and no study has yet analyzed the radiographic outcome after lumbar VBT in a double tether technique at two years follow-up, which was the aim of this study.
Methods
This is a retrospective, single surgeons’ data analysis of all consecutive immature patients who have had VBT of the lumbar spine (to L3 or L4) between January 2019 and September 2020. Primary interest focused on coronal curve correction at two years post-operatively. Suspected tether breakages were analyzed separately and defined as an angular change of more than 5° between two adjacent screws.
Results
Forty-one patients were eligible for this study and 35 (85%) had complete two-year follow-up data. Average age at surgery was 14.3 years. All patients had a Sanders stage of 7 or below. Average curve correction for thoracolumbar/lumbar curves at two years follow-up was 50%. 90% of patients had at least one level with a suspected tether breakage. No patient required a revision surgery within two years from surgery but two patients were surgically revised after two years.
Conclusion
VBT in the lumbar spine resulted in 50% coronal curve correction two years post-operatively despite a tether breakage in 90% of patients.




Similar content being viewed by others
Data availability
Data are available.
Code availability
Not applicable.
References
Trobisch PD, Kobbe P, Baroncini A (2020) Dynamic scoliosis correction as alternative treatment for patients with adolescent idiopathic scoliosis: a non-fusion surgical technique. Z Orthop Unfall 158:641–646
Baronicni A, Trobisch PD, Birkenmaier C et al (2022) Radiographic results after vertebral body tethering. Z Orthop Unfall 160:387–392
Raitio A, Syvänen J, Helenius I (2022) Vertebral body tethering: Indications, surgical technique, and a systematic review of published results. J Clin Med 11:2576
Samdani AF, Pahys JM, Ames JR et al (2021) Prospective follow-up report on anterior vertebral body tethering for idiopathic scoliosis: interim results from an FDA IDE study. J Bone Joint Surg Am 103:1611–1619
Alanay A, Yucekul A, Abul K et al (2020) Thoracoscopic vertebral body tethering for adolescent idiopathic scoliosis: follow-up curve behavior according to Sanders skeletal maturity staging. Spine 45:E1483–E1492
Baroncini A, Courvoisier A, Berjano P et al (2022) The effects of vertebral body tethering on sagittal parameters: evaluations from a 2-years follow-up. Eur Spine J 31:1060–1066
Baroncini A, Trobisch PD, Migliorini F (2021) Learning curve for vertebral body tethering: analysis on 90 consecutive patients. Spine Deform 9:141–147
Mathew S, Larson AN, Potter DD, Milbrandt TA (2021) Defining the learning curve in CT-guided navigated thoracoscopic vertebral body tethering. Spine Deform 9:1581–1589
Nicolini LF, Kobbe P, Seggewiß J et al (2022) Motion preservation surgery for scoliosis with a vertebral body tethering system: a biomechanical study. Eur Spine J 31:1013–1021
Mathew SE, Milbrandt TA, Larson AN (2022) Measurable lumbar motion remains 1 year after vertebral body tethering. J Pediatr Orthop 42:e861–e867
Trobisch PD, Baroncini A (2021) Preliminary outcomes after vertebral body tethering (VBT) for lumbar curves and subanalysis of a 1-versus 2-tether construct. Eur Spine J 30:3570–3576
Trobisch P, Baroncini A, Berrer A, Da Paz S (2022) Difference between radiographically suspected and intraoperatively confirmed tether breakages after vertebral body tethering for idiopathic scoliosis. Eur Spine J 31:1045–1050
Baroncini A, Trobisch P, Eschweiler J, Migliorini, (2022) Analaysis of the risk factors for early tether breakage following vertebral body tethering in adolescent idiopathic scoliosis. Eur Spine J 31:2348–2354
Baroncini A, Migliorini F, Eschweiler J, Hildebrand F, Trobisch P (2022) The timing of tether breakage influences clinical results after VBT. Eur Spine J 31:2362–2367
Jain V, Lykissas M, Trobisch P et al (2014) Surgical aspects of spinal growth modulation in scoliosis correction. Instr Course Lect 63:335–344
Newton P, Takahashi Y, Yang Y et al (2022) Anterior vertebral body tethering for thoracic idiopathic scoliosis leads to asymmetric growth of the periapical vertebrae. Spine Deform 10:553–561
Will RE, Stokes IA, Qiu X, Walker MR, Sanders JO (2009) Cobb angle progression in adolescent scoliosis begins at the intervertebral disc. Spine 34:2782–2786
Stokes IA, Aronsson DD (2001) Disc and vertebral wedging in patients with progressive scoliosis. J Spinal Disord 14:317–322
Nault ML, Mac-Thiong JM, Roy-Beaudry M et al (2014) Three-dimensional spine parameters can differentiate between progressive and nonprogressive patients with AIS at the initial visit: a retrospective analysis. J Pediatr Orthop 33:618–623
Castelein RM, Pasha S, Cheng JC, Dubousset J (2020) Idiopathic scoliosis as a rotatory decompensation of the spine. J Bone Miner Res 35:1850–1857
Faraj SSA, Holewijn RM, van Hooff ML et al (2016) De novo degenerative lumbar scoliosis: a systematic review of prognostic factors for curve progression. Eur Spine J 25:2347–2358
Funding
No funding was received/required for this study.
Author information
Authors and Affiliations
Contributions
PDT: Lead investigator, Study design, Data analysis. Draft of manuscript, Manuscript revision. Final approval (includes revision). RC: Data analysis. Draft of Manuscript revision. Final approval (includes revision). SDP: Data acquisition, Data analysis. Manuscript revision. Final approval (includes revision). All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflicts of interest
PDT: Consultant: Globus Medical, Stryker Spine; Paid lectures: ZimVie Spine, Triaspine. RC: Stryker Spine Research Grant, Co-owner Cresco Spine (Spring Distraction System), Co-owner Dutch Scoliosis Center, InSpine Netherlands Research Grant, Fondation Yves Cotrel Research Grants, Nuvasive Research Grant, J&J Congress bureau, AO Foundation Research Grant, Eurospine Research Grant, Surgical Advisory Board MRI Guidance, Medical Advisory Board Telefield Medicine. SDP: nothing to disclose.
Ethical approval
This retrospective review was approved by the local ethics committee.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Trobisch, P.D., Castelein, R. & Da Paz, S. Radiographic outcome after vertebral body tethering of the lumbar spine. Eur Spine J 32, 1895–1900 (2023). https://doi.org/10.1007/s00586-023-07740-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07740-2