Abstract
Background
Periprosthetic bone loss is a common observation following arthroplasty. Recognizing and understanding the nature of bone loss is vital as it determines the subsequent performance of the device and the overall outcome. Despite its significance, the term “bone loss” is often misused to describe inflammatory osteolysis, a complication with vastly different clinical outcomes and treatment plans. Therefore, the goal of this review was to report major findings related to vertebral radiographic bone changes around cervical disc replacements, mitigate discrepancies in clinical reports by introducing uniform terminology to the field, and establish a precedence that can be used to identify the important nuances between these distinct complications.
Methods
A systematic review of the literature was conducted following PRISMA guidelines, using the keywords “cervical,” “disc replacement,” “osteolysis,” “bone loss,” “radiograph,” and “complications.” A total of 23 articles met the inclusion criteria with the majority being retrospective or case reports.
Results
Fourteen studies reported periprosthetic osteolysis in a total of 46 patients with onset ranging from 15–96 months after the index procedure. Reported causes included: metal hypersensitivity, infection, mechanical failure, and wear debris. Osteolysis was generally progressive and led to reoperation. Nine articles reported non-inflammatory bone loss in 527 patients (52.5%), typically within 3–6 months following implantation. The reported causes included: micromotion, stress shielding, and interrupted blood supply. With one exception, bone loss was reported to be non-progressive and had no effect on clinical outcome measures.
Conclusions
Non-progressive, early onset bone loss is a common finding after CDA and typically does not affect the reported short-term pain scores or lead to early revision. By contrast, osteolysis was less common, presenting more than a year post-operative and often accompanied by additional complications, leading to revision surgery. A greater understanding of the clinical significance is limited by the lack of long-term studies, inconsistent terminology, and infrequent use of histology and explant analyses. Uniform reporting and adoption of consistent terminology can mitigate some of these limitations. Executing these actionable items is critical to assess device performance and the risk of revision.
Level of Evidence IV
Diagnostic: individual cross-sectional studies with consistently applied reference standard and blinding.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical disc arthroplasty was developed to mitigate problems attributed to fusion, that is, maintaining a greater range of motion and preventing adjacent segment degeneration [1,2,3,4,5,6,7,8,9,10]. However, cervical disc replacements (CDRs) have introduced new complications to the spine, previously observed at the larger, synovial joints [11,12,13,14]. While the materials and surface treatments used for CDRs and larger joint replacements are similar, physiological loading conditions, and kinematics differ. Nonetheless, complications such as periprosthetic bone loss have recently been reported for CDRs [15,16,17,18,19,20,21].
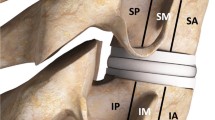
While bone loss has been reported as a radiographic or surgical observation in CDRs, its role in clinical performance is not well understood. This problem is compounded by a lack of uniform terminology which blurs the distinction between non-inflammatory and inflammatory bone loss (osteolysis) [19]. As a result, these distinct terms are often used interchangeably, as evidenced by a recent systematic review, which combined clinical outcomes from patients with non-specific bone loss and bone loss due to osteolysis to draw conclusions on treatments [22]. Osteolysis is characterized by lesions resulting from an inflammatory response (Fig. 1a&b) [23], whereas, non-inflammatory bone loss is a process of adaptation to mechanical changes (Fig. 1c&d) [20]. Consequently, the mechanism of bone loss is important to identify. A schematic image was created to depict two representative progressions of osteolysis versus non-inflammatory bone loss that are often observed. Despite the stark contrast between the two phenomenon, incorrect identification is prevalent. This points to the damaging nature of the terminology and accentuates the need for remedy.
This distinction is pivotal in understanding true incidence of the complications and providing useful information as to the symptoms and timeline associated with either complication. While resorption may be a natural mechanical change with little long-term significance, osteolysis may require a complete redesign or reevaluation of materials. By understanding the clinical relevance of these complications, engineers and implant designers will be better equipped to reassess resulting issues with the device and its design.
Here, we present a systematic review of the literature on CDRs to assess radiographic bone changes and document-reported causations of bone changes. By surveying the reported causes, we can identify common threads among the literature and use this knowledge to establish a lexicon for non-inflammatory bone loss versus osteolysis in the field. The information provided in this study may aid surgeons in assessment of radiographic changes in patients, and in the advancement of implant design and materials.
Methods & materials
Search methodology
Two of the authors (J.M.W. and S.N.S.) systematically searched electronic databases following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [24]. Specifically, a comprehensive search of the PubMed, Google Scholar, and ScienceDirect databases was conducted for studies reporting outcome of CDR including evaluation and assessment of periprosthetic bone loss or osteolysis. The keyword search terms used were “cervical disc replacement/arthroplasty,” “osteolysis,” “bone loss,” “radiograph,” and “complications.” To be included, studies must include a radiographic review, incidence of bone changes, and be written in English. Studies were categorized as prospective, randomized, or retrospective reports.
Data extraction
The following categories of data were extracted for further analysis from each article: (1) general information such as type of device, patient age, and any patient reported clinical outcomes (2) data pertaining to specifics of bone loss or osteolysis, such as time of observation, implant materials, subsequent surgery, and explant analysis results, (3) patient-reported clinical outcomes, and (4) incidence of bone loss or osteolysis. Additionally, any specific information pertaining to bone loss grading criteria, such as that of Kieser et al., was included [25]. In prospective studies in which the number of patients lost to follow-up was not provided, 100% follow-up was assumed.
In a number of studies, the terms “bone loss” and “osteolysis” were used interchangeably, exemplifying ambiguity that the present study aims to address and clarify. In these cases, the present study’s authors analyzed each articles descriptions, provided images, and clues to assess whether the outcome being reported could be deemed as bone loss or osteolysis beyond a reasonable doubt.
Results
Literature review
The searches yielded 1061 articles. Abstracts were screened and reviewed and, after removing studies that did not qualify or were duplicates, 49 articles were further evaluated (Fig. 2). Exclusion criteria included studies lacking bone loss or osteolysis data, focusing on the lumbar spine or anterior cervical discectomy and fusion data only, or lack of radiographic data. Inclusion criteria included fell-text studies assessing patients with a CDR, radiographic evidence of bone loss or osteolysis, and cervical spine data. Nine clinical articles were further excluded, leaving 40 full-text articles to be reviewed. Another 17 articles did not assess bone changes radiographically and were excluded, leaving 23 articles for the present review (Table 1).
Study characteristics
From the 23 included articles, the following information was collected: author(s), number of patients, follow-up, study type, mean patient age, country of origin, and overall reoperation rates (Table 1). Studies that included multiple devices were then separated according to implant, by implant name, implant materials, number of patients, follow-up time, and reported term(s) of bone change. The majority of cases reporting osteolysis distinguished between non-inflammatory bone loss and inflammatory osteolysis, whereas articles focused on bone loss were more inconsistent in their terminology and definitions. Overall, nine articles used bone loss and osteolysis interchangeably to describe the respective bone remodeling seen (Tables 2 and 3). Additionally, when reported, progression, removal, and implantation duration were noted. Results for histology or explant analyses were recorded when presented (Tables 4 and 5).
Reported osteolysis
Overall, fourteen articles reported the resorption of periprosthetic bone due to osteolysis in six implant designs (Table 2). Duration of implantation prior to reoperation ranged from 15–96 months. Radiographic analysis was performed at multiple time points, with progressive osteolysis observed in eight articles [26,27,28,29,30,31,32]. In twelve articles, the implants were removed. In one article, a case report for a 2-level disc replacement, a ventral mass was removed, the devices were retained, and a 3-level posterior fusion was performed [33].
Early reoperation rates were reported for the devices composed of stainless steel or CoCr components, previously reported to be associated with metal sensitivity. Specifically, the Prestige-ST, composed of steel plates and steel core, was reported to have high incidence of osteolysis between 7 and 30 months [28, 34]. Osteolysis was noted later for devices with polymeric components, ranging from 24–120 months following implantation (Table 4).
In eight articles, histological analysis was reported to confirm the radiographic and/or intra-operative diagnosis of osteolysis [29,30,31,32,33, 35, 36]. Two articles reported positive cultures for Propionibacterium acnes[29, 30] and two for Staphylococcus epidermidis.[35, 36] Some of the observations included abundant giant cells, granulomatous formation, macrophages, metal particles, and flakes of polymeric debris, which are features of a potentially osteolysis-inducing foreign body response [23].
Neck pain was most frequently reported for patients with osteolysis [26, 27, 30, 33,34,35,36,37,38]. Radicular symptoms were reported in four studies[28, 33, 35, 38] and paresthesia was reported in three case reports [29, 30, 33]. Other symptoms accompanying osteolysis were: dysphagia, respiratory compromise, myelopathy, shoulder pain, distal upper extremity numbness, and decreased fine motor dexterity. Clinical outcome scores were reported in two case studies with VAS and NDI scores both reporting severe pain [36, 38].
Reported bone loss
Nine articles reported non-inflammatory bone loss in seven implant designs (Table 3). In the majority of studies, the location of bone loss was specified as the anterior region of the vertebral bodies [39,40,41,42], occurring 3–6 months post-operative. Only one article reported failure of an implant with severe bone loss; however, other adverse events were reported in that case, so it was unclear what the main cause of revision was [43]. In contrast, the remaining eight articles reported no progression or correlation of bone loss and device failure (Table 5). For these studies, mean length of follow-up ranged from 24–120 months; therefore, some studies may not have sufficient follow-up time to assess long-term ramifications of early bone loss.
Five articles reported range of motion (ROM) data for the patient cohorts [39,40,41,42, 44]. Of these, only one study compared ROM of patients with or without bone loss, reporting mean pre- operative ROM of 8.99° and final follow-up of 8.25° in patients with bone loss, and pre-operative ROM of 9.1° and post-operative of 7.09° in those with no-bone loss, but this difference was not statistically significant [44]. The remaining articles reported ROM for the total patient population, but did not distinguish between patients with or without bone loss [39,40,41,42]. Combining the results of these nine articles, the ROM at final follow-up was comparable to the pre-operative ROM (P = 0.2).
Among included articles, 515 of 949 (54.2%) patients experienced bone loss of some severity. One article was excluded from this calculation due to duplicity of the patient cohort from another included article. Five articles used grading criteria to rank bone loss, with mild bone loss most commonly reported [25, 39,40,41, 44]. Bone loss differed in both severity and incidence among devices, but because data was not reported consistently, no definitive conclusions could be drawn.
Clinical outcome scores for NDI, VAS arm and neck were measured for patients with bone loss in three articles [39, 40, 44]. However, a combined average could not be calculated due to differences in reporting methodologies. For example, one study reported VAS arm and neck scores using numerical values while another reported scores qualitatively, in terms of minor and major changes [39, 40]. Nevertheless, each concluded that bone loss did not have an effect on clinical outcome scores.
Pain symptoms were reported in four articles; however, three improved over the course of follow-up [39, 41, 43, 45]. Two studies reported early neck pain with long-term improvement [39, 45]. One study reported radicular pain with long-term resolution [41]. The final study reported recurrent neck and arm pain with no resolution until revision. This was the only study reporting bone loss in a failed device [43].
Discussion
Radiographic bone changes in periprosthetic bone are commonly reported after arthroplasties in large joints, and their causes, clinical impact, and management have been the subject of extensive research over the last several decades [23, 46,47,48]. Many factors can stimulate radiographic bone changes including differences in mechanical load distribution, reaction to wear debris, implant micromotion, and infection [20, 46, 47, 49]. While it may seem intuitive that the cervical spine might be vulnerable to these same factors, particularly wear debris and infection, the loading conditions, kinematics, and biological environment differ from large joints [21, 50]. Specifically, the a functional spine unit, or two vertebra and the replaced disc, does not have the “effective joint space” seen in the hip, created by the hip joint’s synovial membrane which can trap wear particles [51]. Consequently, it is unclear whether wear debris particles generated by a CDR would have the potential to generate a host response comparable to that at other joints.
In hip and knee arthroplasties, the terminology used to describe non-inflammatory bone loss and osteolysis has evolved as more information has been gained regarding their etiology and presentation. As a result, clear distinctions between the two processes can be made. Bone loss has been established as a response to mechanical changes, whereas the term ‘osteolysis’ has become synonymous with a progressive bone resorption induced by particulate debris or due to infection, hypersensitivity or fluid pressure [19, 23, 49, 52]. However, this terminology has not translated to spine literature, creating confusion and threatening the ability to correctly assess the impact of a given change on clinical outcome. In the present review, we highlighted the importance of defining type of bone changes to clarify the etiologies behind both non-inflammatory bone loss and osteolysis in the cervical spine [22].
The results of the present review confirmed that non-inflammatory bone loss and osteolysis presented as distinct clinical observations in CDR patients with authors offering several explanations for each, discussed below. Additionally, this review emphasizes the importance of clarifying the type of complication, especially between these terms, so future designs can accurately utilize reported data to address serious failures and potential material concerns, as well as prognostication of outcome. Just as clinical observations show clear distinctions between osteolysis and non-inflammatory bone loss, the subject’s vernacular should follow suit.
Presentation of osteolysis vs. bone loss
The present study emphasizes the stark differences between osteolysis and non-inflammatory bone loss. Inflammatory osteolysis may present around the implant and appear as large lesions being scooped out of the bone (Fig. 1a&1b). By contrast, non-inflammatory bone loss appears as an erosive remodeling of the vertebral body (Fig. 1c&1d). Osteolysis may be present surrounding the implant, whereas bone loss is more common around the peripheral or anterior side of the vertebral body. These clear visual distinctions demand new terminology that accurately describes these differences.
Wear debris
In larger, synovial joints, wear debris has long been recognized as a potential cause of osteolysis. However, in several studies in the present review, the early onset of bone resorption led authors to conclude that wear debris was an unlikely primary cause [39, 41, 44, 45, 53]. In late onset cases, progressive osteolysis was attributed to mechanical failure of the M6-C in five studies, despite findings consistent with device failure and histopathology confirming the presence of particulate polymeric debris and giant cells [29, 30, 33, 35, 36]. This device was noted to include a sheath intended to contain and decrease debris migration, and rupture of the sheath contributed to particle-induced osteolysis [35, 36]. These findings were consistent with those reported for another annulus-nucleus analog device with a sheath, the Bryan [54].
The use of histopathology in confirming the presence of wear debris is pivotal in understanding the etiology behind osteolysis. As with most joint arthroplasties, material selection was crucial for minimizing debris and failures. Although cervical disc replacements utilize similar materials, little is known about how the body responds to these materials in the spine. Unlike most large joints, the spine is not a synovial joint so we cannot use these examples as a precedent. This suggests that material reactions may differ slightly from those observed in other joints and may affect the clinical outcome. Therefore, cases with suspected osteolysis should prioritize histopathology tests to confirm the presence or lack of wear debris in the surrounding tissues.
Stress shielding
In the articles reviewed, stress shielding was frequently cited as a cause of non-inflammatory bone loss. Referencing Wolff’s Law, which states that bones will adapt to applied stresses [55], some articles hypothesized that the implants created higher stresses posteriorly, resulting in remodeling to adapt to the modified stresses [45, 53, 56]. Some articles suggest that resection of the anterior longitudinal ligament (ALL) contributes to reduced stresses in the anterior vertebra after surgery [25]. The common “Smith-Robinson” surgical approach for CDR includes this resection which may increase lordosis, decreasing stresses anteriorly [57]. The ALL increases stability and provides a natural constraint for motion [58]. Radiographic observations of anterior bone loss could result from a change in natural motion and stress distribution after ALL resection. Wang et al. reported that patients with bone loss experienced more lordosis following surgery, possibly due to the resection [42]. They hypothesized that this change in stress patterns left a hypo-pressure area on the anterior portion of the vertebra, leading to resorption. Similarly, Kieser et al.[25, 40] reported the resection of the ALL caused bone loss due to decreased anterior stresses. Although these authors believe the timing is inconsistent with this theory, spinal vertebrae are predominantly composed of trabecular bone, which may remodel much faster than cortical bone surrounding hips or knees.
As most bone loss cases have not been associated with pain symptoms or device failure, this etiology would be consistent with remodeling in the cervical spine in the short post-operative time period while the bone adapts to change in stress and is non-progressive. In order to confirm this, longer follow-up with bone loss patients, as well as biomechanical studies to analyze the force distribution of a healthy and implanted cervical spine, are necessary.
Micromotion
Micromotion is another mechanism that has been attributed to bone loss[49], largely resulting in bone loss immediately anterior or posterior [44]. One study suggested that early micromotion during the first 3–6 months lead to bone loss, but after 6 months, no further change was seen, presumably due to a reduction in micromotion through enhanced fixation [41]. Another study reported that patients with hybrid surgeries who were immobile during the first three months had reduced micromotion and a lower incidence of bone loss [44]. The authors suggested that bone loss may have occurred during the process of osseointegration but stopped following successful integration. It has been widely accepted that cyclic motions under 40–150 microns will allow for bone formation [59]. However, as there are no studies that have quantified micromotion to assess the early fixation of cervical disc replacements, it is unknown if the same threshold can be applied to spine devices.
Infection & metal hypersensitivity
Several authors speculated that infection was the cause for observed osteolysis; yet the majority presented incomplete evidence to confirm infection. Most articles did not provide laboratory results to confirm the infection diagnosis[60] and those that did had conflicting results. Cultures tested positive for either for Propionibacterium acnes or Staphylococcus epidermidis; however, there were reports of some negative cultures or normal inflammatory markers in these cases. Due to this inconsistency, most articles could not conclude that infection was the primary cause [26, 29, 36].
Propionibacterium acnes is well documented to be of low virulence and slow growing, which renders it difficult to culture and diagnose as problematic. Its slow growth requires lengthy periods of incubation, which can lead to contamination and false negatives, further adding to the confusion [61]. Propionibacterium acnes has been reported to show poor sensitivity to standard lab markers such as white blood cell counts and erythrocyte sedimentation rates, making it difficult to detect [62]. Additionally, some positive cultures presented with normal inflammatory markers, suggesting inflammatory markers may not even be sensitive enough in the cervical spine to confirm infection. Therefore, conflicting evidence of an infection associated with osteolysis is expected, making it difficult to confirm an association.
In the absence of a confirmed diagnosis of infection, an immune-mediated response due to metal or polyethylene hypersensitivity was considered a possible cause of the osteolysis [26, 27]. Although hypersensitivity has long been observed in orthopedic implants, no validated test is available to confirm this [63, 64]. Studies that could not confirm infection concluded that wear debris was the main cause of osteolysis, despite no explant images or histological quantification of wear debris being provided. Evidence like this further questions reliability of causation analysis and demands a change.
Incidence & Time of Onset
Osteolysis in large joint replacements may take years to manifest as a clinically significant phenomenon [48, 65]. In contrast, in the spine, some authors reported onset less than a year post-operative, while others reported it after more than five years [26, 28, 29, 35, 36, 60]. The time disparities between onset and failure could be due to the natural history and severity of different causes.
Among the 14 articles reporting osteolysis, 48 patients were reported to have osteolysis and all required reoperation. Because most of these studies were case reports, the incidence of osteolysis could not be determined. Consequently, the prevalence of osteolysis in the general CDR patient population is still unknown. Case reports have highlighted the severity of osteolysis once diagnosed, but to recognize if this is a serious problem with disc replacements, larger patient cohorts and longer follow-up periods are crucial. By contrast, the incidence of bone loss in the nine articles reviewed was 515 out of 949 patients (54.2%), proving bone loss to be highly prevalent post-operatively.
Limitations
This review had several limitations, partly due to gaps in the literature for radiographic bone changes. The reviewed articles included many single case reports or small patient cohorts, limiting confidence in the combined averages tabulated. However, nearly all reported cases of osteolysis that could be attributed to reaction from wear debris were in single case reports. This finding alone emphasizes the importance of including all studies in the present systematic review, and not only randomized clinical trials. Specifically, some previous review articles that have addressed this issue have limited their study to randomized trials and may have severely under-reported the incidence and importance of osteolysis.
Studies were not uniform with their grading system or terminology. In some studies, a large number of cases were reported without clearly specifying how bone loss was assessed, quantified, or reported. Future studies would benefit from a universal grading scale of bone changes and radiographic reviews of larger patient cohorts with longer follow-up.
Conclusions
Short-term, non-inflammatory bone loss is a common observation following CDR, while osteolysis is less frequently reported. Further, while non-inflammatory bone loss rarely leads to revision, osteolysis often progresses and can lead to device removal. Without histology and explant analysis, it is difficult to determine the specific mechanism responsible for bone loss. Although our analysis shows clear differences between these bone changes, these terms are often confused. The practice of interchanging these terms ultimately puts the patient at risk as recommended clinical treatments may not align with the actual prognosis. Therefore, this review highlights the need for uniform terminology to differentiate between non-inflammatory and inflammatory bone changes to identify the nature and severity of the reported bone loss and the need to assess these complications in preclinical trials.
References
Cummins BH, Robertson JT, Gill SS (1998) Surgical experience with an implanted artificial cervical joint. J Neurosurg 88:943–948. https://doi.org/10.3171/jns.1998.88.6.0943
MacDowall A, Canto Moreira N, Marques C, Skeppholm M, Lindhagen L, Robinson Y, Lofgren H, Michaelsson K, Olerud C (2019) Artificial disc replacement versus fusion in patients with cervical degenerative disc disease and radiculopathy: a randomized controlled trial with 5-year outcomes. J Neurosurg Spine 30:323–331. https://doi.org/10.3171/2018.9.SPINE18659
Malham GM, Parker RM, Ellis NJ, Chan PG, Varma D (2014) Cervical artificial disc replacement with ProDisc-C: clinical and radiographic outcomes with long-term follow-up. J Clin Neurosci 21:949–953. https://doi.org/10.1016/j.jocn.2013.09.013
Mehren C, Heider F, Siepe CJ, Zillner B, Kothe R, Korge A, Mayer HM (2017) Clinical and radiological outcome at 10 years of follow-up after total cervical disc replacement. Eur Spine J 26:2441–2449. https://doi.org/10.1007/s00586-017-5204-6
Phillips FM, Geisler FH, Gilder KM, Reah C, Howell KM, McAfee PC (2015) Long-term outcomes of the US FDA IDE prospective, randomized controlled clinical trial comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 40:674–683. https://doi.org/10.1097/BRS.0000000000000869
Vaccaro A (2015) Long-term clinical experience with selectively constrained SECURE-C cervical artificial disc for 1-level cervical disc disease. Int J Spine Surg 12:11
Zeng J, Liu H, Rong X, Wang B, Yang Y, Gao X, Wu T, Hong Y (2018) Clinical and radiographic outcomes of cervical disc arthroplasty with Prestige-LP Disc: a minimum 6-year follow-up study. BMC Musculoskelet Disord 19:285. https://doi.org/10.1186/s12891-018-2201-9
Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, An HS (2002) Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976) 27:2431–2434. https://doi.org/10.1097/00007632-200211150-00003
Gornet MF, Burkus JK, Shaffrey ME, Nian H, Harrell FE Jr (2016) Cervical disc arthroplasty with prestige LP disc versus anterior cervical discectomy and fusion: seven-year outcomes. Int J Spine Surg 10:24. https://doi.org/10.14444/3024
Gornet MF, Burkus JK, Shaffrey ME, Schranck FW, Copay AG (2019) Cervical disc arthroplasty: 10-year outcomes of the Prestige LP cervical disc at a single level. J Neurosurg Spine 31:317–325. https://doi.org/10.3171/2019.2.spine1956
Atkins GJ, Haynes DR, Howie DW, Findlay DM (2011) Role of polyethylene particles in peri-prosthetic osteolysis: a review. World J Orthopedics 2:93–101. https://doi.org/10.5312/wjo.v2.i10.93
Chikaura H, Nakashima Y, Fujiwara Y, Komohara Y, Takeya M, Nakanishi Y (2016) Effect of particle size on biological response by human monocyte-derived macrophages. Biosurf Biotribol 2:18–25. https://doi.org/10.1016/j.bsbt.2016.02.003
Longhofer LK, Chong A, Strong NM, Wooley PH, Yang SY (2017) Specific material effects of wear-particle-induced inflammation and osteolysis at the bone-implant interface: a rat model. J Orthop Transl 8:5–11. https://doi.org/10.1016/j.jot.2016.06.026
Thomas WC, Parvataneni HK, Vlasak RG, Gray CF (2020) Early polyethylene failure in a modern total hip prosthesis: a note of caution. J Arthroplasty 35:1297–1302. https://doi.org/10.1016/j.arth.2019.12.043
Kosse NM, van Hellemondt GG, Wymenga AB, Heesterbeek PJ (2017) Comparable stability of cemented vs press-fit placed stems in revision total knee arthroplasty with mild to moderate bone loss: 6.5-year results from a randomized controlled trial with radiostereometric analysis. J Arthroplasty 32:197–201. https://doi.org/10.1016/j.arth.2016.06.003
Peitgen DS, Innmann MM, Merle C, Gotterbarm T, Moradi B, Streit MR (2018) Periprosthetic bone mineral density around uncemented titanium stems in the second and third decade after total hip arthroplasty: a DXA study after 12, 17 and 21 years. Calcif Tissue Int 103:372–379. https://doi.org/10.1007/s00223-018-0438-9
Ren L, Wang W (2018) Effect of risedronate on femoral periprosthetic bone loss following total hip replacement: a systematic review and meta-analysis. Medicine 97:e0379. https://doi.org/10.1097/md.0000000000010379
Sumner DR (2015) Long-term implant fixation and stress-shielding in total hip replacement. J Biomech 48:797–800. https://doi.org/10.1016/j.jbiomech.2014.12.021
Freeman MA (1999) Radiolucent lines: a question of nomenclature. J Arthroplasty 14:1–2. https://doi.org/10.1016/s0883-5403(99)90195-x
Huiskes R, Ruimerman R, van Lenthe GH, Janssen JD (2000) Effects of mechanical forces on maintenance and adaptation of form in trabecular bone. Nature 405:704–706. https://doi.org/10.1038/35015116
Hallab N, Link HD, McAfee PC (2003) Biomaterial optimization in total disc arthroplasty. Spine (Phila Pa 1976) 28:S139-152. https://doi.org/10.1097/01.brs.0000092214.87225.80
Joaquim AF, Lee NJ, Lehman RA, Tumialán LM, Riew KD (2020) Osteolysis after cervical disc arthroplasty. Eur Spine J 29:10. https://doi.org/10.1007/s00586-020-06578-2
Willert H, Hb B, Buchhorn G (1990) Osteolysis in alloarthroplasty of the hip: the role of ultrahigh molecular weight polyethylene wear particles. Clin Orthop Relat Res 258:95–107
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ : British Medical Journal 349:g7647. https://doi.org/10.1136/bmj.g7647
Kieser DC, Cawley DT, Fujishiro T, Mazas S, Boissière L, Obeid I, Pointillart V, Vital JM, Gille O (2018) Risk factors for anterior bone loss in cervical disc arthroplasty. J Neurosurg Spine 29:123–129. https://doi.org/10.3171/2018.1.spine171018
Tumialán LM, Gluf WM (2011) Progressive vertebral body osteolysis after cervical disc arthroplasty. Spine (Phila Pa 1976) 36:E973-978. https://doi.org/10.1097/BRS.0b013e3181fd863b
Skeppholm M, Henriques T, Tullberg T (2017) Higher reoperation rate following cervical disc replacement in a retrospective, long-term comparative study of 715 patients. Eur Spine J 26:2434–2440. https://doi.org/10.1007/s00586-017-5218-0
Kang DG, Wagner SC, Lehman RA Jr (2014) Osteolysis in the setting of metal-on-metal cervical disc arthroplasty. The Spine J: Off J North Am Spine Soc 14:1362–1365. https://doi.org/10.1016/j.spinee.2014.02.034
Clark NJ, Francois EL, Freedman BA, Currier B (2020) Early implant failure of a 2-Level M6-cervical total disc replacement: a case report. JBJS Case Connector 10:e1900644. https://doi.org/10.2106/jbjs.cc.19.00644
Harris L, Dyson E, Elliot M, Peterson D, Ulbricht C, Casey A (2019) Delayed periprosthetic collection after cervical disc arthroplasty. J Neurosurg Spine. https://doi.org/10.3171/2019.9.spine19900
Baltus C, Costa E, Vaz G, Raftopoulos C (2019) Granulomatous reaction on a double-level cervical total disc arthroplasty. World Neurosurg 122:360–363. https://doi.org/10.1016/j.wneu.2018.11.070
Roschke E, von der Höh NH, Dietz A, Stingu CS, Gradistanac T, Henkelmann J, Heyde CE (2021) A rare case of wear induced complications after cervical disc replacement. Zeitschrift fur Orthopadie und Unfallchirurgie. https://doi.org/10.1055/a-1340-0643
Brophy CM, Hoh DJ (2018) Compressive cervical pannus formation in a patient after 2-level disc arthroplasty: a rare complication treated with posterior instrumented fusion. J Neurosurg Spine 29:130–134. https://doi.org/10.3171/2018.1.spine17867
Wagner SC, Formby PM, Kang DG, Van Blarcum GS, Cody JP, Tracey RW, Lehman RA Jr (2016) Persistent axial neck pain after cervical disc arthroplasty: a radiographic analysis. The Spine J: Off J North Am Spine Soc 16:851–856. https://doi.org/10.1016/j.spinee.2016.02.043
Harati A, Oni P, Oles L, Reuter T, Hamdan M (2020) Vertebral body osteolysis 6 years after cervical disk arthroplasty. J Neurol Surg A Cent Eur Neurosurg 81:188–192. https://doi.org/10.1055/s-0039-1698435
Ruzevick JJW, Chen E, Hofstetter C (2017) Periprostetic osteolysis after 2 level cervical disc arthroplasty featuring artificial nucleus. Jacobs J Spine 1:4
Zavras AG, Sullivan TB, Singh K, Phillips FM, Colman MW (2021) Failure in cervical total disc arthroplasty: single institution experience, systematic review of the literature, and proposal of the RUSH TDA failure classification system. The Spine J. https://doi.org/10.1016/j.spinee.2021.08.006
Ebinu JO, Ramanathan D, Kurtz SM, Lawandy S, Kim KD (2021) Periprosthetic osteolysis in cervical total disc arthroplasty: a single institutional experience. Neurosurg Open. https://doi.org/10.1093/neuopn/okab013
Heo DH, Lee DC, Oh JY, Park CK (2017) Bone loss of vertebral bodies at the operative segment after cervical arthroplasty: a potential complication? Neurosurg Focus 42:E7. https://doi.org/10.3171/2016.10.focus16393
Kieser DC, Cawley DT, Fujishiro T, Tavolaro C, Mazas S, Boissiere L, Obeid I, Pointillart V, Vital JM, Gille O (2019) Anterior bone loss in cervical disc arthroplasty. Asian Spine J 13:13–21. https://doi.org/10.31616/asj.2018.0008
Ren X, Wang W, Chu T, Wang J, Li C, Jiang T (2011) The intermediate clinical outcome and its limitations of Bryan cervical arthroplasty for treatment of cervical disc herniation. J Spinal Disord Tech 24:221–229. https://doi.org/10.1097/BSD.0b013e3181e9f309
Wang X, Meng Y, Liu H, Hong Y, Wang B (2020) Is anterior bone loss the opposite of anterior heterotopic ossification in prestige-lp cervical disc replacement? World Neurosurg 136:e407–e418. https://doi.org/10.1016/j.wneu.2020.01.022
Hacker FM, Babcock RM, Hacker RJ (2013) Very late complications of cervical arthroplasty: results of 2 controlled randomized prospective studies from a single investigator site. Spine (Phila Pa 1976) 38:2223–2226. https://doi.org/10.1097/brs.0000000000000060
Wu TK, Liu H, Wang BY, He JB, Ding C, Rong X, Yang Y, Huang KK, Hong Y (2020) Incidence of bone loss after Prestige-LP cervical disc arthroplasty: a single-center retrospective study of 396 cases. The Spine J: Off J North Am Spine Soc 20:9. https://doi.org/10.1016/j.spinee.2020.05.102
Chen TY, Chen WH, Tzeng CY, Huang CW, Yang CC, Chen HT, Chang CC, Lee CY, Tsou HK (2020) Anterior bone loss after cervical Bryan Disc arthroplasty: insight into the biomechanics following total disc replacement. The Spine J: Off J North Am Spine Soc 20:7. https://doi.org/10.1016/j.spinee.2020.04.017
Gallo J, Goodman SB, Konttinen YT, Raska M (2013) Particle disease: biologic mechanisms of periprosthetic osteolysis in total hip arthroplasty. Innate Immun 19:213–224. https://doi.org/10.1177/1753425912451779
Gallo J, Goodman SB, Konttinen YT, Wimmer MA, Holinka M (2013) Osteolysis around total knee arthroplasty: a review of pathogenetic mechanisms. Acta Biomater 9:8046–8058. https://doi.org/10.1016/j.actbio.2013.05.005
Harris WH (2001) Wear and periprosthetic osteolysis: the problem. Clin Orthop Related Res. https://doi.org/10.1097/00003086-200112000-00007
Bauer TW, Schils J (1999) The pathology of total joint arthroplasty.II. Mech Implant Fail Skelet Radiol 28:483–497. https://doi.org/10.1007/s002560050552
Hallab NJ, Cunningham BW, Jacobs JJ (2003) Spinal implant debris-induced osteolysis. Spine (Phila Pa 1976) 28:S125-138. https://doi.org/10.1097/00007632-200310151-00006
Schmalzried TP, Jasty M, Harris WH (1992) Periprosthetic bone loss in total hip arthroplasty. polyethylene wear debris and the concept of the effective joint space. J Bone Joint Surg Am 74:849–863
Beaulé PE, Campbell P, Mirra J, Hooper JC, Schmalzried TP (2001) Osteolysis in a cementless, second generation metal-on-metal hip replacement. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-200105000-00020
Kim SH, Chung YS, Ropper AE, Min KH, Ahn TK, Won KS, Shin DA, Han IB (2015) Bone loss of the superior adjacent vertebral body immediately posterior to the anterior flange of Bryan cervical disc. Eur Spine J 24:2872–2879. https://doi.org/10.1007/s00586-015-3849-6
Fan H, Wu S, Wu Z, Wang Z, Guo Z (2012) Implant failure of Bryan cervical disc due to broken polyurethane sheath: a case report. Spine (Phila Pa 1976) 37:E814-816. https://doi.org/10.1097/BRS.0b013e3182477d85
Wolff J (1870) Uber die innere Architektur der knochen und ihre Bedeutung Furdir Frage vom Knochenswachstum. Archiv Fur Pathologische ANATOMIE und Physiologie und fur Klische Medizin 50:64
Lin CY, Kang H, Rouleau JP, Hollister SJ, Marca FL (2009) Stress analysis of the interface between cervical vertebrae end plates and the Bryan, Prestige LP, and ProDisc-C cervical disc prostheses: an in vivo image-based finite element study. Spine (Phila Pa 1976) 34:1554–1560. https://doi.org/10.1097/BRS.0b013e3181aa643b
Leven D, Meaike J, Radcliff K, Qureshi S (2017) Cervical disc replacement surgery: indications, technique, and technical pearls. Curr Rev Musculoskelet Med 10:160–169. https://doi.org/10.1007/s12178-017-9398-3
Marchi L, Oliveira L, Coutinho E, Pimenta L (2012) The importance of the anterior longitudinal ligament in lumbar disc arthroplasty: 36-Month follow-up experience in extreme lateral total disc replacement. Int J Spine Surg 6:18–23. https://doi.org/10.1016/j.ijsp.2011.09.002
Pilliar RM, Lee JM, Maniatopoulos C (1986) Observations on the effect of movement on bone ingrowth into porous-surfaced implants. Clin Orthop Relat Res 208:108–113
Park JB, Chang H, Yeom JS, Suk KS, Lee DH, Lee JC (2016) Revision surgeries following artificial disc replacement of cervical spine. Acta Orthop Traumatol Turc 50:610–618. https://doi.org/10.1016/j.aott.2016.04.004
Brolin TJ, Hackett DJ, Abboud JA, Hsu JE, Namdari S (2017) Routine cultures for seemingly aseptic revision shoulder arthroplasty: are they necessary? J Shoulder Elbow Surg 26:2060–2066. https://doi.org/10.1016/j.jse.2017.07.006
Shields MV, Abdullah L, Namdari S (2016) The challenge of Propionibacterium acnes and revision shoulder arthroplasty: a review of current diagnostic options. J Shoulder Elbow Surg 25:1034–1040. https://doi.org/10.1016/j.jse.2016.01.009
Christiansen K, Holmes K, Zilko PJ (1980) Metal sensitivity causing loosened joint prostheses. Ann Rheum Dis 39:476–480. https://doi.org/10.1136/ard.39.5.476
Elves MW, Wilson JN, Scales JT, Kemp HB (1975) Incidence of metal sensitivity in patients with total joint replacements. BMJ 4:376–378. https://doi.org/10.1136/bmj.4.5993.376
Gupta SK, Chu A, Ranawat AS, Slamin J, Ranawat CS (2007) Review ARTICLE: OSTEOLYSIS AFTER TOTAL KNEE ARTHROPlasty. J Arthroplasty 22:787–799. https://doi.org/10.1016/j.arth.2007.05.041
Acknowledgements
This study was funded by OrthoFix, Plano, TX.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The institution, Orthopedic Institute for Children, received a research grant funded by OrthoFix, Plano, TX for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wahbeh, J.M., Park, SH., Campbell, P. et al. The lexicon for periprosthetic bone loss versus osteolysis after cervical disc arthroplasty: a systematic review. Eur Spine J 31, 830–842 (2022). https://doi.org/10.1007/s00586-021-07092-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-07092-9