Abstract
Purpose
Multiple-rod constructs (MRCs) are often used in deformity correction for increased stability and rigidity. There are currently no reports showing minimally invasive placement of MRCs in adult deformity surgery and its technical feasibility through preoperative software planning.
Methods
Data were collected retrospectively from medical records of six consecutive patients who underwent minimally invasive MRCs with robotics planning by a single surgeon at an academic center between March–August 2020.
Results
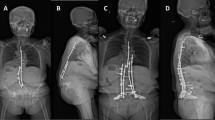
A total of six patients (4 females, mean age 69.7 years) underwent minimally invasive long-segment (6 +) posterior fixation with multiple rods (3 +) using the Mazor X Stealth Edition robotics platform. Average follow-up was 14.3 months. All patients underwent oblique lumbar interbody fusion (OLIF) as a first stage, followed by second stage posterior fixation in the same day. The mean number of levels posteriorly instrumented was 8.8. One patient underwent 3 rod fixation (1 iliac, 2 S2AI) and 5 patients underwent quad rod fixation (2 iliac, 2 S2AI). The mean time to secure all rods was 8 min 36 s. Mean improvement in spinopelvic parameters was -4.9 cm sagittal vertical axis, 18.0° lumbar lordosis, and -10.7° pelvic tilt with an average pelvic incidence of 62.5°. Estimated blood loss (EBL) was 100–250 cc with no blood transfusions, and all but one patient ambulated on postoperative day 1 or 2.
Conclusion
Spinal robotics brings us into a new era of minimally invasive construct design. To our knowledge, this is the first description of the technical feasibility of MRCs in minimally invasive adult spinal deformity surgery.






Similar content being viewed by others
References
Lovecchio F, Qureshi SA (2019) The current state of minimally invasive approaches to adult spinal deformity. Curr Rev Musculoskelet Med. https://doi.org/10.1007/s12178-019-09570-6
Burks SS, Uribe JS, Kolcun JPG, Fortunel A, Godzik J, Bach K, Wang MY (2019) Proximal fusion constructs in minimally invasive scoliosis surgery are successful without interbody or intertransverse fusion. J Neurosurg Spine. https://doi.org/10.3171/2019.5.SPINE19192
Shen FH, Qureshi R, Tyger R, Lehman R, Singla A, Shimer A, Hassanzadeh H (2018) Use of the “dual construct” for the management of complex spinal reconstructions. Spine J 18:482–490. https://doi.org/10.1016/j.spinee.2017.08.235
Sandquist L, Carr D, Tong D, Gonda R, Soo TM (2015) Preventing proximal junctional failure in long segmental instrumented cases of adult degenerative scoliosis using a multilevel stabilization screw technique. Surg Neurol Int 6:112. https://doi.org/10.4103/2152-7806.159383
Graham RB, Sugrue PA, Koski TR (2016) Adult degenerative scoliosis. Clin Spine Surg 29:95–107. https://doi.org/10.1097/BSD.0000000000000367
Wang G, Hu J, Liu X, Cao Y (2015) Surgical treatments for degenerative lumbar scoliosis: a meta analysis. Eur Spine J 24:1792–1799. https://doi.org/10.1007/s00586-015-3942-x
Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, Boachie-Adjei O, Burton DC, Akbarnia BA, Mundis GM, Ames CP, Kebaish K, Hart RA, Farcy JP, Lafage V, ISSG (2013) Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 38:E803-812. https://doi.org/10.1097/BRS.0b013e318292b7
Takemoto M, Boissière L, Vital JM, Pellisé F, Perez-Grueso FJS, Kleinstück F, Acaroglu ER, Alanay A, Obeid I (2017) Are sagittal spinopelvic radiographic parameters significantly associated with quality of life of adult spinal deformity patients? Multivariate linear regression analyses for pre-operative and short-term post-operative health-related quality of life. Eur Spine J 26:2176–2186. https://doi.org/10.1007/s00586-016-4872-y
Fujishiro T, Boissière L, Cawley DT, Larrieu D, Gille O, Vital JM, Pellisé F, Pérez-Grueso FJS, Kleinstück F, Acaroglu E, Alanay A, Obeid I, European Spine Study Group ESSG (2018) Decision-making factors in the treatment of adult spinal deformity. Eur Spine J 27:2312-2321. https://doi.org/10.1007/s00586-018-5572-6
Guevara-Villazón F, Boissiere L, Hayashi K, Larrieu D, Ghailane S, Vital JM, Gille O, Pointillart V, Obeid I, Bourghli A (2020) Multiple-rod constructs in adult spinal deformity surgery for pelvic-fixated long instrumentations: an integral matched cohort analysis. Eur Spine J 29:886–895. https://doi.org/10.1007/s00586-020-06311-z
Palumbo MA, Shah KN, Eberson CP, Hart RA, Daniels AH (2015) Outrigger rod technique for supplemental support of posterior spinal arthrodesis. Spine J 15:1409–1414. https://doi.org/10.1016/j.spinee.2015.03.004
Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH (2007) Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976) 32:2238–2244. https://doi.org/10.1097/BRS.0b013e31814cf24a
Nasser R, Yadla S, Maltenfort MG, Harrop JS, Anderson DG, Vaccaro AR, Sharan AD, Ratliff JK (2010) Complications in spine surgery. J Neurosurg Spine 13:144–157. https://doi.org/10.3171/2010.3.SPINE09369
Hyun SJ, Lenke LG, Kim YC, Koester LA, Blanke KM (2014) Comparison of standard 2-rod constructs to multiple-rod constructs for fixation across 3-column spinal osteotomies. Spine (Phila Pa 1976) 39:1899–1904. https://doi.org/10.1097/BRS.0000000000000556
Jager ZS, İnceoğlu S, Palmer D, Akpolat YT, Cheng WK (2016) Preventing instrumentation failure in three-column spinal osteotomy: biomechanical analysis of rod configuration. Spine Deform 4:3–9. https://doi.org/10.1016/j.jspd.2015.06.005
Wang X, Borgman B, Vertuani S, Nilsson J (2017) A systematic literature review of time to return to work and narcotic use after lumbar spinal fusion using minimal invasive and open surgery techniques. BMC Health Serv Res 17:446. https://doi.org/10.1186/s12913-017-2398-6
Wang MY, Mummaneni PV (2010) Minimally invasive surgery for thoracolumbar spinal deformity: initial clinical experience with clinical and radiographic outcomes. Neurosurg Focus 28:E9. https://doi.org/10.3171/2010.1.FOCUS09286
Choy W, Miller CA, Chan AK, Fu KM, Park P, Mummaneni PV (2018) Evolution of the minimally invasive spinal deformity surgery algorithm: an evidence-based approach to surgical strategies for deformity correction. Neurosurg Clin N Am 29:399–406. https://doi.org/10.1016/j.nec.2018.03.007
Hamilton DK, Kanter AS, Bolinger BD, Mundis GM, Nguyen S, Mummaneni PV, Anand N, Fessler RG, Passias PG, Park P, La Marca F, Uribe JS, Wang MY, Akbarnia BA, Shaffrey CI, Okonkwo DO, ISSG (2016) Reoperation rates in minimally invasive, hybrid and open surgical treatment for adult spinal deformity with minimum 2-year follow-up. Eur Spine J 25:2605–2611. https://doi.org/10.1007/s00586-016-4443-2
Makhni MC, Zhang Y, Park PJ, Cerpa M, Yang M, Pham MH, Sielatycki JA, Beauchamp EC, Lenke LG (2019) The “kickstand rod” technique for correction of coronal imbalance in patients with adult spinal deformity: initial case series. J Neurosurg Spine. https://doi.org/10.3171/2019.9.SPINE19389
Jiang B, Pennington Z, Azad T, Liu A, Ahmed AK, Zygourakis CC, Westbroek EM, Zhu A, Cottrill E, Theodore N (2020) Robot-assisted versus freehand instrumentation in short-segment lumbar fusion: experience with real-time image-guided spinal robot. World Neurosurg 136:e635–e645. https://doi.org/10.1016/j.wneu.2020.01.119
Acknowledgements
There were no sources of funding for this work.
Author information
Authors and Affiliations
Contributions
Dr. Pham reports consultant fees with Medtronic. Mr. Shah reports no disclosures. Dr. Diaz-Aguilar reports no disclosures. Dr. Osorio reports consultant fees with Medtronic, Depuy-Synthes, and Alpha Tec. Dr. Lehman reports consultant fees with Medtronic; speaking and/or teaching arrangements with Medtronic, DePuy, Stryker; grants from the Department of Defense, Defense Medical Research Development Program.
Corresponding author
Ethics declarations
Conflict of interest
M.H. reports consultant fees with Medtronic. V.S. reports no disclosures. D.D. reports no disclosures. R.L. reports consultant fees with Medtronic; speaking and/or teaching arrangements with Medtronic, DePuy, Stryker; grants from the Department of Defense, Defense Medical Research Development Program. J.O. reports consultant fees with Medtronic, DePuy and Alpha Tec.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pham, M.H., Shah, V.J., Diaz-Aguilar, L.D. et al. Minimally invasive multiple-rod constructs with robotics planning in adult spinal deformity surgery: a case series. Eur Spine J 31, 95–103 (2022). https://doi.org/10.1007/s00586-021-06980-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06980-4