Abstract
Study design
A prospective cohort study
Objective
To determine a classification system for cone of economy (CoE) measurements that defines clinically significant changes in altered balance and to assess if the CoE measurements directly impacts patients reported outcome measures (PROMs).
Summary of background data
Preoperative functional data is a crucial component of determining patient disability and prognosis. The CoE has been theorized to be the foundation of biomechanical changes that leads to increased energy expenditure and disability in spine patients. PROMs have been developed to quantify the level of debilitation in spine patients but have various limitations.
Methods
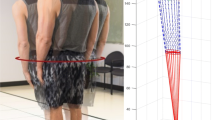
A total of 423 symptomatic adult patients with spine pathology completed a series of PROMs preoperatively including VAS, ODI, Tampa Scale for Kinesiophobia (TSK), Fear and Avoidance Beliefs Questionnaire (FABQ), and Demoralization (DS). Functional balance was tested in this group using a full-body reflective marker set to measure head and center of mass (CoM) sway.
Results
PROMs scores were correlated with the magnitude of the CoE measurements. Patients were separated by the following proposed classification: CoM coronal sway > 1.5 cm, CoM sagittal sway > 3.0 cm, CoM total sway > 30.0 cm, head coronal sway > 3.0 cm, head sagittal sway > 6.0 cm, and head total sway > 60.0 cm. Significant differences were noted in the ODI (< 0.001), FABQ physical activity (< 0.001–0.009), DS (< 0.001–0.023), and TSK (< 0.001–0.032) across almost all planes of motion for both CoM and head sway. The ODI was most sensitive to the difference between groups across CoM and head sway planes with a mean ODI of 47.5–49.5 (p < 0.001) in the severe group versus 36.6–39.3 (p < 0.001) in the moderate group.
Conclusions
By classifying CoE measurements by the cutoffs proposed, clinically significant alterations in balance can be quantified. Furthermore, this study demonstrates that across spinal pathology, higher magnitude CoE and range of sway measurements correlate with worsening PROMs. The Haddas’ CoE classification system in this study helps to identify patients that may benefit from surgery and guide their postoperative prognosis.



Similar content being viewed by others
References
Dubousset J, Weinstein S (1994) The pediatric spine: principles and practice. Three-dimensional Anal Scoliotic Deform 479:496
Godzik J, Frames CW, Smith Hussain V, Olson MC, Kakarla UK, Uribe JS, Lockhart TE, Turner JD (2020) Postural stability and dynamic balance in adult spinal deformity: prospective pilot study. World Neurosurg 141:e783–e791. https://doi.org/10.1016/j.wneu.2020.06.010
Haddas R, Lieberman IH (2018) A method to quantify the “cone of economy.” Eur Spine J 27:1178–1187. https://doi.org/10.1007/s00586-017-5321-2
Haddas R, Ju KL, Belanger T, Lieberman IH (2018) The use of gait analysis in the assessment of patients afflicted with spinal disorders. Eur Spine J. https://doi.org/10.1007/s00586-018-5569-1
Haddas R, Lieberman I, Boah A, Arakal R, Belanger T, Ju KL (2019) Functional balance testing in cervical spondylotic myelopathy patients. Spine 44:103–109. https://doi.org/10.1097/BRS.0000000000002768
Haddas R, Lieberman IH (2019) The change in sway and neuromuscular activity in adult degenerative scoliosis patients pre and post surgery compared with controls. Spine 44:E899-e907. https://doi.org/10.1097/brs.0000000000003009
Haddas R, Lieberman I, Block A, Derman P (2020) The effect of surgical decompression and fusion on functional balance in patients with degenerative lumbar spondylolisthesis. Spine (Phila Pa 1976) 45:E878–E884. https://doi.org/10.1097/BRS.0000000000003436
Haddas R, Satin A, Lieberman I (2020) What is actually happening inside the “cone of economy”: compensatory mechanisms during a dynamic balance test. Eur Spine J. https://doi.org/10.1007/s00586-020-06411-w
Haddas R, Kisinde S, Mar D, Lieberman I (2020) Does improved radiographic alignment truly enhance dynamic functional balance? Spine Deform. https://doi.org/10.1007/s43390-020-00089-2
Horak FB, Henry SM, Shumway-Cook A (1997) Postural perturbations: new insights for treatment of balance disorders. Phys Ther 77:517–533. https://doi.org/10.1093/ptj/77.5.517
Lewis M, Nashner GM (1985) The organization of human postural movements: a formal basis and experimental synthesis. Behav Brain Sci 8:135–150
Ross RT (1991) Dissociated loss of vibration, joint position and discriminatory tactile senses in disease of spinal cord and brain. Can J Neurol Sci 18:312–320
Creath R, Kiemel T, Horak F, Jeka JJ (2008) The role of vestibular and somatosensory systems in intersegmental control of upright stance. J Vestibular Res: Equilib Orientat 18:39–49
Bohm PE, Fehlings MG, Kopjar B, Tetreault LA, Vaccaro AR, Anderson KK, Arnold PM (2017) Psychometric properties of the 30-m walking test in patients with degenerative cervical myelopathy: results from two prospective multicenter cohort studies. Spine J 17:211–217. https://doi.org/10.1016/j.spinee.2016.08.033
Tanishima S, Nagashima H, Ishii H, Fukata S, Dokai T, Murakami T, Morio Y (2017) Significance of stabilometry for assessing postoperative body sway in patients with cervical myelopathy. Asian Spine J 11:763–769. https://doi.org/10.4184/asj.2017.11.5.763
Yoshikawa M, Doita M, Okamoto K, Manabe M, Sha N, Kurosaka M (2008) Impaired postural stability in patients with cervical myelopathy: evaluation by computerized static stabilometry. Spine 33:E460-464. https://doi.org/10.1097/BRS.0b013e318178e666
Labelle H, Mac-Thiong JM, Roussouly P (2011) Spino-pelvic sagittal balance of spondylolisthesis: a review and classification. Eur Spine J 20(Suppl 5):641–646. https://doi.org/10.1007/s00586-011-1932-1
Yagi M, Ohne H, Kaneko S, Machida M, Yato Y, Asazuma T (2018) Does corrective spine surgery improve the standing balance in patients with adult spinal deformity? Spine J 18:36–43. https://doi.org/10.1016/j.spinee.2017.05.023
Hasegawa K, Okamoto M, Hatsushikano S, Shimoda H, Ono M, Homma T, Watanabe K (2017) Standing sagittal alignment of the whole axial skeleton with reference to the gravity line in humans. J Anat 230:619–630. https://doi.org/10.1111/joa.12586
Obeid I, Hauger O, Aunoble S, Bourghli A, Pellet N, Vital JM (2011) Global analysis of sagittal spinal alignment in major deformities: correlation between lack of lumbar lordosis and flexion of the knee. Eur Spine J 20(Suppl 5):681–685. https://doi.org/10.1007/s00586-011-1936-x
Kim S, Duncan PW, Groban L, Segal H, Abbott RM, Williamson JD (2017) Patient-reported outcome measures (PROM) as a preoperative assessment tool. J Anesth Perioper Med 4:274–281
Hey HWD, Luo N, Chin SY, Lau ETC, Wang P, Kumar N, Lau LL, Ruiz JN, Thambiah JS, Liu KG, Wong HK (2018) The predictive value of preoperative health-related quality-of-life scores on postoperative patient-reported outcome scores in lumbar spine surgery. Glob Spine J 8:156–163. https://doi.org/10.1177/2192568217701713
Nayak NR, Coats JM, Abdullah KG, Stein SC, Malhotra NR (2015) Tracking patient-reported outcomes in spinal disorders. Surg Neurol Int 6:S490-499. https://doi.org/10.4103/2152-7806.166892
Diebo BG, Shah NV, Boachie-Adjei O, Zhu F, Rothenfluh DA, Paulino CB, Schwab FJ, Lafage V (2019) Adult spinal deformity. Lancet (London, England) 394:160–172. https://doi.org/10.1016/s0140-6736(19)31125-0
Ailon T, Smith JS, Shaffrey CI, Lenke LG, Brodke D, Harrop JS, Fehlings M, Ames CP (2015) Degenerative spinal deformity. Neurosurgery 77(Suppl 4):S75-91. https://doi.org/10.1227/neu.0000000000000938
Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, DeWald C, Mehdian H, Shaffrey C, Tribus C, Lafage V (2012) Scoliosis research society-schwab adult spinal deformity classification: a validation study. Spine 37:1077–1082. https://doi.org/10.1097/BRS.0b013e31823e15e2
Daubs MD, Lenke LG, Bridwell KH, Kim YJ, Hung M, Cheh G, Koester LA (2013) Does correction of preoperative coronal imbalance make a difference in outcomes of adult patients with deformity? Spine (Phila Pa 1976) 38:476–483. https://doi.org/10.1097/BRS.0b013e3182846eb3
Matz PG, Meagher RJ, Lamer T, Tontz WL Jr, Annaswamy TM, Cassidy RC, Cho CH, Dougherty P, Easa JE, Enix DE, Gunnoe BA, Jallo J, Julien TD, Maserati MB, Nucci RC, O’Toole JE, Rosolowski K, Sembrano JN, Villavicencio AT, Witt JP (2016) Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J 16:439–448. https://doi.org/10.1016/j.spinee.2015.11.055
Rashbaum RF, Ohnmeiss DD, Lindley EM, Kitchel SH, Patel VV (2016) Sacroiliac joint pain and its treatment. Clin Spine Surg 29:42–48
Laslett M, Aprill CN, McDonald B, Young SB (2005) Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther 10:207–218
O’Sullivan S, Schmitz T (2007) Physical rehabilitation. Davis Company, Philadelphia, F.A
Fairbank JCT, Pynsent PB (2000) The oswestry disability index. Spine 25:2940–2953
Weermeijer JD, Meulders A (2018) Clinimetrics: tampa scale for kinesiophobia. J Physiother 64:126. https://doi.org/10.1016/j.jphys.2018.01.001
Neblett R, Hartzell MM, Mayer TG, Bradford EM, Gatchel RJ (2016) Establishing clinically meaningful severity levels for the tampa scale for kinesiophobia (TSK-13). Eur J Pain 20:701–710. https://doi.org/10.1002/ejp.795
Lee CP, Fu TS, Liu CY, Hung CI (2017) Psychometric evaluation of the oswestry disability index in patients with chronic low back pain: factor and mokken analyses. Health Qual Life Outcomes 15:192. https://doi.org/10.1186/s12955-017-0768-8
Brodke DJ, Saltzman CL, Brodke DS (2016) PROMIS for orthopaedic outcomes measurement. J Am Acad Orthop Surg 24:744–749. https://doi.org/10.5435/jaaos-d-15-00404
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors disclose no potential conflicts of interest.
Ethical approval
The study was approved by the Western Institutional Review Board for the Protection of Human Subjects (IRB#: 20152881).
Informed consent
This research involves human participants who signed informed consent before taking part in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Haddas, R., Sambhariya, V., Kosztowski, T. et al. Cone of economy classification: evolution, concept of stability, severity level, and correlation to patient-reported outcome scores. Eur Spine J 30, 2271–2282 (2021). https://doi.org/10.1007/s00586-020-06678-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06678-z