Abstract
Purpose
This systematic review and meta-analysis of all available evidence was performed to assess the safety and efficacy of surgery for lumbar stenosis and spondylolisthesis in patients 80 years or older versus those younger than 80 years.
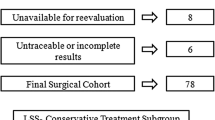
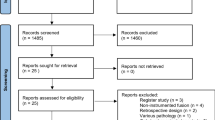
Methods
A search of the literature was conducted in PubMed/MEDLINE, EMBASE and the Cochrane Collaboration Library. Relevant studies comparing the clinical outcomes of lumbar surgery in octogenarians and younger patients were selected according to the eligibility criteria. The predefined endpoints were extracted and meta-analysed from the identified studies.
Results
Data from 16 observational studies including 374,197 patients were included in the final analysis. The pooled data revealed that patients 80 years or older had a significantly higher incidence of overall complication, mortality, readmission and longer length of hospital stay than younger patients. There was a similar improvement in the clinical symptoms (Oswestry Disability Index and pain) of patients in the two groups. No significant differences in overall wound complication, reoperation rate, operative time and intraoperative blood loss were found between the groups.
Conclusions
Our results revealed that the clinical improvement in pain and disability did not significantly differ according to age, although the patients aged 80 years or older had increased incidences of mortality and complication than younger patients. Age alone is not a contraindication for lumbar surgery in very old patients. A careful preoperative evaluation, proper patient selection and appropriate surgical approach are important to achieve successful surgical outcomes.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.









Similar content being viewed by others
References
Fehlings MG, Tetreault L, Nater A, Choma T, Harrop J, Mroz T, Santaguida C, Smith JS (2015) The aging of the global population: the changing epidemiology of disease and spinal disorders. Neurosurgery 77(Suppl 1):S1–S5
Phan K, Mobbs RJ (2016) Minimally invasive versus open laminectomy for lumbar stenosis: a systematic review and meta-analysis. Spine (Phila Pa 1976) 41(2):E91–E100
Dijkerman M, Overdevest G, Moojen W, Vleggeert-Lankamp C (2018) Decompression with or without concomitant fusion in lumbar stenosis due to degenerative spondylolisthesis: a systematic review. Eur Spine J 27(7):1629–1643
Shabat S, Arinzon Z, Folman Y, Leitner J, David R, Pevzner E, Gepstein R, Ilya P, Shuval I (2008) Long-term outcome of decompressive surgery for lumbar spinal stenosis in octogenarians. Eur Spine J 17(2):193–198
Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG (2010) Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 303(13):1259–1265
Nagashima H, Dokai T, Hashiguchi H, Ishii H, Kameyama Y, Katae Y, Morio Y, Morishita T, Murata M, Nanjo Y (2011) Clinical features and surgical outcomes of cervical spondylotic myelopathy in patients aged 80 years or older: a multi-center retrospective study. Eur Spine J 20(2):240
Galiano K, Obwegeser AA, Gabl MV, Bauer R, Twerdy K (2005) Long-term outcome of laminectomy for spinal stenosis in octogenarians. Spine (Phila Pa 1976) 30(3):332–335
Lieber BA, Chiang V, Prabhu AV, Agarwal N, Henry JK, Lin D, Kazemi N, Tabbosha M (2016) Postoperative complications for elderly patients after single-level lumbar fusions for spondylolisthesis. World Neurosurg 91:149–153
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605
Deyo RA, Hickam D, Duckart JP, Piedra M (2013) Complications following surgery for lumbar stenosis in a veteran population. Spine (Phila Pa 1976) 38(19):1695
Giannadakis C, Solheim O, Jakola AS, Nordseth T, Gulati AM, Nerland US, Nygaard ØP, Solberg TK, Gulati S (2016) Surgery for lumbar spinal stenosis in individuals aged 80 and older: a multicenter observational study. J Am Geriatr Soc 64(10):2011–2018
Rihn JA, Hilibrand AS, Zhao W, Lurie JD, Vaccaro AR, Albert TJ, Weinstein J (2015) Effectiveness of surgery for lumbar stenosis and degenerative spondylolisthesis in the octogenarian population: analysis of the Spine Patient Outcomes Research Trial (SPORT) data. J Bone Joint Surg Am 97(3):177
Ulrich NH, Kleinstück F, Woernle CM, Antoniadis A, Winklhofer S, Burgstaller JM, Farshad M, Oberle J, Porchet F, Min K (2015) Clinical outcome in lumbar decompression surgery for spinal canal stenosis in the aged population: a prospective Swiss multicenter cohort study. Spine (Phila Pa 1976) 40(6):415–422
Ciol MA, Deyo RA, Howell E, Kreif S (1996) An assessment of surgery for spinal stenosis: time trends, geographic variations, complications, and reoperations. J Am Geriatr Soc 44(3):285–290
Hayashi K, Matsumura A, Konishi S, Kato M, Namikawa T, Nakamura H (2016) Clinical outcomes of posterior lumbar interbody fusion for patients 80 years of age and older with lumbar degenerative disease: minimum 2 years’ follow-up. Glob Spine J 6(7):665–672
Jansson K-Å, Blomqvist P, Granath F, Nemeth G (2003) Spinal stenosis surgery in Sweden 1987–1999. Eur Spine J 12(5):535–541
Kalanithi PS, Patil CG, Boakye M (2009) National complication rates and disposition after posterior lumbar fusion for acquired spondylolisthesis. Spine (Phila Pa 1976) 34(18):1963–1969
Lagman C, Ugiliweneza B, Boakye M, Drazin D (2017) Spine surgery outcomes in elderly patients versus general adult patients in the United States: a MarketScan analysis. World Neurosurg 103:780–788
Liao J-C, Chen W-J (2018) Surgical outcomes in the elderly with degenerative spondylolisthesis: comparative study between patients over 80 years of age and under 80 years—a gender-, diagnosis-, and surgical method-matched two-cohort analyses. Spine J 18(5):734–739
Machado GC, Maher CG, Ferreira PH, Harris IA, Deyo RA, McKay D, Li Q, Ferreira ML (2017) Trends, complications, and costs for hospital admission and surgery for lumbar spinal stenosis. Spine (Phila Pa 1976) 42(22):1737–1743
Murphy ME, Gilder H, Maloney PR, McCutcheon BA, Rinaldo L, Shepherd D, Kerezoudis P, Ubl DS, Crowson CS, Krauss WE (2017) Lumbar decompression in the elderly: increased age as a risk factor for complications and nonhome discharge. J Neurosurg Spine 26(3):353–362
Nanjo Y, Nagashima H, Dokai T, Hamamoto Y, Hashiguchi H, Ishii H, Kameyama Y, Morio Y, Murata M, Tanida A (2013) Clinical features and surgical outcomes of lumbar spinal stenosis in patients aged 80 years or older: a multi-center retrospective study. Arch Orthop Trauma Surg 133(9):1243–1248
Puvanesarajah V, Jain A, Shimer AL, Li X, Singla A, Shen F, Hassanzadeh H (2017) Complications and mortality following 1 to 2 level lumbar fusion surgery in patients above 80 years of age. Spine (Phila Pa 1976) 42(6):437–441
Battié MC, Jones CA, Schopflocher DP, Hu RW (2012) Health-related quality of life and comorbidities associated with lumbar spinal stenosis. Spine J 12(3):189–195
Sciubba DM, Scheer JK, Yurter A, Smith JS, Lafage V, Klineberg E, Gupta M, Eastlack R, Mundis GM, Protopsaltis TS (2016) Patients with spinal deformity over the age of 75: a retrospective analysis of operative versus non-operative management. Eur Spine J 25(8):2433–2441
Rothenfluh DA, Koenig M, Stokes OM, Behrbalk E, Boszczyk BM (2014) Access-related complications in anterior lumbar surgery in patients over 60 years of age. Eur Spine J 23(Suppl 1):S86–S92
Li G, Patil CG, Lad SP, Ho C, Tian W, Boakye M (2008) Effects of age and comorbidities on complication rates and adverse outcomes after lumbar laminectomy in elderly patients. Spine (Phila Pa 1976) 33(11):1250–1255
Sobottke R, Herren C, Siewe J, Mannion AF, Roder C, Aghayev E (2017) Predictors of improvement in quality of life and pain relief in lumbar spinal stenosis relative to patient age: a study based on the Spine Tango registry. Eur Spine J 26(2):462–472
Costa F, Ortolina A, Tomei M, Cardia A, Zekay E, Fornari M (2013) Instrumented fusion surgery in elderly patients (over 75 years old): clinical and radiological results in a series of 53 patients. Eur Spine J 22(Suppl 6):S910–S913
Antoniadis A, Ulrich NH, Schmid S, Farshad M, Min K (2017) Decompression surgery for lumbar spinal canal stenosis in octogenarians; a single center experience of 121 consecutive patients. Br J Neurosurg 31(1):67–71
Raffo CS, Lauerman WC (2006) Predicting morbidity and mortality of lumbar spine arthrodesis in patients in their ninth decade. Spine (Phila Pa 1976) 31(1):99–103
Shamji MF, Mroz T, Hsu W, Chutkan N (2015) Management of degenerative lumbar spinal stenosis in the elderly. Neurosurgery 77(suppl_1):S68–S74
Försth P, Ólafsson G, Carlsson T, Frost A, Borgström F, Fritzell P, Öhagen P, Michaëlsson K, Sandén B (2016) A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med 374(15):1413–1423
Ghogawala Z, Dziura J, Butler WE, Dai F, Terrin N, Magge SN, Coumans JV, Harrington JF, Amin-Hanjani S, Schwartz JS, Sonntag VK, Barker FG, Benzel EC (2016) Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med 374(15):1424–1434
Drazin D, Lagman C, Bhargava S, Nuño M, Kim TT, Johnson JP (2017) National trends following decompression, discectomy, and fusion in octogenarians and nonagenarians. Acta Neurochir 159(3):517–525
Funding
The study had no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liang, H., Lu, S., Jiang, D. et al. Clinical outcomes of lumbar spinal surgery in patients 80 years or older with lumbar stenosis or spondylolisthesis: a systematic review and meta-analysis. Eur Spine J 29, 2129–2142 (2020). https://doi.org/10.1007/s00586-019-06261-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06261-1