Abstract
Purpose
Candida induced spondylodiscitis of the cervical spine in immunocompetent patients is an extremely rare infectious complication. Since clinical symptoms might be nonspecific, therapeutic latency can lead to permanent spinal cord damage, sepsis and fatal complications. Surgical debridement is strongly recommended but there is no standard antimycotic regime for postsurgical treatment. This paper summarizes available data and demonstrates another successfully treated case.
Methods
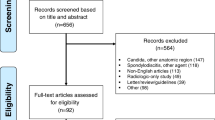
The systematic analysis was performed according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines. PubMed and Web of Science were scanned to identify English language articles. Additionally, the authors describe the case of a 60-year-old male patient who presented with a Candida albicans induced cervical spondylodiscitis after an edematous pancreatitis and C. albicans sepsis. Anterior cervical corpectomy and fusion of C4-C6, additional anterior plating, as well as posterior stabilization C3-Th1 was followed by a 6-month antimycotic therapy. There was neither funding nor conflict of interests.
Results
A systematic literature analysis was conducted and 4599 articles on spondylodiscitis were scanned. Only four cases were found reporting about a C. albicans spondylodiscitis in a non-immunocompromised patient. So far, our patient was followed up for 2 years. Until now, he shows free of symptoms and infection parameters. Standard testing for immunodeficiency showed no positive results.
Conclusion
Candida albicans spondylodiscitis of the cervical spine presents a potentially life-threatening disease. To our knowledge, this is the fifth case in literature that describes the treatment of C. albicans spondylodiscitis in an immunocompetent patient. Surgical debridement has to be considered, following antimycotic regime recommendations vary in pharmaceutical agents and treatment duration.




Similar content being viewed by others
References
Oksi J, Finnilä T, Hohenthal U, Rantakokko-Jalava K (2014) Candida dubliniensis spondylodiscitis in an immunocompetent patient. Case report and review of the literature. Med Mycol Case Rep 3:4–7. doi:10.1016/j.mmcr.2013.11.001
Miller DJ, Mejicano GC (2001) Vertebral osteomyelitis due to Candida species: case report and literature review. Clin Infect Dis 33:523–530. doi:10.1086/322634
Hennequin C, Bourée P, Hiesse C, Dupont B, Charpentier B (1996) Spondylodiskitis due to Candida albicans: report of two patients who were successfully treated with fluconazole and review of the literature. Clin Infect Dis 23:176–178
Voigt C, Lill H (2006) Candida albicans induced spondylodiscitis of the cervical spine of a polytraumatized patient. Unfallchirurg 109:998–1002. doi:10.1007/s00113-006-1143-0
Gouliouris T, Aliyu SH, Brown NM (2010) Spondylodiscitis: update on diagnosis and management. J Antimicrob Chemother 65(Suppl 3):iii11–iii24. doi:10.1093/jac/dkq303
Lewis RE, Klepser ME (1999) The changing face of nosocomial candidemia: epidemiology, resistance, and drug therapy. Am J Health Syst Pharm 56(16):525–533
Garbino J, Schnyder I, Lew D, Bouchuiguir-Wafa K, Rohner P (2003) An unusual cause of vertebral osteomyelitis: Candida species. Scand J Infect Dis 35:288–291
Hendrickx L, Van Wijngaerden E, Samson I, Peetermans WE (2001) Candidal vertebral osteomyelitis: report of 6 patients, and a review. Clin Infect Dis 32:527–533. doi:10.1086/318714
Arias F, Mata-Essayag S, Landaeta ME, Capriles CH, Pérez C, Núñez MJ, Carvajal A, Silva M (2004) Candida albicans osteomyelitis: case report and literature review. Int J Infect Dis 8:307–314. doi:10.1016/j.ijid.2003.12.006
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, Group P-P (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. doi:10.1186/2046-4053-4-1
Ramos A (2013) Vertebral osteomyelitis due to Candida species: a cohort study and review of the literature. Open J Orthop 3:83–89
Gamaletsou MN, Kontoyiannis DP, Sipsas NV, Moriyama B, Alexander E, Roilides E, Brause B, Walsh TJ (2012) Candida osteomyelitis: analysis of 207 pediatric and adult cases (1970–2011). Clin Infect Dis 55:1338–1351. doi:10.1093/cid/cis660
Cone LA, Byrd RG, Potts BE, Wuesthoff M (2004) Diagnosis and treatment of Candida vertebral osteomyelitis: clinical experience with a short course therapy of amphotericin B lipid complex. Surg Neurol 62:234–237. doi:10.1016/j.surneu.2003.11.018 (discussion 237)
Bonakdar-pour A, Gaines VD (1983) The radiology of osteomyelitis. Orthop Clin North Am 14:21–37
Pennisi AK, Davis DO, Wiesel S, Moskovitz P (1985) CT appearance of Candida diskitis. J Comput Assist Tomogr 9:1050–1054
Müller EJ, Russe OJ, Muhr G (2004) Osteomyelitis of the spine. Orthopade 33:305–315. doi:10.1007/s00132-003-0603-2
Williams RL, Fukui MB, Meltzer CC, Swarnkar A, Johnson DW, Welch W (1999) Fungal spinal osteomyelitis in the immunocompromised patient: MR findings in three cases. AJNR Am J Neuroradiol 20:381–385
Pappas PG, Kauffman CA, Andes D, Benjamin DK, Calandra TF, Edwards JE, Filler SG, Fisher JF, Kullberg BJ, Ostrosky-Zeichner L, Reboli AC, Rex JH, Walsh TJ, Sobel JD, America IDSo (2009) Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis 48:503–535. doi:10.1086/596757
Nagata K, Ohashi T, Ariyoshi M, Sonoda K, Imoto H, Inoue A (1998) Percutaneous suction aspiration and drainage for pyogenic spondylitis. Spine (Phila Pa 1976) 23:1600–1606
Wang YC, Lee ST (2001) Candida vertebral osteomyelitis: a case report and review of the literature. Chang Gung Med J 24:810–815
Berbari EF, Kanj SS, Kowalski TJ, Darouiche RO, Widmer AF, Schmitt SK, Hendershot EF, Holtom PD, Huddleston PM, Petermann GW, Osmon DR (2015) Executive summary: 2015 Infectious Diseases Society of America (IDSA) clinical practice guidelines for the diagnosis and treatment of native vertebral osteomyelitis in adults. Clin Infect Dis 61:859–863. doi:10.1093/cid/civ633
Fountain SS (1979) A single-stage combined surgical approach for vertebral resections. J Bone Joint Surg Am 61:1011–1017
Stone JL, Cybulski GR, Rodriguez J, Gryfinski ME, Kant R (1989) Anterior cervical debridement and strut-grafting for osteomyelitis of the cervical spine. J Neurosurg 70:879–883. doi:10.3171/jns.1989.70.6.0879
Abramovitz JN, Batson RA, Yablon JS (1986) Vertebral osteomyelitis. The surgical management of neurologic complications. Spine (Phila Pa 1976) 11:418–420
Fidel PL, Vazquez JA, Sobel JD (1999) Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans. Clin Microbiol Rev 12:80–96
Bailly S, Maubon D, Fournier P, Pelloux H, Schwebel C, Chapuis C, Foroni L, Cornet M, Timsit JF (2016) Impact of antifungal prescription on relative distribution and susceptibility of Candida spp.—trends over 10 years. J Infect 72:103–111. doi:10.1016/j.jinf.2015.09.041
Pfaller MA, Messer SA, Moet GJ, Jones RN, Castanheira M (2011) Candida bloodstream infections: comparison of species distribution and resistance to echinocandin and azole antifungal agents in Intensive Care Unit (ICU) and non-ICU settings in the SENTRY Antimicrobial Surveillance Program (2008–2009). Int J Antimicrob Agents 38:65–69. doi:10.1016/j.ijantimicag.2011.02.016
Cornely OA, Bassetti M, Calandra T, Garbino J, Kullberg BJ, Lortholary O, Meersseman W, Akova M, Arendrup MC, Arikan-Akdagli S, Bille J, Castagnola E, Cuenca-Estrella M, Donnelly JP, Groll AH, Herbrecht R, Hope WW, Jensen HE, Lass-Flörl C, Petrikkos G, Richardson MD, Roilides E, Verweij PE, Viscoli C, Ullmann AJ, Group EFIS (2012) ESCMID* guideline for the diagnosis and management of Candida diseases 2012: non-neutropenic adult patients. Clin Microbiol Infect 18(Suppl 7):19–37. doi:10.1111/1469-0691.12039
Weber ML, Abela A, de Repentigny L, Garel L, Lapointe N (1987) Myeloperoxidase deficiency with extensive candidal osteomyelitis of the base of the skull. Pediatrics 80:876–879
Moon HH, Kim JH, Moon BG, Kim JS (2008) Cervical spondylodiscitis caused by Candida albicans in non-immunocompromised patient. J Korean Neurosurg Soc 43:45–47. doi:10.3340/jkns.2008.43.1.45
Lee SW, Lee SH, Chung HW, Kim MJ, Seo MJ, Shin MJ (2013) Candida spondylitis: comparison of MRI findings with bacterial and tuberculous causes. AJR Am J Roentgenol 201:872–877. doi:10.2214/AJR.12.10344
Acknowledgements
The authors contracted with Michael S. Altus, PhD, ELS, of Intensive Care Communications, Inc., Baltimore, MD, USA, to edit their revised manuscript. The authors thank Dr Altus for his excellent services. The authors maintained complete control over the direction and content of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Rights and permissions
About this article
Cite this article
Stolberg-Stolberg, J., Horn, D., Roßlenbroich, S. et al. Management of destructive Candida albicans spondylodiscitis of the cervical spine: a systematic analysis of literature illustrated by an unusual case. Eur Spine J 26, 1009–1018 (2017). https://doi.org/10.1007/s00586-016-4827-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4827-3