Abstract
Purpose
Many investigators have reported the financial conflicts of interest (COI), which could result in potential bias in the reporting of outcomes for patients undergoing total disc replacement (TDR) rather than anterior cervical discectomy and fusion (ACDF). This bias may be subconsciously introduced by the investigator in a non-blinded radiographic review. The purpose of this study was to determine if bias was present when a group of spine specialists rated adjacent segment degeneration (ASD) following cervical TDR or ACDF.
Methods
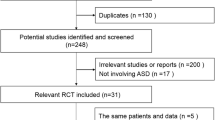
Potential bias in the assessment of ASD was evaluated through the reviews of cervical radiographs (pre- and 6 years post-operative) from patients participating in the ProDisc-C FDA trial (ProDisc-C IDE #G030059). The index level was blinded on all radiographs during the first review, but unblinded in the second. Five reviewers (a radiologist, two non-TDR surgeons, and two TDR surgeons), two of whom had a COI with the ProDisc-C trial sponsor, assessed ASD on a three point scale: yes, no, or unable to assess. Intra- and inter-rater reliabilities between all raters were assessed by the Kappa statistic.
Results
The intra-rater reliability between reviews was substantial, indicating little to no bias in assessing ASD development/progression. The Kappa statistics were 0.580 and 0.644 for the TDR surgeons (p < 0.0001), 0.718 and 0.572 for the non-TDR surgeons (p < 0.0001), and 0.642 for the radiologist (p < 0.0001). Inter-rater reliability for the blinded review ranged from 0.316 to 0.607 (p < 0.0001) and from 0.221 to 0.644 (p < 0.0001) for the unblinded review.
Conclusions
The knowledge of the surgical procedure performed did not bias the assessment of ASD.


Similar content being viewed by others
References
Burkus JK, Haid RW, Traynelis VC, Mummaneni PV (2010) Long-term clinical and radiographic outcomes of cervical disc replacement with the Prestige disc: results from a prospective randomized controlled clinical trial. J Neurosurg Spine 13:308–318. doi:10.3171/2010.3.SPINE09513
Coric D, Nunley PD, Guyer RD, Musante D, Carmody CN, Gordon CR, Lauryssen C, Ohnmeiss DD, Boltes MO (2011) Prospective, randomized, multicenter study of cervical arthroplasty: 269 patients from the Kineflex|C artificial disc investigational device exemption study with a minimum 2-year follow-up: clinical article. J Neurosurg Spine 15:348–358. doi:10.3171/2011.5.SPINE10769
Delamarter RB, Murrey D, Janssen ME, Goldstein JA, Zigler J, Tay BK, Darden B 2nd (2010) Results at 24 months from the prospective, randomized, multicenter Investigational Device Exemption trial of ProDisc-C versus anterior cervical discectomy and fusion with 4-year follow-up and continued access patients. SAS J 4:122–128. doi:10.1016/j.esas.2010.09.001
Goffin J, van Loon J, Van Calenbergh F, Lipscomb B (2010) A clinical analysis of 4- and 6-year follow-up results after cervical disc replacement surgery using the Bryan Cervical Disc Prosthesis. J Neurosurg Spine 12:261–269. doi:10.3171/2009.9.SPINE09129
Heller JG, Sasso RC, Papadopoulos SM, Anderson PA, Fessler RG, Hacker RJ, Coric D, Cauthen JC, Riew DK (2009) Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine 34:101–107. doi:10.1097/BRS.0b013e31818ee263
Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA (2007) Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine 6:198–209. doi:10.3171/spi.2007.6.3.198
Murrey D, Janssen M, Delamarter R, Goldstein J, Zigler J, Tay B, Darden B (2009) Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J 9:275–286. doi:10.1016/j.spinee.2008.05.006
Peng CW, Yue WM, Basit A, Guo CM, Tow BP, Chen JL, Nidu M, Yeo W, Tan SB (2011) Intermediate results of the prestige LP cervical disc replacement: clinical and radiological analysis with minimum two-year follow-up. Spine 36:E105–E111. doi:10.1097/BRS.0b013e3181d76f99
Quan GM, Vital JM, Hansen S, Pointillart V (2011) Eight-year clinical and radiological follow-up of the Bryan cervical disc arthroplasty. Spine 36:639–646. doi:10.1097/BRS.0b013e3181dc9b51
(2011) Conference Program. In: 39th Annual Meeting of the Cervical Spine Research Society. Scottsdale, AZ
(2012) Conference Program. In: 40th Annual Meeting of the Cervical Spine Research Society. Chicago, IL
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Robinson RA, Smith GW (2010) Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. SAS J 4:34–35. doi:10.1016/j.esas.2010.01.003
Cloward RB (1958) The anterior approach for removal of ruptured cervical disks. J Neurosurg 15:602–617. doi:10.3171/jns.1958.15.6.0602
Bohlman HH, Emery SE, Goodfellow DB, Jones PK (1993) Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am 75:1298–1307
Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, An HS (2002) Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine 27:2431–2434. doi:10.1097/01.BRS.0000031261.66972.B1
Fuller DA, Kirkpatrick JS, Emery SE, Wilber RG, Davy DT (1998) A kinematic study of the cervical spine before and after segmental arthrodesis. Spine 23:1649–1656
Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone J Surg Am 81:519–528
Ragab AA, Escarcega AJ, Zdeblick TA (2006) A quantitative analysis of strain at adjacent segments after segmental immobilization of the cervical spine. J Spin Disord Tech 19:407–410
Rao RD, Wang M, McGrady LM, Perlewitz TJ, David KS (2005) Does anterior plating of the cervical spine predispose to adjacent segment changes? Spine 30:2788–2792 (discussion 2793)
Reitman CA, Hipp JA, Nguyen L, Esses SI (2004) Changes in segmental intervertebral motion adjacent to cervical arthrodesis: a prospective study. Spine 29:E221–E226
Schwab JS, Diangelo DJ, Foley KT (2006) Motion compensation associated with single-level cervical fusion: where does the lost motion go? Spine 31:2439–2448. doi:10.1097/01.brs.0000239125.54761.23
Maiman DJ, Kumaresan S, Yoganandan N, Pintar FA (1999) Biomechanical effect of anterior cervical spine fusion on adjacent segments. Bio-Med Mater Eng 9:27–38
Chien A, Lai DM, Wang SF, Cheng CH, Hsu WL, Wang JL (2015) Differential segmental motion contribution of single- and two-level anterior cervical discectomy and fusion. Eur Spine J 24:2857–2865. doi:10.1007/s00586-015-3900-7
Janssen ME, Zigler JE, Spivak JM, Delamarter RB, Darden BV 2nd, Kopjar B (2015) ProDisc-C total disc replacement versus anterior cervical discectomy and fusion for single-level symptomatic cervical disc disease: seven-year follow-up of the prospective randomized US food and drug administration investigational device exemption study. J Bone Joint Surg Am 97:1738–1747. doi:10.2106/jbjs.n.01186
Hisey MS, Bae HW, Davis R, Gaede S, Hoffman G, Kim K, Nunley PD, Peterson D, Rashbaum R, Stokes J (2014) Multi-center, prospective, randomized, controlled investigational device exemption clinical trial comparing Mobi-C Cervical Artificial Disc to anterior discectomy and fusion in the treatment of symptomatic degenerative disc disease in the cervical spine. Int J Spine Surg. doi:10.14444/1007
Mendoza-Lattes S (2015) Cervical disc replacement: are we there yet? Commentary on an article by Michael E. Janssen, DO, et al.: “ProDisc-C total disc replacement versus anterior cervical discectomy and fusion for single-level symptomatic cervical disc disease. seven-year follow-up of the prospective randomized US food and drug administration investigational device exemption study”. J Bone Joint Surg Am 97:e71. doi: 10.2106/jbjs.o.00750
Jia Z, Mo Z, Ding F, He Q, Fan Y, Ruan D (2014) Hybrid surgery for multilevel cervical degenerative disc diseases: a systematic review of biomechanical and clinical evidence. Eur Spine J 23:1619–1632. doi:10.1007/s00586-014-3389-5
Welke B, Schwarze M, Hurschler C, Book T, Magdu S, Daentzer D (2016) In vitro investigation of a new dynamic cervical implant: comparison to spinal fusion and total disc replacement. Eur Spine J 25:2247–2254. doi:10.1007/s00586-015-4361-8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Funding
This is an investigator-initiated study with no external funding.
Rights and permissions
About this article
Cite this article
Laxer, E.B., Brigham, C.D., Darden, B.V. et al. Adjacent segment degeneration following ProDisc-C total disc replacement (TDR) and anterior cervical discectomy and fusion (ACDF): does surgeon bias effect radiographic interpretation?. Eur Spine J 26, 1199–1204 (2017). https://doi.org/10.1007/s00586-016-4780-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4780-1