Abstract
Purpose
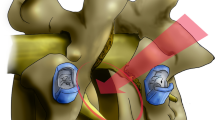
Conventional lumbar arthrodesis for the treatment of degenerative spondylolisthesis (DS) is associated with high complication rates and variable clinical efficacy. Modern minimally invasive (MIS) approaches may reduce the morbidity and produce greater clinical improvement compared to traditional surgical techniques. The objective of this study is to report radiographic outcomes and evaluate clinical improvements in the context of substantial clinical benefit for DS patients treated with a MIS 90° lateral, transpsoas approach for lumbar interbody fusion.
Methods
From 2005 to 2011, 60 consecutive patients were treated with MIS lateral interbody fusion for Grade I or II DS at a single institution. Mean patient age was 68 years, 75 % were female, and 30 % had undergone previous lumbar surgery. A total of 71 levels were treated, supplemental posterior fixation was used in 57 (95 %) cases, and 26 (43 %) patients underwent additional direct posterior decompression.
Results
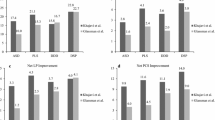
Average follow-up was 20.3 months. Average ORT, EBL, and LOS were 206 min, 83 cc, and 1.29 days, respectively. Complications occurred in 3 (5 %) patients. Transient approach-related thigh/groin pain was observed in 5 (8 %) cases. There were no cases of pseudoarthrosis. At 1 year, LBP improved 71 %, LP improved 68 %, ODI decreased 52 %, and SF-36 PCS and MCS improved 43 and 21 %, respectively. Substantial clinical benefit was met by 94.7 % of patients on NRS LBP, by 84.6 % on NRS LP, by 83.7 % on ODI, and by 66.7 % on SF-36 PCS. Disc height increased 71 % and segmental lordosis increased 27.8 % at treated levels. Foraminal height, width, and volume increased 19.7, 18.0, and 39.6 %, respectively. Slip improved 60.7 % with interbody fusion only and further improved to 69.2 % after the placement of supplemental instrumentation.
Conclusions
MIS lateral interbody fusion in the treatment of DS resulted in significant improvements in clinical and radiographic outcomes, with a low complication rate and a high proportion of patients achieving substantial clinical benefit.





Similar content being viewed by others
References
Weinstein JN, Lurie JD, Tosteson TD, Zhao W, Blood EA, Tosteson AN, Birkmeyer N, Herkowitz H, Longley M, Lenke L, Emery S, Hu SS (2009) Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. Four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am 6:1295–1304
Weinstein JN, Lurie JD, Tosteson TD, Hanscom B, Tosteson AN, Blood EA, Birkmeyer NJ, Hilibrand AS, Herkowitz H, Cammisa FP, Albert TJ, Emery SE, Lenke LG, Abdu WA, Longley M, Errico TJ, Hu SS (2007) Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med 22:2257–2270
Glassman SD, Copay AG, Berven SH, Polly DW, Subach BR, Carreon LY (2008) Defining substantial clinical benefit following lumbar spine arthrodesis. J Bone Joint Surg Am 9:1839–1847
Ozgur BM, Aryan HE, Pimenta L, Taylor WR (2006) Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 4:435–443
Rodgers WB, Gerber EJ, Patterson J (2011) Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine 1:26–32
Oliveira L, Marchi L, Coutinho E, Pimenta L (2010) A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine 26(Suppl):S331–S337
Cappuccino A, Cornwall GB, Turner AW, Fogel GR, Duong HT, Kim KD, Brodke DS (2010) Biomechanical analysis and review of lateral lumbar fusion constructs. Spine 26(Suppl):S361–S367
Elowitz EH, Yanni DS, Chwajol M, Starke RM, Perin NI (2011) Evaluation of indirect decompression of the lumbar spinal canal following minimally invasive lateral transpsoas interbody fusion: radiographic and outcome analysis. Minim Invasive Neurosurg 5–6:201–206
Rodgers WB, Lehmen JA, Gerber EJ, Rodgers JA (2012) Grade 2 spondylolisthesis at L4–5 treated by XLIF: safety and midterm results in the “worst case scenario”. Sci World J 2012:356712
Rodgers WB, Cox CS, Gerber EJ (2010) Early complications of extreme lateral interbody fusion in the obese. J Spinal Disord Tech 6:393–397
Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L (2012) Stand-alone lateral interbody fusion for the treatment of low-grade degenerative spondylolisthesis. Sci World J 2012:456346
Ogilvie JW (2005) Complications in spondylolisthesis surgery. Spine 6(Suppl):S97–101
Lauber S, Schulte TL, Liljenqvist U, Halm H, Hackenberg L (2006) Clinical and radiologic 2-4-year results of transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Spine 15:1693–1698
Park Y, Ha JW, Lee YT, Oh HC, Yoo JH, Kim HB (2011) Surgical outcomes of minimally invasive transforaminal lumbar interbody fusion for the treatment of spondylolisthesis and degenerative segmental instability. Asian Spine J 4:228–236
Meyerding HW (1956) Spondylolisthesis; surgical fusion of lumbosacral portion of spinal column and interarticular facets; use of autogenous bone grafts for relief of disabling backache. J Int Coll Surg 26(5 Part 1):566–591
Matsunaga S, Sakou T, Morizono Y, Masuda A, Demirtas AM (1990) Natural history of degenerative spondylolisthesis. Pathogenesis and natural course of the slippage. Spine 11:1204–1210
Martin CR, Gruszczynski AT, Braunsfurth HA, Fallatah SM, O’Neil J, Wai EK (2007) The surgical management of degenerative lumbar spondylolisthesis: a systematic review. Spine 16:1791–1798
Luk KD, Chow DH, Holmes A (2003) Vertical instability in spondylolisthesis: a traction radiographic assessment technique and the principle of management. Spine 8:819–827
Glassman SD, Carreon LY, Djurasovic M, Dimar JR, Johnson JR, Puno RM, Campbell MJ (2009) Lumbar fusion outcomes stratified by specific diagnostic indication. Spine J 1:13–21
Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG (2007) The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine 24:2764–2770
Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY (2008) Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scales. Spine J 6:968–974
Shamji MF, Isaacs RE (2008) Anterior-only approaches to scoliosis. Neurosurgery 3(Suppl):139–148
Ferrara LA, Secor JL, Jin BH, Wakefield A, Inceoglu S, Benzel EC (2003) A biomechanical comparison of facet screw fixation and pedicle screw fixation: effects of short-term and long-term repetitive cycling. Spine 12:1226–1234
Kawaguchi Y, Matsui H, Tsuji H (1994) Back muscle injury after posterior lumbar spine surgery. Part 2: histologic and histochemical analyses in humans. Spine 22:2598–2602
Kawaguchi Y, Matsui H, Tsuji H (1994) Back muscle injury after posterior lumbar spine surgery. Part 1: histologic and histochemical analyses in rats. Spine 22:2590–2597
Kim CW (2010) Scientific basis of minimally invasive spine surgery: prevention of multifidus muscle injury during posterior lumbar surgery. Spine 26(Suppl):S281–S286
Kim CW, Siemionow K, Anderson DG, Phillips FM (2011) The current state of minimally invasive spine surgery. Instr Course Lect 60:353–370
Kim DY, Lee SH, Chung SK, Lee HY (2005) Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine 1:123–129
Hukins DW, Kirby MC, Sikoryn TA, Aspden RM, Cox AJ (1990) Comparison of structure, mechanical properties, and functions of lumbar spinal ligaments. Spine 8:787–795
Baker JK, Reardon PR, Reardon MJ, Heggeness MH (1993) Vascular injury in anterior lumbar surgery. Spine 15:2227–2230
Flynn JC, Price CT (1984) Sexual complications of anterior fusion of the lumbar spine. Spine 5:489–492
Christensen FB, Bunger CE (1997) Retrograde ejaculation after retroperitoneal lower lumbar interbody fusion. Int Orthop 3:176–180
Brau SA (2002) Mini-open approach to the spine for anterior lumbar interbody fusion: description of the procedure, results and complications. Spine J 3:216–223
Penta M, Fraser RD (1997) Anterior lumbar interbody fusion. A minimum 10-year follow-up. Spine 20:2429–2434
Rajaraman V, Vingan R, Roth P, Heary RF, Conklin L, Jacobs GB (1999) Visceral and vascular complications resulting from anterior lumbar interbody fusion. J Neurosurg 1(Suppl):60–64
Scaduto AA, Gamradt SC, Yu WD, Huang J, Delamarter RB, Wang JC (2003) Perioperative complications of threaded cylindrical lumbar interbody fusion devices: anterior versus posterior approach. J Spinal Disord Tech 6:502–507
Villavicencio AT, Burneikiene S, Bulsara KR, Thramann JJ (2006) Perioperative complications in transforaminal lumbar interbody fusion versus anterior-posterior reconstruction for lumbar disc degeneration and instability. J Spinal Disord Tech 2:92–97
Okuda S, Miyauchi A, Oda T, Haku T, Yamamoto T, Iwasaki M (2006) Surgical complications of posterior lumbar interbody fusion with total facetectomy in 251 patients. J Neurosurg Spine 4:304–309
Rihn JA, Patel R, Makda J, Hong J, Anderson DG, Vaccaro AR, Hilibrand AS, Albert TJ (2009) Complications associated with single-level transforaminal lumbar interbody fusion. Spine J 8:623–629
Tohmeh AG, Rodgers WB, Peterson MD (2011) Dynamically evoked, discrete-threshold electromyography in the extreme lateral interbody fusion approach. J Neurosurg Spine 1:31–37
Tormenti MJ, Maserati MB, Bonfield CM, Okonkwo DO, Kanter AS (2010) Complications and radiographic correction in adult scoliosis following combined transpsoas extreme lateral interbody fusion and posterior pedicle screw instrumentation. Neurosurg Focus 3:E7
Uribe JS, Vale FL, Dakwar E (2010) Electromyographic monitoring and its anatomical implications in minimally invasive spine surgery. Spine 26(Suppl):S368–S374
Epstein NE (2008) How often is minimally invasive minimally effective: what are the complication rates for minimally invasive surgery? Surg Neurol 4:386–388
McAfee PC, Phillips FM, Andersson G, Buvenenadran A, Kim CW, Lauryssen C, Isaacs RE, Youssef JA, Brodke DS, Cappuccino A, Akbarnia BA, Mundis GM, Smith WD, Uribe JS, Garfin S, Allen RT, Rodgers WB, Pimenta L, Taylor W (2010) Minimally invasive spine surgery. Spine 26(Suppl):S271–S273
Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG (1997) Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine 2:210–219
Berjano P, Lamartina C (2011) Minimally invasive lateral transpsoas approach with advanced neurophysiologic monitoring for lumbar interbody fusion. Eur Spine J 9:1584–1586
Berjano P, Balsano M, Buric J, Petruzzi M, Lamartina C (2012) Direct lateral access lumbar and thoracolumbar fusion: preliminary results. Eur Spine J 21:S37–S42
Berjano P, Lamartina C (2013) Far lateral approaches (XLIF) in adult scoliosis. Eur Spine J 22:S242–S253
Hu WK, He SS, Zhang SC, Liu YB, Li M, Hou TS, Ma XL, Wang J (2011) An MRI study of psoas major and abdominal large vessels with respect to the X/DLIF approach. Eur Spine J 4:557–562
Pumberger M, Hughes AP, Huang RR, Sama AA, Cammisa FP, Girardi FP (2012) Neurologic deficit following lateral lumbar interbody fusion. Eur Spine J 6:1192–1199
Conflict of interest
Dr. Khajavi is a consultant for NuVasive, Inc. and has received research grants from NuVasive, Inc., though none were received related to this work. Alessandria Shen, subsequent to this work, became employed directly by NuVasive for a short time and no longer has any conflicts. No other authors report any conflicts.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khajavi, K., Shen, A. & Hutchison, A. Substantial clinical benefit of minimally invasive lateral interbody fusion for degenerative spondylolisthesis. Eur Spine J 24 (Suppl 3), 314–321 (2015). https://doi.org/10.1007/s00586-015-3841-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-3841-1