Abstract
Purpose
Basilar invagination is a rare craniocervical malformation which may lead to neurological deficits related to compression of brainstem and upper cervical cord as well as instability of the craniocervical junction. This study presents results of a treatment algorithm developed over a 20-year period focussing on anatomical findings, short-term and long-term outcomes.
Methods
69 patients with basilar invagination (mean age 41 ± 18 years, history 64 ± 85 months) were encountered. The clinical courses were documented with a score system for individual neurological symptoms for short-term results after 3 and 12 months. Long-term outcomes were analyzed with Kaplan–Meier statistics.
Results
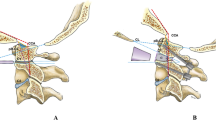
Patients with (n = 31) or without (n = 38) ventral compression were distinguished. 25 patients declined an operation, while 44 patients underwent 48 operations. Surgical management depended on the presence of ventral compression and segmentation anomalies between occiput and C3, signs of instability and presence of caudal cranial nerve dysfunctions. 16 patients without ventral compression underwent foramen magnum decompressions without fusion. 19 patients with ventral compression and abnormalities of segmentation or evidence of instability underwent a foramen magnum decompression with craniocervical (n = 18) or C1/2 (n = 1) stabilization. In nine patients with severe ventral compression and caudal cranial nerve deficits, a transoral resection of the odontoid was combined with a posterior decompression and fusion. Within the first postoperative year neurological scores improved for all symptoms in each patient group. In the long-term, postoperative deteriorations were related exclusively to instabilities either becoming manifest after a foramen magnum decompression in three or as a result of hardware failures in two patients.
Conclusions
The great majority of patients with basilar invagination report postoperative improvements with this management algorithm. Most patients without ventral compression can be managed by foramen magnum decompression alone. The majority of patients with ventral compression can be treated by posterior decompression, realignment and stabilization alone, reserving anterior decompressions for patients with profound, symptomatic brainstem compression.




Similar content being viewed by others
References
Menezes AH, VanGilder JC, Graf CJ, McDonnell DE (1980) Craniocervical abnormalities. A comprehensive surgical approach. J Neurosurg 53:444–455
Goel A (2004) Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine 1:281–286
Klekamp J, Samii M (1993) Introduction of a score system for the clinical evaluation of patients with spinal processes. Acta Neurochir (Wien) 123:221–223
Klekamp J (2012) Surgical treatment of Chiari I malformation–analysis of intraoperative findings, complications, and outcome for 371 foramen magnum decompressions. Neurosurgery 71:365–380. doi:10.1227/NEU.0b013e31825c3426 (discussion 380)
Klekamp J, Batzdorf U, Samii M, Bothe HW (1996) The surgical treatment of Chiari I malformation. Acta Neurochir (Wien) 138:788–801
Klekamp J, Samii M (2001) Syringomyelia—diagnosis and treatment. Springer Verlag, Heidelberg
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Menezes AH (2008) Craniocervical developmental anatomy and its implications. Childs Nerv Syst 24:1109–1122
Milhorat TH, Chou MW, Trinidad EM, Kula RW, Mandell M, Wolpert C, Speer MC (1999) Chiari I malformation redefined: clinical and radiographic findings for 364 symptomatic patients. Neurosurgery 44:1005–1017
Ali MM, Russell N, Awada A, McLean D (1996) A cranio-cervical malformation presenting as acute respiratory failure. J Emerg Med 14:569–572
Goel A, Shah A (2009) Reversal of longstanding musculoskeletal changes in basilar invagination after surgical decompression and stabilization. J Neurosurg Spine 10:220–227
Dickman CA, Kalani MY (2012) Resolution of cervical syringomyelia after transoral odontoidectomy and occipitocervical fusion in a patient with basilar invagination and Type I Chiari malformation. J Clin Neurosci 19:1726–1728. doi:10.1016/j.jocn.2012.04.006
Menezes AH (2012) Craniovertebral junction abnormalities with hindbrain herniation and syringomyelia: regression of syringomyelia after removal of ventral craniovertebral junction compression. J Neurosurg 116:301–309. doi:10.3171/2011.9.jns11386
Joseph V, Rajshekhar V (2003) Resolution of syringomyelia and basilar invagination after traction. Case illustration. J Neurosurg Spine 98:298
Hwang SW, Heilman CB, Riesenburger RI, Kryzanski J (2008) C1-C2 arthrodesis after transoral odontoidectomy and suboccipital craniectomy for ventral brain stem compression in Chiari I patients. Eur Spine J 17:1211–1217
Jian FZ, Chen Z, Wrede KH, Samii M, Ling F (2010) Direct posterior reduction and fixation for the treatment of basilar invagination with atlantoaxial dislocation. Neurosurgery 66:678–687 (discussion 687)
Collignon FP, Cohen-Gadol AA, Krauss WE (2004) Circumferential decompression of the foramen magnum for the treatment of syringomyelia associated with basilar invagination. Neurosurg Rev 27:168–172
Goel A, Bhatjiwale M, Desai K (1998) Basilar invagination: a study based on 190 surgically treated patients. J Neurosurg 88:962–968
Bollo RJ, Riva-Cambrin J, Brockmeyer MM, Brockmeyer DL (2012) Complex Chiari malformations in children: an analysis of preoperative risk factors for occipitocervical fusion. J Neurosurg Pediatr 10:134–141. doi:10.3171/2012.3.peds11340
Simsek S, Yigitkanli K, Belen D, Bavbek M (2006) Halo traction in basilar invagination: technical case report. Surg Neurol 66:311–314 (discussion 314)
Dahdaleh NS, Dlouhy BJ, Menezes AH (2012) Application of neuromuscular blockade and intraoperative 3D imaging in the reduction of basilar invagination. J Neurosurg Pediatr 9:119–124. doi:10.3171/2011.11.peds11332
Peng X, Chen L, Wan Y, Zou X (2011) Treatment of primary basilar invagination by cervical traction and posterior instrumented reduction together with occipitocervical fusion. Spine (Phila Pa 1976) 36:1528–1531. doi:10.1097/BRS.0b013e3181f804ff
Goel A, Shah A (2008) Atlantoaxial joint distraction as a treatment for basilar invagination: a report of an experience with 11 cases. Neurol India 56:144–150
Botelho RV, Neto EB, Patriota GC, Daniel JW, Dumont PA, Rotta JM (2007) Basilar invagination: craniocervical instability treated with cervical traction and occipitocervical fixation. Case report. J Neurosurg Spine 7:444–449
Kim LJ, Rekate HL, Klopfenstein JD, Sonntag VK (2004) Treatment of basilar invagination associated with Chiari I malformations in the pediatric population: cervical reduction and posterior occipitocervical fusion. J Neurosurg 101:189–195
Salunke P, Behari S, Kirankumar MV, Sharma MS, Jaiswal AK, Jain VK (2006) Pediatric congenital atlantoaxial dislocation: differences between the irreducible and reducible varieties. J Neurosurg 104:115–122
Kaibara T, Hurlbert RJ, Sutherland GR (2001) Intraoperative magnetic resonance imaging-augmented transoral resection of axial disease. Neurosurg Focus 10:E4
Gladi M, Iacoangeli M, Specchia N, Re M, Dobran M, Alvaro L, Moriconi E, Scerrati M (2012) Endoscopic transnasal odontoid resection to decompress the bulbo-medullary junction: a reliable anterior minimally invasive technique without posterior fusion. Eur Spine J 21(Suppl 1):S55–S60. doi:10.1007/s00586-012-2220-4
Scholtes F, Signorelli F, McLaughlin N, Lavigne F, Bojanowski MW (2011) Endoscopic endonasal resection of the odontoid process as a standalone decompressive procedure for basilar invagination in Chiari type I malformation. Minim Invasive Neurosurg 54:179–182
Goel A (2005) Progressive basilar invagination after transoral odontoidectomy: treatment by atlantoaxial facet distraction and craniovertebral realignment. Spine 30:E551–E555
Mouchaty H, Perrini P, Conti R, Di Lorenzo N (2009) Craniovertebral junction lesions: our experience with the transoral surgical approach. Eur Spine J 18(Suppl 1):13–19
Naderi S, Pamir MN (2001) Further cranial settling of the upper cervical spine following odontoidectomy. Report of two cases. J Neurosurg Spine 95:246–249
Daniel RT, Muzumdar A, Ingalhalikar A, Moldavsky M, Khalil S (2012) Biomechanical stability of a posterior-alone fixation technique after craniovertebral junction realignment. World Neurosurg 77:357–361. doi:10.1016/j.wneu.2011.06.039
Menezes AH (2008) Surgical approaches: postoperative care and complications “transoral-transpalatopharyngeal approach to the craniocervical junction”. Childs Nerv Syst 24:1187–1193
Bagley CA, Witham TF, Pindrik JA, Davis RF, Bydon A, Gokaslan ZL, Wolinsky JP (2009) Assuring optimal physiologic craniocervical alignment and avoidance of swallowing-related complications after occipitocervical fusion by preoperative halo vest placement. J Spinal Disord Tech 22:170–176. doi:10.1097/BSD.0b013e318168be6f
Miyata M, Neo M, Fujibayashi S, Ito H, Takemoto M, Nakamura T (2009) O-C2 angle as a predictor of dyspnea and/or dysphagia after occipitocervical fusion. Spine (Phila Pa 1976) 34:184–188. doi:10.1097/BRS.0b013e31818ff64e
Yoshida M, Neo M, Fujibayashi S, Nakamura T (2007) Upper-airway obstruction after short posterior occipitocervical fusion in a flexed position. Spine (Phila Pa 1976) 32:E267–E270. doi:10.1097/01.brs.0000259977.69726.6f
Matsunaga S, Onishi T, Sakou T (2001) Significance of occipitoaxial angle in subaxial lesion after occipitocervical fusion. Spine (Phila Pa 1976) 26:161–165
Arora P, Behari S, Banerji D, Chhabra DK, Jain VK (2004) Factors influencing the outcome in symptomatic Chiari I malformation. Neurol India 52:470–474
Aghakhani N, Parker F, David P, Morar S, Lacroix C, Benoudiba F, Tadie M (2009) Long-term follow-up of Chiari-related syringomyelia in adults: analysis of 157 surgically treated cases. Neurosurgery 64:308–315. doi:10.1227/01.neu.0000336768.95044.80 (discussion 315)
Nockels RP, Shaffrey CI, Kanter AS, Azeem S, York JE (2007) Occipitocervical fusion with rigid internal fixation: long-term follow-up data in 69 patients. J Neurosurg Spine 7:117–123
Plotz GM, Schutz U, Grob D (1998) Dorsal occipitocervical fusion—indications and results. Z Orthop Ihre Grenzgeb 136:364–374
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Klekamp, J. Treatment of basilar invagination. Eur Spine J 23, 1656–1665 (2014). https://doi.org/10.1007/s00586-014-3423-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3423-7