Abstract
Purpose
The purpose of this study was to examine radiographic and clinical outcomes in the treatment of adult degenerative scoliosis using a minimally invasive (MI) lateral approach for anterior lumbar interbody fusion (IBF).
Methods
A prospective study of 24 consecutive degenerative scoliosis patients treated with MI, 90° lateral, transpsoas approach for anterior IBF was conducted. Twenty-one patients (88 %) were available for at least 12 months follow-up (mean 24 months).
Results
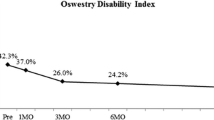
Mean operating time, estimated blood loss, and length of stay was 218 min, 68 mL, and 2.2 days, respectively. Complications occurred in one (5 %) case, a postoperative foot drop. At the last follow-up, disability improved by 50 % from 48.4 to 24.4. Back pain improved by 59 % from 7.0 to 2.9. Leg pain improved by 41 % from 5.6 to 3.3. In patients with a baseline score greater than 2.0, leg pain decreased by 42 % from 6.6 to 3.8. SF-36 physical component score improved by 41 % from 28.0 to 39.6, while mental component score increased by 18 % from 42.2 to 49.8. All changes were statistically significant, p < 0.05. Cobb angle was corrected from 27.7° to 16.6° and lumbar lordosis increased 39 % from −31.8° to −44.0°. Disc height increased from 5.7 to 11.6 mm, segmental lordosis increased by 48 % from 11.6° to 17.2°, and foraminal height increased from 16.4 to 21.7 mm. At the last follow-up, 100 % of patients were satisfied with their outcome, and 86 % would undergo the same procedure again. No revisions occurred.
Conclusions
MI lateral IBF in the treatment of degenerative scoliosis results in lower complication rates and clinical and radiographic outcomes equivalent to reports in the literature of conventional approaches.






Similar content being viewed by others
References
Aebi M (2005) The adult scoliosis. Eur Spine J 14:925–948
Grubb SA, Lipscomb HJ (1992) Diagnostic findings in painful adult scoliosis. Spine (Phila Pa 1976) 17:518–527
Smith JS, Shaffrey CI, Berven S et al (2009) Improvement of back pain with operative and nonoperative treatment in adults with scoliosis. Neurosurgery 65:86–93
Swank SM (1979) The management of scoliosis in the adult. Orthop Clin North Am 10:891–904
Schwab F, Dubey A, Gamez L et al (2005) Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976) 30:1082–1085
Wang MY, Mummaneni PV (2010) Minimally invasive surgery for thoracolumbar spinal deformity: initial clinical experience with clinical and radiographic outcomes. Neurosurg Focus 28:E9
Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 30:682–688
Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy JP, Pagala M (2002) Adult scoliosis: a quantitative radiographic and clinical analysis. Spine (Phila Pa 1976) 27:387–392
Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG (2007) The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 32:2764–2770
Smith JS, Sansur CA, Donaldson WF III et al (2011) Short-term morbidity and mortality associated with correction of thoracolumbar fixed sagittal plane deformity: a report from the scoliosis research society morbidity and mortality committee. Spine (Phila Pa 1976) 36:958–964
Sansur CA, Smith JS, Coe JD et al (2011) Scoliosis research society morbidity and mortality of adult scoliosis surgery. Spine (Phila Pa 1976) 36:E593–E597
Schwab FJ, Lafage V, Farcy JP, Bridwell KH, Glassman S, Shainline MR (2008) Predicting outcome and complications in the surgical treatment of adult scoliosis. Spine (Phila Pa 1976) 33:2243–2247
Isaacs RE, Hyde J, Goodrich JA, Rodgers WB, Phillips FM (2010) A prospective, nonrandomized, multicenter evaluation of extreme lateral interbody fusion for the treatment of adult degenerative scoliosis: perioperative outcomes and complications. Spine (Phila Pa 1976) 35:S322–S330
Swank S, Lonstein JE, Moe JH, Winter RB, Bradford DS (1981) Surgical treatment of adult scoliosis. A review of two hundred and twenty-two cases. J Bone Joint Surg Am 63:268–287
Smith JS, Shaffrey CI, Berven S et al (2009) Operative versus nonoperative treatment of leg pain in adults with scoliosis: a retrospective review of a prospective multicenter database with two-year follow-up. Spine (Phila Pa 1976) 34:1693–1698
Glassman SD, Carreon LY, Shaffrey CI et al (2010) The costs and benefits of nonoperative management for adult scoliosis. Spine (Phila Pa 1976) 35:578–582
Dakwar E, Cardona RF, Smith DA, Uribe JS (2010) Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg Focus 28:E8
Smith WD, Youssef JA, Christian G, Serrano S, Hyde JA (2012) Lumbarized sacrum as a relative contraindication for lateral transpsoas interbody fusion at L5–6. J Spinal Disord Tech 25:285–291
Pumberger M, Hughes AP, Huang RR, Sama AA, Cammisa FP, Girardi FP (2012) Neurologic deficit following lateral lumbar interbody fusion. Eur Spine J 21:1192–1199
Kepler CK, Bogner EA, Herzog RJ, Huang RC (2011) Anatomy of the psoas muscle and lumbar plexus with respect to the surgical approach for lateral transpsoas interbody fusion. Eur Spine J 20:550–556
Shamji MF, Isaacs RE (2008) Anterior-only approaches to scoliosis. Neurosurgery 63:139–148
Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH (2007) Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976) 32:2238–2244
Anand N, Baron EM, Thaiyananthan G, Khalsa K, Goldstein TB (2008) Minimally invasive multilevel percutaneous correction and fusion for adult lumbar degenerative scoliosis: a technique and feasibility study. J Spinal Disord Tech 21:459–467
Anand N, Rosemann R, Khalsa B, Baron EM (2010) Mid-term to long-term clinical and functional outcomes of minimally invasive correction and fusion for adults with scoliosis. Neurosurg Focus 28:E6
Mundis GM, Akbarnia BA, Phillips FM (2010) Adult deformity correction through minimally invasive lateral approach techniques. Spine (Phila Pa 1976) 35:S312–S321
Ozgur BM, Agarwal V, Nail E, Pimenta L (2010) Two-year clinical and radiographic success of minimally invasive lateral transpsoas approach for the treatment of degenerative lumbar conditions. SAS J 1:41–46
Tormenti MJ, Maserati MB, Bonfield CM, Okonkwo DO, Kanter AS (2010) Complications and radiographic correction in adult scoliosis following combined transpsoas extreme lateral interbody fusion and posterior pedicle screw instrumentation. Neurosurg Focus 28:E7
Berjano P, Lamartina C (2013) Far lateral approaches (XLIF) in adult scoliosis. Eur Spine J 22(Suppl 2):S242–S253
Phillips FM, Isaacs RE, Rodgers WB, Khajavi K, Tohmeh AG, Deviren V, Peterson MD, Hyde J, Kurd M (2013) Adult degenerative scoliosis treated with XLIF: clinical and radiographic results of a prospective multicenter study with 24-month follow-up. Spine (Phila Pa 1976) 38:1853–1861
Conflict of interest
Nuvasive Inc: consultant honoraria/travel only.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khajavi, K., Shen, A.Y. Two-year radiographic and clinical outcomes of a minimally invasive, lateral, transpsoas approach for anterior lumbar interbody fusion in the treatment of adult degenerative scoliosis. Eur Spine J 23, 1215–1223 (2014). https://doi.org/10.1007/s00586-014-3246-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3246-6