Abstract
Objective
The optimal timing of stabilization in patients with traumatic thoracolumbar fractures remains controversial. There is currently a lack of consensus on the timing of surgical stabilization, which is limited by the reality that a randomized controlled trial to evaluate early versus late stabilization is difficult to perform. Therefore, the objective of this study was to determine the benefits, safety and costs of early stabilization compared with late stabilization using data available in the current literature.
Methods
An electronic literature search was performed in Medline, Embase, Cochrane Database of Systematic Reviews, and Cochrane Central Register of Controlled Trials for relevant studies evaluating the timing of surgery in patients with thoracolumbar fractures. Two reviewers independently analyzed and selected each study on the basis of the eligibility criteria. The quality of the included studies was assessed using the Grading of Recommendations Assessment, Development, and Evaluation system (GRADE). Any disagreements were resolved by consensus.
Results
Ten studies involving 2,512 subjects were identified. These studies demonstrated that early stabilization shortened the hospital length of stay, intensive care unit length of stay, ventilator days and reduced morbidity and hospital expenses for patients with thoracic fractures. However, reduced morbidity and hospital expenses were not observed with stabilization of lumbar fractures. Owing to the very low level of evidence, no conclusion could be made regarding the effect of early stabilization on mortality.
Conclusions
We could adhere to the recommendation that patients with traumatic thoracolumbar fractures should undergo early stabilization, which may reduce the hospital length of stay, intensive care unit length of stay, ventilator days, morbidity and hospital expenses, particularly when the thoracic spine is involved. Individual patient characteristics should be concerned carefully. However, the definite conclusion cannot be made due to the heterogeneity of the included studies and low level of evidence. Further prospective studies are required to confirm whether there are benefits to early stabilization compared with late stabilization.
Similar content being viewed by others
Introduction
The timing of surgery in patients with traumatic thoracolumbar fractures, with or without spinal cord injury (SCI), remains controversial. There are several advantages to early surgery in patients with thoracolumbar fractures. Quicker patient mobilization with shorter hospital stays and a lower incidence of thromboembolic and pulmonary complications are two major benefits [5, 6]. Early mobilization is also thought to decrease mortality and morbidity, which is described in the evolution of the management of femur fractures. However, early surgery may be associated with hypotension, increased neurological complications and operative hemorrhages. Other potential disadvantages include operating in a setting of potentially missed or underestimated multiple injuries, operating without a full understanding of the overall injury, and operating under non-ideal conditions relative to the complexity of the surgery and resources required. Later surgery avoids the above complications or disadvantages and allows for surgical intervention under more controlled conditions.
Currently, there have been no adequate studies that investigate whether the timing of surgery affects surgical outcomes. Although several retrospective studies have reported that early surgery was associated with a lower incidence of complications and a decreased hospital length of stay (HLOS), these studies exhibited methodological deficits and a higher risk of bias because of poor study design. The underlying problem is the difficulty in the design and execution of a randomized controlled trial to determine the clinical outcomes and complications because of the ethical concerns and logistics of scheduling a major spine surgery in an urgent manner [3].
The purpose of this systematic review was to evaluate the benefits, safety and costs of early stabilization compared with late stabilization after traumatic thoracolumbar fractures, with or without SCI, and to evaluate the evidence according to the GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) system. This will provide a foundation of evidence from which a clinical decision may be made to guide the surgeon and to determine the optimal timing of surgery.
Materials and methods
Search strategy and eligibility criteria
An electronic search using the keywords thoracolumbar, thoracic or lumbar, spine or spinal, trauma and surgery was performed in Medline, Embase, Sciencedirect, Cochrane Database of Systematic Reviews, and Cochrane Central Register of Controlled Trials through June 2012. Manual searches were performed in addition to the electronic search for the reference lists of all of the retrieved articles. Moreover, all of the relevant conference databases, which provide gray literature, were also searched. In studies where there were overlapping patients and the criteria included the hospital, study period, and participation information, we retained only the largest study to avoid any duplication of information. In addition, the selected studies had to compare the early with late surgical stabilization in adult patients (≥18 years) with traumatic thoracolumbar fractures. Owing to time, the early surgery was described as ranging between 8 and 72 h [4, 11, 14, 15]. Studies that defined early surgery as greater than 72 h were excluded. Exclusion criteria included cervical fractures, a sample size <10 in each treatment group and studies without sufficient outcome data. Articles published in languages other than English were also excluded.
Study selection
Two reviewers (DX and JXM) independently analyzed each title and abstract on the basis of the eligibility criteria and then met to discuss any discrepancies. Articles that were not excluded from our study on the basis of the title and abstract were independently retrieved for full-text review by the same two reviewers.
Data extraction
The two independent reviewers (DX and JXM) extracted data from the qualifying articles. A previously piloted data extraction form was used to record information regarding the population, study design, sample size, spine segment, the number of ventilator (VENT) days, HLOS, intensive care unit of stay (ICULOS), respiratory complications, morbidity, mortality and in-hospital costs. The corresponding author of each study was then contacted to obtain any additional information that was required. In the case of discrepancies, a third reviewer (JW) was involved.
Methodological quality and rating the evidence of each article
The quality of the studies was independently assessed by two authors (JXM and YC). The method used to evaluate the quality of evidence of the individual studies and the overall quality of the body of evidence incorporated aspects of the rating scheme developed by the Oxford Centre for Evidence-based Medicine [18], which was used with modifications by The Journal of Bone and Joint Surgery American Volume (J Bone Joint Surg Am) [23], with precepts outlined by the Grades of Recommendation Assessment, Development and Evaluation (GRADE) Working Group [1] and with recommendations made by the Agency for Healthcare Research and Quality (AHRQ) [22]. Each included study was rated against prior criteria that were classified into four levels (level of evidence I, II, III, and IV) for each of the four different study types (i.e., therapeutic, prognostic, diagnostic, and economic or decision modeling). The basic principle behind the level of evidence was that some articles were more influential than others based solely on the nature of their study design because improved study methods decreased the potential for error and minimized the sources of bias [21]. Previous studies have shown that a higher level of evidence is associated with increased rates of citation in orthopedic literature [16]. Furthermore, the concept of the level of evidence has recently gained widespread acceptance in the orthopedic community. A third author (XLM) was the adjudicator when conflicting evaluations were needed to be resolved.
Analysis
We pooled the number of VENT days, HLOS, ICULOS, respiratory complications, hospital expenses and mortality cases. A qualitative analysis [20] was performed considering the following three domains: quality of studies, quantity of studies and consistency of results across the studies [22]. The quality of studies is associated with the level of evidence, which has been described above. The quantity of studies is defined by the number of published studies that are similar in population, outcome and medical condition. The consistency refers to whether the results of the different studies lead to a similar conclusion (similar values and in the same direction). We judged whether the body of literature represented a minimum standard for each of the three domains using the following criteria: for study quality, at least 80 % of the studies reported were required to be rated as a level of evidence I or II; for the study quantity, at least three published studies were needed that were adequately powered to answer the study question; and for study consistency, at least 70 % of the studies were required to have consistent results. The definition of the overall strength of the evidence is presented in Table 1, which used the concepts obtained from the GRADE Working Group [1]. An overall strength of “high” meant that “further research is very unlikely to change our confidence in the estimate of the effect.” The overall strength of “moderate” meant that “further research is likely to have an important impact on our confidence in the estimate of the effect.” However, an overall strength of evidence rating of “low” meant that “further research is very likely to have an important impact on our confidence in the estimate of the effect and is likely to change the estimate.” Moreover, “very low” meant that “any estimate of the effect is very uncertain.”
Results
Study identification
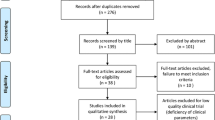
On the basis of our research, we identified 1,160 potential citations after the duplications were excluded. After screening of the citation titles and abstracts, we identified 98 publications for full-text reading. On the basis of the full-text screening, 10 studies that provided a comparison of early versus late thoracolumbar fracture stabilization were included in the present review. The most frequent reason for exclusion was the inclusion of only cervical fractures or the absence of stratification for results by spine level. Figure 1 depicts the flow diagram of the selection process for relevant studies.
Study characteristics included in the analysis
The characteristics of the studies are presented in Table 2. A total of 10 studies [2, 4–6, 8, 10–12, 15, 19] were included, consisting of 2,512 patients with thoracolumbar fractures. These articles were published between 1999 and 2012. The number of total study subjects ranged from 27 [4, 15] to 1,126 [2]. All of the investigations compared early and late surgical stabilization in adult patients with traumatic thoracolumbar fractures. The majority of the studies used 72 h as the separation time point between early and late intervention. In addition, there were 2 studies that used 24 or 8 h to separate early versus late surgery. Half of the included studies reported whether the patients were with or without SCI.
Quality assessment
The results of the study quality assessment are presented in Table 2. Two studies [2, 4] were graded as level II, whereas the remaining eight studies were graded as level III. Only one study [4] was a quasi-randomized controlled trial. One observational study [15] was a prospective cohort study, and the remaining eight studies were retrospective cohort studies. Although the quasi-randomized controlled trial was single-blinded to the evaluators, it did not have a concealed sequence allocation and had used an inaccurate randomized method. The prospective cohort study lacked an independent assessment of complications and did not control for potential confounding factors. Propensity score modeling (PSM) was applied in one retrospective study to mitigate imbalances in variables known to be associated with an assignment for an intervention, which offsets any confounding factors between the treatment groups and improved the comparison of outcomes.
Clinical outcomes
The outcome parameters available and evaluated in each of the ten studies are summarized in Table 3. Conclusions from each study are summarized in Table 4. Nine of the studies reported the HLOS. Four of the nine studies [6, 10–12] presented data for thoracic and lumbar fractures, one study [19] included only thoracic fractures, and two studies [4, 5] included only thoracolumbar fractures and divided the patients into subgroups according to injury severity score (ISS). One study [8] divided all of the patients into an early and a late group with comparable ISS, equal laboratory parameters at admission, and comparable demographics. The mean HLOS with thoracic fractures ranged from 10.1 to 38.3 days in the early group compared with 14.4 to 42.6 days in the late group. The mean HLOS with lumbar fractures ranged from 9.4 to 33.8 days in the early group compared with 14.1 to 36.4 days in the late group. The range of the mean HLOS with thoracic/lumbar/thoracolumbar was 8.1 to 70 days in the early group compared with 15 to 108 days in the late group. The HLOS was significantly lower in the early group compared with the late group in all of the included studies. However, some of these studies reported that the ICULOS was significantly lower in the early group than in the late group. Six studies reported the VENT days for thoracic, lumbar or thoracolumbar fractures. In three of the included studies [6, 12, 19], the patients with thoracic fractures had significantly lower VENT days in the early group, as presented in Table 3. Frangen et al. [8] reported that patients with thoracic, lumbar or thoracolumbar fractures have significantly lower VENT days in the early group compared to patients with ISS (26–37), as well as less complete paraplegia or preoperative lung failure. There was no significant difference in the VENT days in patients with lumbar fractures only.
The rate of morbidity as measured by the incidence of respiratory complications and mortality are also presented in Table 3. Seven out of all of the included studies reported the incidence of respiratory complications. Four studies [2, 6, 11, 19] reported that patients with thoracic fractures had a lower rate of respiratory complications in the early group. Kerwin et al. [11] identified a significantly lower incidence of respiratory complications in patients with SCI with thoracic fractures. However, there was no significant difference in the incidence of respiratory complications in patients with lumbar or thoracolumbar fractures only. The mean mortality varied among studies that ranged in thoracic fractures from 0 to 11.1 % in the early group compared with 0 to 17 % in the late group. There was only one study that reported a statistically lower rate of mortality in the early group than the late group (6.2 vs. 17 %) [19]. When stratified by ISS, those in the early group continued to have a lower rate of mortality despite injury severity. However, a study by Kerwin et al. [10] reported that there was a slightly higher rate of mortality in patients with thoracic fractures treated within 48 h compared with those treated after 48 h (5.6 vs. 0 %), but this did not reach statistical significance. Another study conducted by Kerwin et al. [11] in 2005 compared patients with thoracic fractures, with or without SCI, using 72 h as a separation time point for early and late surgeries. There were no deaths reported in patients with SCI. In the subgroup without SCI, a slightly higher rate of mortality was found in the early group, but with no significant difference (11.1 vs. 0 %). These findings indicated that early surgery might be associated with higher mortality. In a later study in 2008, Kerwin et al. [12] reported that there were no deaths in patients with thoracic fractures after reviewing 245 patients from a trauma database. There was no significant difference in mortality between the early and late groups in four studies investigating lumbar fractures only, in one study focused on thoracolumbar fractures, or in three studies reporting on thoracic, lumbar, and thoracolumbar fractures.
Three studies [2, 6, 12] included data on the costs of surgery for patients. One of the three studies [6] demonstrated lower costs for patients with thoracic fractures undergoing early surgery compared with late surgery. Boakye et al. [2] reported that patients with thoracic/thoracolumbar fractures had significantly lower costs in early stabilization after reviewing 1,126 patients from an inpatient database. However, there were no significant differences in the hospital expenses between the groups in two studies that examined lumbar fractures.
Evidence summary and recommendation strengths
The overall strength of evidence to assess whether early surgery in thoracolumbar fractures reduces HLOS, ICULOS, and VENT days is “high” such that the estimate of the effect is very certain. However, the overall strength of evidence to assess whether early surgery reduces in-hospital costs and morbidity is “moderate” such that further research is likely to have an important impact on our confidence in the estimate of the effect. The overall strength of evidence to assess mortality is “very low” of which the estimate of the effect is very uncertain. Therefore, these findings may lower the confidence in recommendations.
Discussion
The optimal timing of surgical stabilization of thoracolumbar injuries, whether early or late, remains controversial, particularly because major traumatic thoracolumbar fractures are commonly associated with polytrauma. Removal of damaged bone, disk and ligament fragments that decompress the swollen spinal cord limits secondary injury and improves the outcome. Several studies have evaluated the neurological outcome, but there is no consensus on the timing of surgery. The timing of stabilization is usually classified as early (<72 h) or late (>72 h). Although early stabilization has been described as ranging anywhere from 8 to 72 h, the 72-h stratification point is based on preclinical studies, which demonstrated that early decompression of acute SCI results in improved neurological recovery [9]. However, there is no clear evidence to support early surgery in decreased mortality and morbidity. A prospective randomized controlled trial on thoracic fractures showed that there was no significant difference in mortality and morbidity [4]. Therefore, we performed a systematic review aimed toward contributing to the planning of the optimal timing and effect of this time interval on the HLOS, ICULOS, VENT days, hospital expenses, morbidity, and mortality.
The shorter HLOS, ICULOS, and VENT days in the early group may be partly attributed to the study design in that the late group, by definition, had a longer hospitalization stay. Moreover, these shorter times may be preserved by avoiding complications, quick recovery, and treatments. A significant large number of late surgery patients required ventilator support for noninfectious reasons, which may reflect the need to sedate and control patients to support additional injuries. The use of ventilator support may increase the risk of pneumonia and may be one factor that increases the risk of respiratory complications in the late group.
From the present systematic review, patients with early surgery had a lower incidence of respiratory complications and shorter ICULOS and HLOS, which resulted in lower hospital expenses. This was a clear advantage for spinal stabilization within 72 h of injury. Moreover, earlier patient mobilization and its advantages to overall patient care were achieved by early stabilization, resulting in lower rates of pneumonia and less resource utilization. In particular, it was extremely significant in patients with pulmonary injuries. However, much of the controversy in the treatment of thoracolumbar fractures originates from inadequate knowledge regarding the pathophysiology of the disease as well as the timing of specific treatments. Kerwin et al. [10] reported that early surgery of thoracic fractures can result in higher mortality, but without exhibiting a significant difference. Croce et al. [6] found a significantly higher mortality in patients with ISS >25 who underwent early spine fixation. This may indicate that proper surgical time and careful consideration of each individual patient’s condition by the surgeon are very important. Pape et al. [17] suggested that early spinal stabilization may not be appropriate for all patients. Severely injured patients may receive an initial injury followed by surgery, which may amplify their previous injuries. The surgery may come too early, adding stimulation to the already activated inflammatory cascade, which may result in deterioration and subsequent increased mortality. Therefore, ISS, in the most included studies, was higher in the late group than in the early group, which may affect patients’ needing on HLOS, ICULOS, VENT days. Furthermore, deaths may still be related to ongoing impairment of immune function resulting from spinal fractures that are difficult to detect during the early period after injury. Kerwin et al. [10] suggested that better recognition of patients with persistent acidosis and inadequate organ perfusion and patients on whom early stabilization should not be performed will improve the outcome and reduce mortality.
Although most fractures were in the thoracolumbar (T11–L2) area, several included studies performed their analysis separately according to the lumbar and thoracic area. However, several included studies did not divide their patients into a thoracic and lumbar group. As a transitional area, there may be no difference in optimal timing for surgery in T12 and L1. Therefore, it may be inappropriate to divide the fracture area into thoracic and lumbar, which might not be applied in all patients with thoracolumbar fractures.
For patients who are neurologically intact, immediate early surgery to stabilize the patient is very attractive. However, for patients who are not neurologically normal, some surgeons fear that some factors, such as operative stress, blood gas changes and hypotension, might worsen neurological injury. Surgeons are very eager for patients to be stabilized prior to surgery, which may postpone the surgery date. Magerl [13] considered only the presence of a partial or progressive neurological lesion as an unstable condition and treated the lesion by spinal stabilization after decompression of neurological elements. Fehlings et al. [7] reported that decompression early after SCI may be performed safely and is associated with improved neurological outcome in patients with cervical SCI. However, the timing of surgical decompression after an SCI remains a controversial topic. Clinical signs after thoracolumbar fractures with SCI may depend on the location of the lesion and the amount of damage to the gray and white matter. Furthermore, several included studies of the present review did not report whether the patients were with or without SCI. Many factors, such as morbidity, mortality, pulmonary condition and physical recovery, were also affected by the presence or absence of neurological injury. Therefore, the patients with or without neurological injury of the included studies might influence the effect size of the outcomes. Although it is better to analyze patients separately with or without SCI, it was unrealistic to collect individual patient characteristics from the included studies.
To a certain degree, the difference of HLOS between early and late surgery seems to be affected by a delay of surgery. Late surgery may result in the prolongation of HLOS directly. Patients without SCI or with low ISS may also be operated lately. Additionally, the timing of surgery may depend on different indications for different surgical approaches and on subjective factors of patients and surgeons. Therefore, the HLOS, which could be easily affected by various confounding factors, may not be an impressive outcome. In a similar way, VENT days may also be affected by ISS and SCI. Patients with severe injuries or with SCI mostly need more VENT days before or after surgery. Hence, selection bias for patients may exert an influence on the accuracy of summarized results, especially in the non-randomized controlled trials.
The limitations of this systematic review primarily include the following: (1) The information obtained from the medical record review did not identify differences in patient groups as an unidentified reason for delaying surgery. (2) Only one quasi-randomized controlled trial was identified in the systematic review. Most of the included studies were a retrospective evaluation of prospectively collected registry data that limited the examination of confounding factors that may have affected the mortality and morbidity. These include the presence of associated injuries, patient baseline medical comorbidities, patients with or without SCI, ISS and surgeon or operation room scheduling conflicts. (3) The registry data may be subject to bias, which affects their internal validity. Furthermore, a specific institution’s clinical volume affects the patient outcomes. (4) Selection biases were introduced in the present review because the database was regional and different hospitals applied different indications for early surgery and criteria for inclusion or exclusion. (5) As confounding factors, associated injuries, neurologic impairment, ISS with or without SCI in patients of the included studies may exert an influence on the homogeneity of the present systematic review. Furthermore, some variables, such as HLOS and data costs of surgery, may be affected by different economic conditions of different regions or countries, which may exert influence on the homogeneity of the included studies.
Despite the above limitations, this review has made a significant contribution in evaluating the timing of surgical intervention in patients with traumatic thoracolumbar fractures. The results of the review represent the best available literature, which suggest that early stabilization most likely decreases complications, facilitates early rehabilitation, decreases hospital expenses, and reduces HLOS, ICULOS, and VENT days. However, no comments can be made about mortality from the present review, as it exhibited a “very low” level of evidence.
Conclusion
This systematic review provided an overview of the current knowledge regarding the timing of stabilization for patients with thoracolumbar fractures. Early surgery may shorten the HLOS, ICULOS, and VENT days for patients with thoracolumbar fractures. Furthermore, early stabilization may also reduce morbidity and hospital expenses when the thoracic spine is involved. However, the present review does not provide evidence that early stabilization of lumbar fractures exhibits benefits other than fewer HLOS, ICULOS and VENT days. Owing to the very low level of evidence, no conclusion can be made in terms of the effect of early stabilization on mortality. Therefore, we could adhere to the recommendation that patients with traumatic thoracolumbar fractures may undergo surgery prior to 72 h to reduce HLOS, ICULOS, VENT days, hospital expenses, morbidity, or potentially mortality, particularly when the thoracic spine is involved. Owing to the underlying heterogeneity of the included studies, the exact conclusion of the present systematic review cannot be made based on the present evidence. Because randomized controlled trials in injured patients are ethically not suitable for investigative study, further prospective and homogeneous studies are required to confirm whether there is a benefit of early stabilization compared with late stabilization.
References
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D, Hill S, Jaeschke R, Leng G, Liberati A, Magrini N, Mason J, Middleton P, Mrukowicz J, O’Connell D, Oxman AD, Phillips B, Schunemann HJ, Edejer TT, Varonen H, Vist GE Jr, Williams JW, Zaza S (2004) Grading quality of evidence and strength of recommendations. BMJ 328:1490. doi:10.1136/bmj.328.7454.1490
Boakye M, Arrigo R, Gephart MG, Zygourakis C, Lad SP (2012) Retrospective, propensity score-matched cohort study examining timing of fracture fixation for traumatic thoracolumbar fractures. J Neurotrauma. doi:10.1089/neu.2012.2364
Carreon LY, Dimar JR (2011) Early versus late stabilization of spine injuries: a systematic review. Spine (Phila Pa 1976) 36:E727–E733. doi:10.1097/BRS.0b013e3181fab02f
Cengiz SL, Kalkan E, Bayir A, Ilik K, Basefer A (2008) Timing of thoracolomber spine stabilization in trauma patients; impact on neurological outcome and clinical course. A real prospective (rct) randomized controlled study. Arch Orthop Trauma Surg 128:959–966. doi:10.1007/s00402-007-0518-1
Chipman JG, Deuser WE, Beilman GJ (2004) Early surgery for thoracolumbar spine injuries decreases complications. J Trauma 56:52–57. doi:10.1097/01.TA.0000108630.34225.85
Croce MA, Bee TK, Pritchard E, Miller PR, Fabian TC (2001) Does optimal timing for spine fracture fixation exist? Ann Surg 233:851–858
Fehlings MG, Vaccaro A, Wilson JR, Singh A, Cadotte DW, Harrop JS, Aarabi B, Shaffrey C, Dvorak M, Fisher C, Arnold P, Massicotte EM, Lewis S, Rampersaud R (2012) Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS One 7:e32037. doi:10.1371/journal.pone.0032037
Frangen TM, Ruppert S, Muhr G, Schinkel C (2010) The beneficial effects of early stabilization of thoracic spine fractures depend on trauma severity. J Trauma 68:1208–1212. doi:10.1097/TA.0b013e3181a0e558
Dimar N Jr, Glassman SD, Raque GH, Zhang YP, Shields CB (1999) The influence of spinal canal narrowing and timing of decompression on neurologic recovery after spinal cord contusion in a rat model. Spine (Phila Pa 1976) 24:1623–1633
Kerwin AJ, Frykberg ER, Schinco MA, Griffen MM, Arce CA, Nguyen TQ, Tepas JR (2007) The effect of early surgical treatment of traumatic spine injuries on patient mortality. J Trauma 63:1308–1313. doi:10.1097/TA.0b013e31815b8361
Kerwin AJ, Frykberg ER, Schinco MA, Griffen MM, Murphy T, Tepas JJ (2005) The effect of early spine fixation on non-neurologic outcome. J Trauma 58:15–21
Kerwin AJ, Griffen MM, Tepas JR, Schinco MA, Devin T, Frykberg ER (2008) Best practice determination of timing of spinal fracture fixation as defined by analysis of the National Trauma Data Bank. J Trauma 65(824–830):830–831. doi:10.1097/TA.0b013e318182af7b
Magerl FP (1984) Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop Relat Res 125–141
McHenry TP, Mirza SK, Wang J, Wade CE, O’Keefe GE, Dailey AT, Schreiber MA, Chapman JR (2006) Risk factors for respiratory failure following operative stabilization of thoracic and lumbar spine fractures. J Bone Joint Surg Am 88:997–1005. doi:10.2106/JBJS.E.00560
McLain RF, Benson (1999) Urgent surgical stabilization of spinal fractures in polytrauma patients. Spine (Phila Pa 1976) 24:1646–1654
Okike K, Kocher MS, Torpey JL, Nwachukwu BU, Mehlman CT, Bhandari M (2011) Level of evidence and conflict of interest disclosure associated with higher citation rates in orthopedics. J Clin Epidemiol 64:331–338. doi:10.1016/j.jclinepi.2010.03.019
Pape HC, Giannoudis P, Krettek C (2002) The timing of fracture treatment in polytrauma patients: relevance of damage control orthopedic surgery. Am J Surg 183:622–629
Phillips B (2004) GRADE: levels of evidence and grades of recommendation. Arch Dis Child 89:489
Schinkel C, Frangen TM, Kmetic A, Andress HJ, Muhr G (2006) Timing of thoracic spine stabilization in trauma patients: impact on clinical course and outcome. J Trauma 61(156–160):160. doi:10.1097/01.ta.0000222669.09582.ec
van Tulder M, Furlan A, Bombardier C, Bouter L (2003) Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa 1976) 28:1290–1299. doi:10.1097/01.BRS.0000065484.95996.AF
Voleti PB, Donegan DJ, Baldwin KD, Lee GC (2012) Level of evidence of presentations at American Academy of Orthopaedic Surgeons annual meetings. J Bone Joint Surg Am 94:e50. doi:10.2106/JBJS.J.01860
West S, King V, Carey TS, Lohr KN, McKoy N, Sutton SF, Lux L (2002) Systems to rate the strength of scientific evidence. Evid Rep Technol Assess (Summ) 1–11
Wright JG, Swiontkowski MF, Heckman JD (2003) Introducing levels of evidence to the journal. J Bone Joint Surg Am 85-A:1–3
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Additional information
D. Xing and Y. Chen contributed equally to this work.
Rights and permissions
About this article
Cite this article
Xing, D., Chen, Y., Ma, JX. et al. A methodological systematic review of early versus late stabilization of thoracolumbar spine fractures. Eur Spine J 22, 2157–2166 (2013). https://doi.org/10.1007/s00586-012-2624-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2624-1