Abstract
Purpose
Due to the disadvantages of iliac crest bone and the poor bone quality of autograft gained from decompression surgery, alternative filling materials for posterior lumbar interbody fusion cages have been developed. β-Tricalcium phosphate is widely used in cages. However, data regarding the fusion rate of β-TCP assessed by computer tomography are currently not available.
Materials
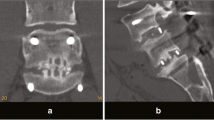
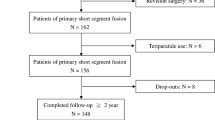
A prospective clinical trial involving 34 patients (56.7 years) was performed: 26 patients were treated with single-level, five patients double-level and three patients triple-level PLIF filled with β-TCP and bone marrow aspirate perfusion, and additional posterior pedicle screw fixation. Fusion was assessed by CT and X-rays 1 year after surgery using a validated fusion scale published previously. Functional status was evaluated with the visual analogue scale and the Oswestry Disability Index before and 1 year after surgery.
Results
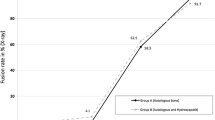
Forty-five levels in 34 patients were evaluated by CT and X-ray with a follow-up period of at least 1 year. Clinically, the average ODI and VAS for leg and back scores improved significantly (P < 0.001). CT assessment revealed solid fusion in 12 levels (26.67 %) and indeterminate fusion in 15 levels (34.09 %). Inadequate fusion (non-union) was detected in 17 levels (38.63 %).
Conclusion
The technique of PLIF using β-TCP yielded a good clinical outcome 1 year after surgery, however, a high rate of pseudoarthrosis was found in this series therefore, we do not recommend β-TCP as a bone graft substitute using the PLIF technique.





Similar content being viewed by others
References
Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES (2006) United States’ trends and regional variations in lumbar spine surgery: 1992–2003. Spine 31(23):2707–2714. doi:10.1097/01.brs.0000248132.15231.fe
Sasso RC, LeHuec JC, Shaffrey C (2005) Iliac crest bone graft donor site pain after anterior lumbar interbody fusion: a prospective patient satisfaction outcome assessment. J Spinal Disord Tech 18(Suppl):S77–S81
Giannoudis PV, Dinopoulos H, Tsiridis E (2005) Bone substitutes: an update. Injury 36(Suppl 3):S20–S27. doi:10.1016/j.injury.2005.07.029
Becker S, Maissen O, Ponomarev I, Stoll T, Rahn B, Wilke I (2006) Osteopromotion by a beta-tricalcium phosphate/bone marrow hybrid implant for use in spine surgery. Spine 31(1):11–17
Muschik M, Ludwig R, Halbhubner S, Bursche K, Stoll T (2001) Beta-tricalcium phosphate as a bone substitute for dorsal spinal fusion in adolescent idiopathic scoliosis: preliminary results of a prospective clinical study. Eur Spine J 10(Suppl 2):S178–S184. doi:10.1007/s005860100271 (Official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society)
Yamada T, Yoshii T, Sotome S, Yuasa M, Kato T, Arai Y, Kawabata S, Tomizawa S, Sakaki K, Hirai T, Shinomiya K, Okawa A (2011) Hybrid grafting using bone marrow aspirate combined with porous beta-tricalcium phosphate and trephine bone for lumbar posterolateral spinal fusion: a prospective comparative study-versus local bone grafting. Spine 37(3):E174–E179. doi:10.1097/BRS.0b013e3182269d64
Sugawara T, Itoh Y, Hirano Y, Higashiyama N, Mizoi K (2011) Beta-tricalcium phosphate promotes bony fusion after anterior cervical discectomy and fusion using titanium cages. Spine 36(23):E1509–E1514. doi:10.1097/BRS.0b013e31820e60d9
Hackenberg L, Halm H, Bullmann V, Vieth V, Schneider M, Liljenqvist U (2005) Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to five year results. Eur Spine J 14(6):551–558. doi:10.1007/s00586-004-0830-1 (Official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society)
Faundez AA, Schwender JD, Safriel Y, Gilbert TJ, Mehbod AA, Denis F, Transfeldt EE, Wroblewski JM (2009) Clinical and radiological outcome of anterior-posterior fusion versus transforaminal lumbar interbody fusion for symptomatic disc degeneration: a retrospective comparative study of 133 patients. Eur Spine J 18(2):203–211. doi:10.1007/s00586-008-0845-0 (Official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society)
Christensen FB, Laursen M, Gelineck J, Eiskjaer SP, Thomsen K, Bunger CE (2001) Interobserver and intraobserver agreement of radiograph interpretation with and without pedicle screw implants: the need for a detailed classification system in posterolateral spinal fusion. Spine 26(5):538–543 (discussion 543–534)
Stauffer RN, Coventry MB (1972) Posterolateral lumbar-spine fusion. Analysis of Mayo Clinic series. J Bone Joint Surg Am 54(6):1195–1204
Zhou ZJ, Zhao FD, Fang XQ, Zhao X, Fan SW (2011) Meta-analysis of instrumented posterior interbody fusion versus instrumented posterolateral fusion in the lumbar spine. J Neurosurg Spine 15(3):295–310. doi:10.3171/2011.4.SPINE10330
Cloward RB (1953) The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. I. Indications, operative technique, after care. J Neurosurg 10(2):154–168. doi:10.3171/jns.1953.10.2.0154
Goh JC, Wong HK, Thambyah A, Yu CS (2000) Influence of PLIF cage size on lumbar spine stability. Spine 25(1):35–39 (discussion 40)
Epstein NE (2006) A preliminary study of the efficacy of beta tricalcium phosphate as a bone expander for instrumented posterolateral lumbar fusions. J Spinal Disord Tech 19(6):424–429
Kroner AH, Eyb R, Lange A, Lomoschitz K, Mahdi T, Engel A (2006) Magnetic resonance imaging evaluation of posterior lumbar interbody fusion. Spine 31(12):1365–1371. doi:10.1097/01.brs.0000218583.43398.e3
Chen WJ, Tsai TT, Chen LH, Niu CC, Lai PL, Fu TS, McCarthy K (2005) The fusion rate of calcium sulfate with local autograft bone compared with autologous iliac bone graft for instrumented short-segment spinal fusion. Spine 30(20):2293–2297
Hashimoto T, Shigenobu K, Kanayama M, Harada M, Oha F, Ohkoshi Y, Tada H, Yamamoto K, Yamane S (2002) Clinical results of single-level posterior lumbar interbody fusion using the Brantigan I/F carbon cage filled with a mixture of local morselized bone and bioactive ceramic granules. Spine 27(3):258–262
Kai Y, Oyama M, Morooka M (2004) Posterior lumbar interbody fusion using local facet joint autograft and pedicle screw fixation. Spine 29(1):41–46. doi:10.1097/01.BRS.0000103940.57588.50
Miura Y, Imagama S, Yoda M, Mitsuguchi H, Kachi H (2003) Is local bone viable as a source of bone graft in posterior lumbar interbody fusion? Spine 28(20):2386–2389. doi:10.1097/01.BRS.0000085326.73430.68
Ito Z, Matsuyama Y, Sakai Y, Imagama S, Wakao N, Ando K, Hirano K, Tauchi R, Muramoto A, Matsui H, Matsumoto T, Kanemura T, Yoshida G, Ishikawa Y, Ishiguro N (2010) Bone union rate with autologous iliac bone versus local bone graft in posterior lumbar interbody fusion. Spine 35(21):E1101–E1105. doi:10.1097/BRS.0b013e3181de4f2e
Nakashima H, Yukawa Y, Ito K, Horie Y, Machino M, Kanbara S, Morita D, Imagama S, Ishiguro N, Kato F (2011) Extension CT scan: its suitability for assessing fusion after posterior lumbar interbody fusion. Eur Spine J 20(9):1496–1502. doi:10.1007/s00586-011-1739-0 (Official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society)
McAfee PC, Boden SD, Brantigan JW, Fraser RD, Kuslich SD, Oxland TR, Panjabi MM, Ray CD, Zdeblick TA (2001) Symposium: a critical discrepancy-a criteria of successful arthrodesis following interbody spinal fusions. Spine 26(3):320–334
Carreon LY, Glassman SD, Schwender JD, Subach BR, Gornet MF, Ohno S (2008) Reliability and accuracy of fine-cut computed tomography scans to determine the status of anterior interbody fusions with metallic cages. Spine J 8(6):998–1002. doi:10.1016/j.spinee.2007.12.004 (Official journal of the North American Spine Society)
Carreon LY, Djurasovic M, Glassman SD, Sailer P (2007) Diagnostic accuracy and reliability of fine-cut CT scans with reconstructions to determine the status of an instrumented posterolateral fusion with surgical exploration as reference standard. Spine 32(8):892–895. doi:10.1097/01.brs.0000259808.47104.dd
Lee JH, Park JW, Lee HS (2011) Fusion rates of a morselized local bone graft in polyetheretherketone cages in posterior lumbar interbody fusion by quantitative analysis using consecutive three-dimensional computed tomography scans. Spine J. doi:10.1016/j.spinee.2011.04.029 (Official journal of the North American Spine Society)
Santos ER, Goss DG, Morcom RK, Fraser RD (2003) Radiologic assessment of interbody fusion using carbon fiber cages. Spine 28(10):997–1001. doi:10.1097/01.BRS.0000061988.93175.74
Lee JH, Jeon DW, Lee SJ, Chang BS, Lee CK (2010) Fusion rates and subsidence of morselized local bone grafted in titanium cages in posterior lumbar interbody fusion using quantitative three-dimensional computed tomography scans. Spine 35(15):1460–1465. doi:10.1097/BRS.0b013e3181c4baf5
Park Y, Ha JW, Lee YT, Sung NY (2011) The effect of a radiographic solid fusion on clinical outcomes after minimally invasive transforaminal lumbar interbody fusion. Spine J 11(3):205–212. doi:10.1016/j.spinee.2011.01.023 (Official journal of the North American Spine Society)
Tsutsumimoto T, Shimogata M, Yoshimura Y, Misawa H (2008) Union versus nonunion after posterolateral lumbar fusion: a comparison of long-term surgical outcomes in patients with degenerative lumbar spondylolisthesis. Eur Spine J 17(8):1107–1112. doi:10.1007/s00586-008-0695-9 (Official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society)
Andersen T, Christensen FB, Laursen M, Hoy K, Hansen ES, Bunger C (2001) Smoking as a predictor of negative outcome in lumbar spinal fusion. Spine 26(23):2623–2628
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. Thaler and R. Lechner contributed equally to this work.
Rights and permissions
About this article
Cite this article
Thaler, M., Lechner, R., Gstöttner, M. et al. The use of beta-tricalcium phosphate and bone marrow aspirate as a bone graft substitute in posterior lumbar interbody fusion. Eur Spine J 22, 1173–1182 (2013). https://doi.org/10.1007/s00586-012-2541-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2541-3