Abstract
Introduction
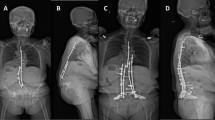
The conventional open pedicle screw fusion (PSF) requires an extensive detachment of the paraspinal muscle from the posterior aspect of the lumbar spine, which can cause muscle injury and subsequently lead to “approach-related morbidity”. The spinous process-splitting (SPS) approach for decompression, unilateral laminotomy for bilateral decompression, and the Wiltse approach for pedicle screw insertion are considered to be less invasive to the paraspinal musculature. We investigated whether SPS open PSF combined with the abovementioned techniques attenuates the paraspinal muscle damage and yields favorable clinical results, including alleviation in the low back discomfort, in comparison to the conventional open PSF.
Methods
We studied 53 patients who underwent single-level PSF for the treatment of degenerative spondylolisthesis (27 patients underwent SPS open PSF and the other 26 underwent the conventional open PSF). The clinical outcomes were assessed using the Japanese Orthopedic Association (JOA) score, the Roland–Morris disability questionnaire (RDQ), and the visual analog scale (VAS) for low back pain and low back discomfort (heavy feeling or stiffness). Postoperative multifidus (MF) atrophy was evaluated using MRI. Follow-up examinations were performed at 1 and 3 years after the surgery.
Results
Although there was no significant difference in the JOA and RDQ score between the two groups, the VAS score for low back pain and discomfort after the surgery were significantly lower in the SPS open PSF group than in the conventional open PSF group. The extent of MF atrophy after SPS open PSF was reduced more significantly than after the conventional open PSF during the follow-up. The MF atrophy ratio was found to correlate with low back discomfort at the 1-year follow-up examination.
Conclusion
In conclusion, SPS open PSF was less damaging to the paraspinal muscle than the conventional open PSF and had a significant clinical effect, reducing low back discomfort over 1 year after the surgery.





Similar content being viewed by others
References
Sihvonen T, Herno A, Paljarvi L, Airaksinen O, Partanen J, Tapaninaho A (1993) Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine 18:575–581
Taylor H, McGregor AH, Medhi-Zadeh S, Richards S, Kahn N, Zadeh JA et al (2002) The impact of self-retaining retractors on the paraspinal muscles during posterior spinal surgery. Spine 27:2758–2762
Khoo LT, Palmer S, Laich DT, Laich DT, Fessler RG (2002) Minimally invasive percutaneous posterior lumbar interbody fusion. Neurosurgery 51(suppl 2):166–181
Logroscino CA, Proietti L, Pola E, Scaramuzzo L, Tamburrelli FC (2011) A Minimally invasive posterior lumbar interbody fusion for degenerative lumbar spine instabilities. Eur Spine J 20(suppl 1):S41–S45
Kantelhardt SR, Martinez R, Baerwinkel S, Burger R, Giese A, Rohde V (2011) Perioperative course and accuracy of screw positioning in conventional, open robotic-guided and percutaneous robotic-guided, pedicles screw placement. Eur Spine J 20:860–868
Park T, Ha JW (2007) Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine 32:537–543
Watanabe K, Hosoya T, Shiraishi T, Matsumoto M, Chiba K, Toyama Y (2005) Lumbar spinous process-splitting laminectomy for lumbar canal stenosis. J Nuerosurg Spine 3:405–408
Oertel MF, Ryang YM, Korinth MC, Gilsbach JM, Rohde V (2006) Long-term results of microsurgical treatment of lumbar spinal stenosis by unilateral laminotomy for bilateral decompression. Neurosurgery 59:1264–1270
Wiltse LL, Bateman JG, Hutchinson RH, Nelson WE (1968) The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Jt Surg Am 50:919–926
Tsutsumimoto T, Shimogata M, Ohta H, Misawa H (2009) Mini-open versus conventional open posterior lumbar interbody fusion for the treatment of lumbar degenerative spondylolisthesis. Spine 34:1923–1928
Kawaguchi Y, Matsui H, Tsuji H (1994) Back muscle injury after posterior lumbar spine surgery: 2. Histologic and histochemical analyses in humans. Spine 19:2598–2602
Shunwu F, Xing Z, Fengdong Z, Xianggian F (2010) Minimally invasive transforaminal lumbar interbody fusion for the treatment of degenerative lumbar diseases. Spine 35:1615–1620
Kim DY, Lee SH, Chung SK, Lee HY (2005) Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine 30:123–129
Shunwu F, Zhijun H, Zhao F, Zhao X, Huang Y, Fang X (2010) Multifidus muscle changes and clinical effects of one-level posterior lumbar interbody fusion: minimally invasive procedure versus conventional open approach. Eur Spine J 19:316–324
Ratanen J, Hurme M, Falck B, Alaranta H, Nykvist F, Lehto M et al (1993) The lumbar multifidus muscle five years after surgery for a lumbar intervertebral disc herniation. Spine 18:568–574
Gejo R, Matsui H, Kawaguchi Y, Ishihara H, Tsuji H (1999) Spinal changes in trunk muscle performance after posterior lumbar surgery. Spine 24:1023–1028
Danneels LA, Vanderstraeten GG, Cambier DC, Witvrouw EE, De Cuyper HJ (2000) CT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. Eur Spine J 9:266–272
Dedering A, Nemeth G, Harms RK (1999) Correlation between electromyographic spectral changes and subjective assessment of lumbar muscle fatigue in subjects without pain from the lower back. Clin Biomech (Bristol, Avon) 14:103–111
Dedering A, Oddsson L, Harms-Ringdahi K, Nemeth G (2002) Electromyography and ratings of lumbar muscle fatigue using a four-level staircase protocol. Clin Biomech (Bristol, Avon) 17:171–176
Demoulin C, Crielaard JM, Vanderthommen M (2007) Spinal muscle evaluation in healthy individuals and low-back-pain patients: a literature review. Jt Bone Spine 74:9–13
Rissanen A, Kalimo H, Alaranta H (1995) Effect of intensive training on the isokinetic strength and structure of lumbar muscles in patients with chronic low back pain. Spine 20:333–340
Storheim K, Holm I, Gunderson R, Brox JI, Bø K (2003) The effect of comprehensive group training on cross-sectional area, density, and strength of paraspinal muscles in patients sick-listed for subacute low back pain. J Spinal Disord Tech 16:271–279
Kikuchi Y, Nakamura T, Takayama S, Horiuchi Y, Toyama Y (2003) MR imaging in the diagnosis of denervated and reinnervated skeletalmuscles: experimental study in rats. Radiology 229:861–867
Bogduk N, Wilson AS, Tynan W (1982) The human lumbar dorsal rami. J Anat 134:383–397
Kawaguchi Y, Matsui H, Tsuji H (1996) Back muscle injury after posterior lumbar spine surgery: a histologic and enzymatic analyses. Spine 21:941–944
Conflict of interest
No grant or any other funding has been received.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mori, E., Okada, S., Ueta, T. et al. Spinous process-splitting open pedicle screw fusion provides favorable results in patients with low back discomfort and pain compared to conventional open pedicle screw fixation over 1 year after surgery. Eur Spine J 21, 745–753 (2012). https://doi.org/10.1007/s00586-011-2146-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-011-2146-2