Abstract
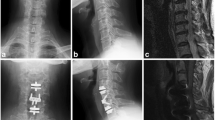
From January 1, 2001 to December 31, 2003, in the Neurosurgery Department of Rome University o “Sapienza,” 167 patients underwent anterior surgery for cervical spondylodiscoarthrosis. The levels treated by the anterior stand-alone technique were: C3–C4 (11%), C4–C5 (19%), C5–C6 (40%), and C6–C7 (30%). All patients underwent left anterior presternocleidomastoid–precarotid approach, microdiscectomy, and interbody fusion using a carbon fiber cage filled with hydroxyapatite. All patients were discharged within 48 h after surgery with cervical orthosis. In one case, a hematoma of the surgical site occurred within 12 h of surgery; for this reason the patient underwent surgical revision and was discharged 4 days later. All patients have worn cervical orthosis for a mean period of 7 weeks and underwent radiological follow-up with cervical RX at 1 and 3 months after surgery. All patients underwent follow-up from 54 to 90 months after surgery, and all of them underwent cervical RX, cervical CT scans for the estimate of fusion, and evaluation of neurological status using VAS and NDI. Of 167 patients, 132 were cooperative for this study, 18 were non-cooperative, and 17 died. The estimation of fusion made by cervical CT scans with sagittal reconstruction showed complete osteointegration of the cage in 115 patients (87.1%), while it showed pseudoarthrosis in 17 patients (12.9%). In 24 patients, we observed adjacent segment degeneration, and 13 of these underwent new surgical procedures in this institute or in another hospital. Clinical evaluation with VAS and NDI showed a good outcome, with poorest benefit in patients over 60 years. The clinical analysis showed a good fusion rate in according with literature, 13% of non-fusion rate without clinical evidence and 20% of ASDegeneration but only 10% had required new surgery. We also observed that patients over 60 years of age had less satisfactory outcome, probably related with the evolution of pathophysiological degeneration of the cervical spine. In the opinion, pseudoarthrosis is caused by malpositioning of the carbon fiber cage.





Similar content being viewed by others
References
Bailey RW, Badgeley MD (1960) Stabilization of the cervical spine by anterior fusion. J Bone Joint Surg (Am) 42-A(4):565–594
Robinson RA, Smith GW (1995) Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp 96:223–224
Cloward RB (1958) The anterior approach for removal of ruptured cervical discs. J Neurosurg 15:602–617
Brantingan J, Steffee A, Geiger J (1991) A carbon fiber implant to aid interbody fusion. Mechanical testing. Spine 16(S6):277–282
Brantingan J (1992) The use of carbon fiber implant in reconstructing anterior spinal column defects. Orthop Trans 16:139–140
Huskisson EC (1974) Measurement of pain. Lancet 2(7889):1127–1131
Vernon H, Mior S (1991) The Neck disability index: a study of reliability and validity. J Manip Physiol Ther 14(7):409–415
Sawin PD, Traynelis VC, Menezes AH (1998) A comparative analysis of fusion rates and donor-site morbidity of autogenic rib and iliac crest bone grafts in posterior cervical fusions. J Neurosurg 88:255–265
Younger EM, Chapman MW (1989) Morbidity at bone graft sites. J Orthop Trauma 3:192–195
Tancredi A, Agrillo A, Delfini R, Fiume D, Frati A, Rinaldi A (2004) Use of carbon fiber cages for treatment of cervical myeloradiculopathies. Surg Neurol 61:221–226
Bohler J, Gaudernak T (1980) Anterior plate stabilization for fracture dislocation of the lower cervical spine. J Trauma 20:203–205
Caspar W, Barbier DD, Klara PM (1989) Anterior cervical fusion and Caspar plate stabilization for cervical trauma. Neurosurg 25:491–502
Fraser JF et al (2007) Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. Neurosurg Spine 6:298–303
Baba H, Furusawa N, Imura S et al (1993) Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine 18:2167–2173
Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg (Am) 84:519–528
Sagawara T, Itoh Y, Hirano Y, Mizoi K (2009) Long term out come and adjacent disc degeneration after anterior cervical discectomy and fusion with titanium cylindrical cages. Acta Neurochir 151:303–309
McCormick PC (2007) The adjacent segment. J Neurosurg Spine 6:1–4
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marotta, N., Landi, A., Tarantino, R. et al. Five-year outcome of stand-alone fusion using carbon cages in cervical disc arthrosis. Eur Spine J 20 (Suppl 1), 8–12 (2011). https://doi.org/10.1007/s00586-011-1747-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-011-1747-0