Abstract
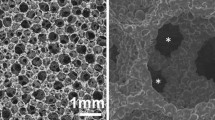
Hydroxyapatite (HA) has been commonly used as a bone graft substitute in various kinds of clinical fields. To improve the healing capability of HA, many studies have been performed to reveal its optimal structural characteristics for better healing outcomes. In spinal reconstruction surgery, non-interconnected porous HAs have already been applied as a bone graft extender in order to avoid autogenous bone harvesting. However, there have been few experimental studies regarding the effects of the structural characteristics of HA in posterolateral lumbar intertransverse process spine fusion (PLF). The aims of this study were to investigate the effect of HA porous characteristics on healing outcomes in a rabbit PLF model in order to elucidate appropriate structural characteristics of HA as a bone graft extender. Thirty-six adult female Japanese White rabbits underwent bilateral intertransverse process fusion at the level of L5–6 without internal fixation. We prepared three types of HA with different porosities: HA with 15% porosity (HA15%), HA with 50% porosity (HA50%), and HA with 85% porosity (HA85%), all of which were clinically available materials. The HA15% and HA50% had few interconnecting pores, whereas the HA85%, which was a recently developed material, had abundant interconnecting pores. All rabbits were randomly divided into the following four groups according to the grafted materials: (1) HA15% + autogenous bone, (2) HA50% + autogenous bone, (3) HA85% + autogenous bone, (4) pure autogenous bone graft. The animals were euthanized at 5 weeks after surgery, and post-mortem analyses including biomechanical testing, radiographical and histological evaluations were performed. There was no statistically significant difference in either fusion rate and/or bending stiffness among the three HA groups. However, in histological and radiological analyses, both bone ingrowth rate and direct bone bonding rate in the HA85% group were significantly higher than those in the HA15% and HA50% groups, despite the similar value of bone volume rate in fusion mass among the three HA groups. In the HA85% group, bone ingrowth was achieved throughout the implanted HAs via interconnecting pores and there was excellent unification between the HA granules and the newly mineralized bone. On the other hand, in the non-interconnected porous HA groups, only a little bone ingrowth could be seen at the peripheral pores of the implanted HA, and its surface was mostly covered with fibrous tissue or empty space. The current study demonstrated that the HA porous characteristics had an effect on the histological outcomes in a rabbit PLF model. We would like to conclude that the interconnected high porous structure seems to be promising for the environment of PLF in the point of producing fusion mass with higher cellular viability. This is because the HA85% is superior in terms of integration with the newly formed bone in fusion mass compared to the non-interconnected porous HAs. However, the porous modifications of HA have little influence on fusion rate and mechanical strength because primary stabilization of the fusion segment is mainly achieved by bridging bone between the adjacent transverse processes outside the implanted materials, rather than the degree of integration between the newly formed bone and the HA granules in PLF.





Similar content being viewed by others
References
Akazawa T, Murata M, Sasaki T (2006) Biodegradation and bioabsorption innovation of the functionally graded bovine bone-originated apatite with blood permeability. J Biomed Mater Res A 76(1):44–51
Annaz B, Hing KA, Kayser M (2004) Porosity variation in Hydroxyapatite and Osteoblast morphology: a scanning electron microscopy study. J Microsc 215(Pt 1):100–110
Berven S, Tay BK, Kleinstueck FS (2001) Clinical applications of bone graft substitutes in spine surgery: consideration of mineralized and demineralized preparations and growth factor supplementation. Eur Spine J 10(Suppl 2):S169–S177
Boden SD (2002) Overview of the biology of Lumbar spine fusion and principles for selecting a bone graft substitute. Spine 27(16 Suppl 1):S26–S31
Boden SD, Martin GJ Jr, Morone M (1999) The use of Coralline Hydroxyapatite with bone marrow, autogenous bone graft, or osteoinductive bone protein extract for posterolateral Lumbar spine fusion. Spine 24(4):320–327
Boden SD, Schimandle JH, Hutton WC (1995) 1995 Volvo Award in basic sciences. The use of an osteoinductive growth factor for lumbar spinal fusion. Part Ii: Study of dose, carrier, and species. Spine 20(24):2633–2644
Boden SD, Schimandle JH, Hutton WC (1995) An experimental lumbar intertransverse process spinal fusion model. Radiographic, histologic, and biomechanical healing characteristics. Spine 20(4):412–420
Chang BS, Lee CK, Hong KS (2000) Osteoconduction at porous hydroxyapatite with various pore configurations. Biomaterials 21(12):1291–1298
Flautre B, Descamps M, Delecourt C (2001) Porous ha ceramic for bone replacement: role of the pores and interconnections—experimental study in the rabbit. J Mater Sci Mater Med 12(8):679–682
Fujishiro T, Nishikawa T, Niikura T (2005) Impaction bone grafting with hydroxyapatite: increased femoral component stability in experiments using sawbones. Acta Orthop 76(4):550–554
Glazer PA, Heilmann MR, Lotz JC (1997) Use of electromagnetic fields in a spinal fusion. A rabbit model. Spine 22(20):2351–2356
Habibovic P, Yuan H, van der Valk CM (2005) 3D Microenvironment as essential element for osteoinduction by biomaterials. Biomaterials 26(17):3565–3575
Hing KA (2004) Bone repair in the twenty-first century: biology, chemistry or engineering? Philos Transact A Math Phys Eng Sci 362(1825):2821–2850
Hing KA, Annaz B, Saeed S (2005) Microporosity enhances bioactivity of synthetic bone graft substitutes. J Mater Sci Mater Med 16(5):467–475
Hing KA, Best SM, Tanner KE (2004) Mediation of bone ingrowth in porous hydroxyapatite bone graft substitutes. J Biomed Mater Res A 68(1):187–200
Ito M, Kotani Y, Hojo N, (2007) Effects of porosity changes in hydroxyapatite ceramics vertebral spacer on its binding capability to the vertebral body: an experimental sheep study. J Neurosurg 6(5):431–437
Kanayama M, Cunningham BW, Weis JC (1997) Maturation of the posterolateral spinal fusion and its effect on load-sharing of spinal instrumentation. An in vivo sheep model. J Bone Joint Surg Am 79(11):1710–1720
Liu DM (1996) Fabrication and characterization of porous hydroxyapatite granules. Biomaterials 17(20):1955–1957
Lu JX, Flautre B, Anselme K (1999) Role of interconnections in porous bioceramics on bone recolonization in vitro and in vivo. J Mater Sci Mater Med 10(2):111–120
Luchetti R (2004) Corrective osteotomy of malunited distal radius fractures using carbonated hydroxyapatite as an alternative to autogenous bone grafting. J Hand Surg 29(5):825–834
Matsumine A, Myoui A, Kusuzaki K (2004) Calcium hydroxyapatite ceramic implants in bone tumour surgery. A long-term follow-up study. J Bone Joint Surg Br 86(5):719–725
Moritz N, Rossi S, Vedel E (2004) Implants coated with bioactive glass by Co2-Laser, an in vivo study. J Mater Sci Mater Med 15(7):795–802
Orr TE, Villars PA, Mitchell SL (2001) Compressive properties of cancellous bone defects in a rabbit model treated with particles of natural bone mineral and synthetic hydroxyapatite. Biomaterials 22(14):1953–1959
Rosa AL, Beloti MM, Oliveira PT (2002) Osseointegration and osseoconductivity of hydroxyapatite of different microporosities. J Mater Sci Mater Med 13(11):1071–1075
Rouahi M, Gallet O, Champion E (2006) Influence of hydroxyapatite microstructure on human bone cell response. J Biomed Mater Res A
Sakamoto M, Matrumoto T, Nakasu M (2007) Development of super porous hydroxyapatites and their utilization for culture of primary rat osteoblast. J Biomed Mater Res A 82(1):238–242
Spivak JM, Hasharoni A (2001) Use of hydroxyapatite in spine surgery. Eur Spine J 10(Suppl 2):S197–S204
Summers BN, Eisenstein SM (1989) Donor site pain from the ilium. A complication of lumbar spine fusion. J Bone Joint Surg Br 71(4):677–680
Tamai N, Myoui A, Tomita T (2002) Novel hydroxyapatite ceramics with an interconnective porous structure exhibit superior osteoconduction in vivo. J Biomed Mater Res 59(1):110–117
Totoribe K, Tajima N, Chosa E (2002) Hydroxyapatite block for use in posterolateral lumbar fusion: a report of four cases. Clin Orthop Relat Res 399:146–151
Wiltse LL, Bateman JG, Hutchinson RH (1968) The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg Am 50(5):919–926
Ylinen P, Raekallio M, Taurio R (2005) Coralline hydroxyapatite reinforced with polylactide fibres in lumbar interbody implantation. J Mater Sci Mater Med 16(4):325–331
Younger EM, Chapman MW (1989) Morbidity at bone graft donor sites. J Orthop Trauma 3(3):192–195
Yuan H, Kurashina K, de Bruijn JD (1999) A preliminary study on osteoinduction of two kinds of calcium phosphate ceramics. Biomaterials 20(19):1799–1806
Acknowledgments
The authors would like to acknowledge Michiko Sakamoto, B.S., PENTAX Co., for their technical support and for providing materials. They are also grateful to Mr. Justin Collings for correcting their use of language. This study was supported by PENTAX Co.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Motomiya, M., Ito, M., Takahata, M. et al. Effect of Hydroxyapatite porous characteristics on healing outcomes in rabbit posterolateral spinal fusion model. Eur Spine J 16, 2215–2224 (2007). https://doi.org/10.1007/s00586-007-0501-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-007-0501-0