Abstract
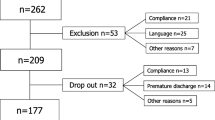
Many of the existing low back pain (LBP) questionnaires of function and symptoms have a content of different domains of disability presented as a single sum score, making it difficult to derive changes within a specific domain. The present study describes the development of a clinically derived back-specific questionnaire incorporating both a functional limitation and a symptom scale, with a further subdivision of the symptom scale in separate indices for severity and temporal aspects. The aims of the study were to assess the overall reliability and validity of the new questionnaire, named the Profile Fitness Mapping questionnaire (PFM). A total of 193 chronic LBP patients answered the PFM together with five validated criterion questionnaires. For the internal consistency of the questionnaires, the three indices of the PFM had the highest Cronbach’s alpha (0.90–0.95) and all items had item–total correlations above 0.2. The correlation coefficients between the PFM and the back-specific criterion questionnaires ranged between 0.61 and 0.83, indicating good concurrent criterion validity. The best discriminative ability between patients with different pain severities was demonstrated by the functional limitation scale of the PFM. Well centered score distribution with no patient’s score at the floor or the ceiling level indicates that the PFM has the potential to detect the improvement or worsening of symptoms and functional limitations in chronic LBP patients. Classification according to the International Classification of Functioning, Disability and health (ICF) of WHO revealed a high degree of homogeneous item content of the symptom scale to the domain of impairments, and of the functional limitation scale to the domain of activity limitations. The present study suggests that the PFM has a high internal consistency and is a valid indicator of symptoms and functional limitations of LBP patients. It offers the combination of a composite total score and the possibility of evaluations within specific domains of disability. Complementary evaluation of test–retest reliability and responsiveness to change is warranted.





Similar content being viewed by others
References
Altman DG (1991) Practical statistics for medical research. Chapman and Hall, London
Andresen EM (2000) Criteria for assessing the tools of disability outcomes research. Arch Phys Med Rehabil 81:S15–S20
Atroshi I, Gummesson C, Andersson B, Dahlgren E, Johansson A (2000) The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: reliability and validity of the Swedish version evaluated in 176 patients. Acta Orthop Scand 71:613–618
Bergner M, Bobbitt RA, Kressel S, Pollard WE, Gilson BS, Morris JR (1976) The sickness impact profile: conceptual formulation and methodology for the development of a health status measure. Int J Health Serv 6:393–415
Brown FG (1983) Principles of educational and psychological testing, 3rd edn. Holt, Rinehart and Winston, New York
Cieza A, Stucki G, Weigl M, Disler P, Jackel W, van der Linden S, Kostanjsek N, de Bie R (2004) ICF core sets for low back pain. J Rehabil Med July:69–74
Cronbach LJ (1951) Coefficient alpha and the internal structure of tests. Psychometrika 16:297–334
Deyo RA, Battie M, Beurskens AJ, Bombardier C, Croft P, Koes B, Malmivaara A, Roland M, Von Korff M, Waddell G (1998) Outcome measures for low back pain research. A proposal for standardized use. Spine 23:2003–2013
Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, Kerns RD, Stucki G, Allen RR, Bellamy N, Carr DB, Chandler J, Cowan P, Dionne R, Galer BS, Hertz S, Jadad AR, Kramer LD, Manning DC, Martin S, McCormick CG, McDermott MP, McGrath P, Quessy S, Rappaport BA, Robbins W, Robinson JP, Rothman M, Royal MA, Simon L, Stauffer JW, Stein W, Tollett J, Wernicke J, Witter J (2005) Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 113:9–19
Ekman M, Jonhagen S, Hunsche E, Jonsson L (2005) Burden of illness of chronic low back pain in Sweden: a cross-sectional, retrospective study in primary care setting. Spine 30:1777–1785
Garratt AM, Klaber Moffett J, Farrin AJ (2001) Responsiveness of generic and specific measures of health outcome in low back pain. Spine 26:71–77
Greenough CG, Fraser RD (1992) Assessment of outcome in patients with low-back pain. Spine 17:36–41
Grotle M, Brox JI, Vollestad NK (2005) Functional status and disability questionnaires: what do they assess? A systematic review of back-specific outcome questionnaires. Spine 30:130–140
Jacob T, Zeev A (2006) Are localized low back pain and generalized back pain similar entities? Results of a longitudinal community based study. Disabil Rehabil 28:369–377
Jensen MP, Karoly P (2001) Self-report scales and procedures for assessing pain in adults. In: Turk DC, Melzack R (eds) Handbook of pain assessment. Guilford Press, New York, pp 15–34
Kjellberg A (1989) Att ställa frågor om arbetsmiljön: en kort handledning i konstruktion av frågeformulär [Swedish]. Arbetsmiljöinstitutet, Förlagstjänst, Solna
Kopec JA, Esdaile JM, Abrahamowicz M, Abenhaim L, Wood-Dauphinee S, Lamping DL, Williams JI (1996) The Quebec back pain disability scale: conceptualization and development. J Clin Epidemiol 49:151–161
Lackner JM, Carosella AM (1999) The relative influence of perceived pain control, anxiety, and functional self efficacy on spinal function among patients with chronic low back pain. Spine 24:2254–2260
Lansky D, Butler JB, Waller FT (1992) Using health status measures in the hospital setting: from acute care to ‘outcomes management’. Med Care 30:MS57–MS73
Margolis RB, Chibnall JT, Tait RC (1988) Test–retest reliability of the pain drawing instrument. Pain 33:49–51
Müller U, Duetz MS, Roeder C, Greenough CG (2004a) Condition-specific outcome measures for low back pain. Part I: validation. Eur Spine J 13:301–313
Müller U, Roeder C, Dubs L, Duetz MS, Greenough CG (2004b) Condition-specific outcome measures for low back pain. Part II: scale construction. Eur Spine J 13:314–324
Müller U, Röder C, Greenough CG (2006) Back related outcome assessment instruments. Eur Spine J 15(Suppl 1):S25–S31
Nunally JC (1967) Psychometric theory. McGraw-Hill, New York
Ohnmeiss DD (2000) Repeatability of pain drawings in a low back pain population. Spine 25:980–988
Rainville J, Ahern DK, Phalen L, Childs LA, Sutherland R (1992) The association of pain with physical activities in chronic low back pain. Spine 17:1060–1064
Rocchi MB, Sisti D, Benedetti P, Valentini M, Bellagamba S, Federici A (2005) Critical comparison of nine different self-administered questionnaires for the evaluation of disability caused by low back pain. Eura Medicophys 41:275–281
Roland M, Fairbank J (2000) The Roland–Morris disability questionnaire and the Oswestry disability questionnaire. Spine 25:3115–3124
Roland M, Morris R (1983) A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine 8:141–144
Ruta DA, Garratt AM, Wardlaw D, Russell IT (1994) Developing a valid and reliable measure of health outcome for patients with low back pain. Spine 19:1887–1896
Stratford PW, Binkley JM, Riddle DL (2000) Development and initial validation of the back pain functional scale. Spine 25:2095–2102
Streiner GL, Norman DR (1990) Health measurement scales: a practical guide to their development and use. Oxford University Press, Oxford
Suarez-Almazor ME, Kendall C, Johnson JA, Skeith K, Vincent D (2000) Use of health status measures in patients with low back pain in clinical settings: comparison of specific, generic and preference-based instruments. Rheumatology (Oxf) 39:783–790
Turk DC (2002) Clinical effectiveness and cost-effectiveness of treatments for patients with chronic pain. Clin J Pain 18:355–365
Waddell G, Main CJ (1984) Assessment of severity in low-back disorders. Spine 9:204–208
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
WHO (2001) International Classification of Functioning, Disability and Health: ICF. Short version. World Health Organization, Geneva
Acknowledgements
The authors would like to direct a special thank to physiologist Henrik Cyrén for most valuable help during the development of the Profile Fitness Mapping scales, Maria Frykman and Nisse Larson for valuable assistance during data collection, processing and analyses, and Margaretha Marklund for graphical work. The present study complies with the Swedish laws and was performed after obtaining advisory pronouncement by the Regional Ethical Review Board in Uppsala, Sweden, and informed consent from each subject.
Author information
Authors and Affiliations
Corresponding author
Appendix: The profile fitness mapping questionnaire
Appendix: The profile fitness mapping questionnaire
The symptom scale

The functional limitation scale

Method of score calculation for the Profile Fitness Mapping scales
The table shows the weighting and maximum score of each item in the Profile Fitness Mapping scales, and the calculation of scores for each index.
Frequency (f) is the answer on how often the symptom is felt (six-point scale from 1 = never/very seldom, to 6 = very often/always). Intensity (i) is the answer on how much the symptom is felt (six-point scale from 7 = nothing/none at all, to 12 = almost unbearable/unbearable, all/maximally). The answers of the functional limitation scale (fl) range from 1 = very good, no problem, very satisfying, very likely, to 6 = very bad, very difficult/impossible, very dissatisfying, very unlikely.
The result of each index is expressed as the percentage of the maximum score, where 100% is the best possible result. Adjustments due to omitted questions are done by removing the maximum score for those questions from the denominator before calculating the percentage.
The symptom scale (s) | The functional limitation scale (fl) | |||||||
|---|---|---|---|---|---|---|---|---|
Items | Weight (W s) | Score frequency index | Score intensity index | Max score | Itemfl | Weight (W fl) | Score function index | Max score |
1 | 2.4 | (6-f1)*W s | (12-i1)* W s | 12 | 1 | 3 | (6-fl1)*W fl | 15 |
2 | 2 | (6-f2)*W s | (12-i2)* W s | 10 | 2 | 3 | (6-fl2)*W fl | 15 |
3 | 1.6 | (6-f3)*W s | (12-i3)* W s | 8 | 3 | 4 | (6-fl3)*W fl | 20 |
4 | 2 | (6-f4)*W s | (12-i4)*W s | 10 | 4 | 3 | (6-fl4)*W fl | 15 |
5 | 1.2 | (6-f5)*W s | (12-i5)*W s | 6 | 5 | 2 | (6-fl5)*W fl | 10 |
6 | 2.4 | (6-f6)*W s | (12-i6)*W s | 12 | 6 | 1.6 | (6-fl6)*W fl | 8 |
7 | 3 | (6-f7)* W s | (12-i7)* W s | 15 | 7 | 1.6 | (6-fl7)*W fl | 8 |
8 | 3 | (6-f8)* W s | (12-i8)* W s | 15 | 8 | 1.2 | (6-fl8)*W fl | 6 |
9 | 4 | (6-f9)* W s | (12-i9)* W s | 20 | 9 | 2 | (6-fl9)*W fl | 10 |
10 | 3 | (6-f10)* W s | (12-i10)* W s | 15 | 10 | 2.4 | (6-fl10)* W fl | 12 |
11 | 5 | (6-f11)* W s | (12-i11)* W s | 25 | 11 | 3 | (6-fl11)* W fl | 15 |
12 | 5 | (6-f12)* W s | (12-i12)* W s | 25 | 12 | 3 | (6-fl12)* W fl | 15 |
13 | 2 | (6-f13)* W s | (12-i13)* W s | 10 | 13 | 3 | (6-fl13)*W fl | 15 |
14 | 3 | (6-f14)* W s | (12-i14)* W s | 15 | 14 | 3 | (6-fl14)* W fl | 15 |
15 | 4 | (6-f15)* W s | (12-i15)* W s | 20 | 15 | 3 | (6-fl15)* W fl | 15 |
16 | 3 | (6-f16)* W s | (12-i16)* W s | 15 | 16 | 3 | (6-fl16)* W fl | 15 |
17 | 2 | (6-f17)* W s | (12-i17)* W s | 10 | 17 | 2 | (6-fl17)* W fl | 10 |
18 | 2 | (6-f18)* W s | (12-i18)* W s | 10 | 18 | 2.4 | (6-fl18)* W fl | 12 |
19 | 2 | (6-f19)* W s | (12-i19)* W s | 10 | 19 | 2 | (6-fl19)* W fl | 10 |
20 | 2.4 | (6-f20)* W s | (12-i20)* W s | 12 | 20 | 1.6 | (6-fl20)* W fl | 8 |
21 | 2 | (6-f21)* W s | (12-i21)* W s | 10 | 21 | 2 | (6-fl21)* W fl | 10 |
22 | 8 | (6-f22)* W s | (12-i22)* W s | 40 | 22 | 2 | (6-fl22)* W fl | 10 |
23 | 8 | (6-f23)* W s | (12-i23)* W s | 40 | 23 | 2 | (6-fl23)* W fl | 10 |
24 | 3.6 | (6-f24)* W s | (12-i24)* W s | 18 | 24 | 2 | (6-fl24)* W fl | 10 |
25 | 3.6 | (6-f25)* W s | (12-i25)* W s | 18 | 25 | 7 | (6-fl25)* W fl | 35 |
26 | 4 | (6-f26)* W s | (12-i26)* W s | 20 | 26 | 4 | (6-fl26)* W fl | 20 |
27 | 2.4 | (6-f27)* W s | (12-i27)* W s | 12 | 27 | 4 | (6-fl27)* W fl | 20 |
28 | 7 | (6-fl28)* W fl | 35 | |||||
Rights and permissions
About this article
Cite this article
Björklund, M., Hamberg, J., Heiden, M. et al. The assessment of symptoms and functional limitations in low back pain patients: validity and reliability of a new questionnaire. Eur Spine J 16, 1799–1811 (2007). https://doi.org/10.1007/s00586-007-0405-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-007-0405-z