Abstract
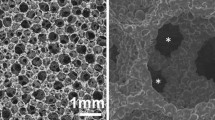
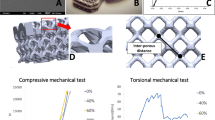
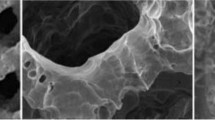
Arthrodesis using interbody cages has demonstrated high fusion rates. However, permanent cages are exposed to stress-shielding, corrosion, and may require explanation when necessary. Polylactic acid (PLA) bioresorbable cages are developed for avoiding these problems, but significant tissue reaction has been reported with 70/30 PLDLLA in some preclinical animal studies. The objective was to evaluate 96/4 PLDLLA cages in a sheep model over 3 years. Sixteen sheeps underwent one level anterior lumbar interbody fusion using 96/4 PLDLLA cages, filled and surrounded with cancellous bone graft from the iliac crest. Six groups of three animals were killed after 3, 6, 9, 12, 24, and 36 months. Harvested lumbar spine had radiographic, MRI, and CT evaluation and histological analysis. Histological results: cage swelling and slight signs of fragmentation associated to fibrocartilaginous tissue apposition at 3 months; bone remodeling around the cage with direct apposition of the mineralization front at 6 months; active cage degradation and complete fusion around the cage at 9 months; cage fragmentation and partial replacement by bone tissue at 12 months; bone bridges in and around the cage at 24 months; full resorption and intervertebral fusion at 36 months. Radiological results: partial arthrodesis at 3 months; definite peripheral arthrodesis at 6 months; similar aspect at 9 months; significant cage resorption at 12 months; definite inner and outer fusion at 24 months; complete cage resorption and calcification at the location of the cage at 36 months confirmed histological observations. Radiographic, CT scan, MRI, and histological data were consistent for showing progressive resorption of 96/4 PLDLLA, interbody fusion, and bone remodeling, with no significant signs of local intolerance reaction. These results are promising and suggest further development of 96/4 PLDLLA cages.









Similar content being viewed by others
References
AFNOR (2005) [Biological evaluation of medical devices - part 6: local effects after implantation]. J Off Repub Fr 70
Agazzi S, Reverdin A, May D (1999) Posterior lumbar interbody fusion with cages: an independent review of 71 cases. J Neurosurg 91:186–192
Alexander JT, Branch CL Jr, Subach BR et al (2002a) Applications of a resorbable interbody spacer in posterior lumbar interbody fusion. J Neurosurg 97:468–472
Alexander JT, Branch CL Jr, Subach BR et al (2002b) Applications of a resorbable interbody spacer via a posterior lumbar interbody fusion technique. Orthopedics 25:s1185–s1189
An YH, Woolf SK, Friedman RJ (2000) Pre-clinical in vivo evaluation of orthopaedic bioabsorbable devices. Biomaterials 21:2635–2652
Bergsma JE, de Bruijn WC, Rozema FR et al (1995a) Late degradation tissue response to poly(l-lactide) bone plates and screws. Biomaterials 16:25–31
Bergsma JE, Rozema FR, Bos RR et al (1995b) In vivo degradation and biocompatibility study of in vitro pre-degraded as-polymerized polyactide particles. Biomaterials 16:267–274
Bostman O, Pihlajamaki H (2000) Clinical biocompatibility of biodegradable orthopaedic implants for internal fixation: a review. Biomaterials 21:2615–2621
Brantigan JW, Steffee AD (1993) A carbon fiber implant to aid interbody lumbar fusion. Two-year clinical results in the first 26 patients. Spine 18:2106–2107
Casteleyn PP, Handelberg F, Haentjens P (1992) Biodegradable rods versus Kirschner wire fixation of wrist fractures. A randomised trial. J Bone Joint Surg Br 74:858–861
Chen C, Chueh J, Tseng H et al (2003) Preparation and characterization of biodegradable PLA polymeric blends. Biomaterials 24:1167–1173
Ciccone WJ 2nd, Motz C, Bentley C et al (2001) Bioabsorbable implants in orthopaedics: new developments and clinical applications. J Am Acad Orthop Surg 9:280–288
de Medinaceli L, al Khoury R, Merle M (1995) Large amounts of polylactic acid in contact with divided nerve sheaths have no adverse effects on regeneration. J Reconstr Microsurg 11:43–49
Donath K, Breuner G (1982) A method for the study of undecalcified bones and teeth with attached soft tissues. The Sage–Schliff (sawing and grinding) technique. J Oral Pathol 11:318–326
Eindorf T, Pflugmacher R, Koch C et al (2005) Spinal fusion with bioresorbable cages—severe degradation effects. Eur Spine J 14:S20
Gogolewski S (2000) Bioresorbable polymers in trauma and bone surgery. Injury 31(Suppl 4):28–32
Hoffmann R, Krettek C, Hetkamper A et al (1992) [Osteosynthesis of distal radius fractures with biodegradable fracture rods. Results of two years follow-up]. Unfallchirurg 95:99–105
Hollinger JO, Battistone GC (1986) Biodegradable bone repair materials. Synthetic polymers and ceramics. Clin Orthop 290–305
Kanayama M, Cunningham BW, Haggerty CJ et al (2000) In vitro biomechanical investigation of the stability and stress-shielding effect of lumbar interbody fusion devices. J Neurosurg 93:259–265
Kandziora F, Pflugmacher R, Scholz M et al (2004) Bioabsorbable interbody cages in a sheep cervical spine fusion model. Spine 29:1845–1855
Kuslich SD, Danielson G, Dowdle JD et al (2000) Four-year follow-up results of lumbar spine arthrodesis using the Bagby and Kuslich lumbar fusion cage. Spine 25:2656–2662
Lundgren D, Nyman S, Mathisen T et al (1992) Guided bone regeneration of cranial defects, using biodegradable barriers: an experimental pilot study in the rabbit. J Craniomaxillofac Surg 20:257–260
Mainil-Varlet P, Rahn B, Gogolewski S (1997) Long-term in vivo degradation and bone reaction to various polylactides. 1. One-year results. Biomaterials 18:257–266
McAfee PC (1999a) Interbody fusion cages in reconstructive operations on the spine. J Bone Joint Surg Am 81:859–880
McAfee PC, Cunningham BW, Lee GA et al (1999b) Revision strategies for salvaging or improving failed cylindrical cages. Spine 24:2147–2153
Merloz P, Minfelde R, Schelp C et al (1995) [In vitro study of the properties of bioresorbable lactic acid polymer materials]. Rev Chir Orthop Reparatrice Appar Mot 81:433–444
Onesti ST, Ashkenazi E (1998) The Ray threaded fusion cage for posterior lumbar interbody fusion. Neurosurgery 42:200–204
Pihlajamaki H, Kinnunen J, Bostman O (1997) In vivo monitoring of the degradation process of bioresorbable polymeric implants using magnetic resonance imaging. Biomaterials 18:1311–1315
Pistner H, Gutwald R, Ordung R et al (1993) Poly(l-lactide): a long-term degradation study in vivo. I. Biological results. Biomaterials 14:671–677
Ray CD (1997) Threaded titanium cages for lumbar interbody fusions. Spine 22:667–679
Regan JJ, Yuan H, McAfee PC (1999) Laparoscopic fusion of the lumbar spine: minimally invasive spine surgery. A prospective multicenter study evaluating open and laparoscopic lumbar fusion. Spine 24:402–411
Rish BL (1989) A critique of posterior lumbar interbody fusion: 12 years’ experience with 250 patients. Surg Neurol 31:281–289
Rokkanen PU, Bostman O, Hirvensalo E et al (2000) Bioabsorbable fixation in orthopaedic surgery and traumatology. Biomaterials 21:2607–2613
Schwach G, Coudane J, Engel R et al (2002) Influence of polymerization conditions on the hydrolytic degradation of poly(dl-lactide) polymerized in the presence of stannous octoate or zinc-metal. Biomaterials 23:993–1002
Schwach G, Vert M (1999) In vitro and in vivo degradation of lactic acid-based interference screws used in cruciate ligament reconstruction. Int J Biol Macromol 25:283–291
Shah RR, Mohammed S, Saifuddin A et al (2003) Comparison of plain radiographs with CT scan to evaluate interbody fusion following the use of titanium interbody cages and transpedicular instrumentation. Eur Spine J 12:378–385
Smit TH, Muller R, Van Dijk M et al (2003) Changes in bone architecture during spinal fusion: three years follow-up and the role of cage stiffness. Spine 28:1802–1808
Togawa D, Bauer TW, Brantigan JW et al (2001) Bone graft incorporation in radiographically successful human intervertebral body fusion cages. Spine 26:2744–2750
Toth JM, Estes BT, Wang M et al (2002a) Evaluation of 70/30 poly (l-lactide-co-dl-lactide) for use as a resorbable interbody fusion cage. J Neurosurg 97:423–432
Toth JM, Wang M, Scifert JL et al (2002b) Evaluation of 70/30 D,L-PLa for use as a resorbable interbody fusion cage. Orthopedics 25:s1131–s1140
Tullberg T (1998) Failure of a carbon fiber implant. A case report. Spine 23:1804–1806
Tunc DC (1996) In vivo degradation and biocompatability study of in vitro pre-degraded as-polymerized polylactide particles. Biomaterials 17:2109–2112
van Dijk M, Smit TH, Burger EH et al (2002a) Bioabsorbable poly-l-lactic acid cages for lumbar interbody fusion: three-year follow-up radiographic, histologic, and histomorphometric analysis in goats. Spine 27:2706–2714
van Dijk M, Smit TH, Sugihara S et al (2002b) The effect of cage stiffness on the rate of lumbar interbody fusion: an in vivo model using poly(l-lactic Acid) and titanium cages. Spine 27:682–688
van Dijk M, Tunc DC, Smit TH et al (2002c) In vitro and in vivo degradation of bioabsorbable PLLA spinal fusion cages. J Biomed Mater Res 63:752–759
van Dijk M, van Diest PJ, Smit TH et al (2005) Four-year follow-up of poly-l-lactic acid cages for lumbar interbody fusion in goats. J Long Term Eff Med Implants 15:125–138
Viljanen J, Kinnunen J, Bondestam S et al (1995) Bone changes after experimental osteotomies fixed with absorbable self-reinforced poly-l-lactide screws or metallic screws studied by plain radiographs, quantitative computed tomography and magnetic resonance imaging. Biomaterials 16:1353–1358
Warden WH, Friedman R, Teresi LM et al (1999) Magnetic resonance imaging of bioabsorbale polylactic acid interference screws during the first 2 years after anterior cruciate ligament reconstruction. Arthroscopy 15:474–480
Weiler A, Helling HJ, Kirch U et al (1996) Foreign-body reaction and the course of osteolysis after polyglycolide implants for fracture fixation: experimental study in sheep. J Bone Joint Surg Br 78:369–376
Weiler A, Hoffmann RF, Stahelin AC et al (2000) Biodegradable implants in sports medicine: the biological base. Arthroscopy 16:305–321
Weiner BK, Fraser RD (1998) Spine update lumbar interbody cages. Spine 23:634–640
Wilke HJ, Kettler A, Claes LE (1997) Are sheep spines a valid biomechanical model for human spines? Spine 22:2365–2374
Wuisman PI, van Dijk M, Smit TH (2002) Resorbable cages for spinal fusion: an experimental goat model. J Neurosurg 97:433–439
Zdeblick TA, Phillips FM (2003) Interbody cage devices. Spine 28:S2–S7
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lazennec, J.Y., Madi, A., Rousseau, M.A. et al. Evaluation of the 96/4 PLDLLA polymer resorbable lumbar interbody cage in a long term animal model. Eur Spine J 15, 1545–1553 (2006). https://doi.org/10.1007/s00586-006-0145-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-006-0145-5