Abstract
Traditionally, spinal fusion has been denied to patients with scoliosis secondary to Duchenne's muscular dystrophy (DMD) when their forced vital capacity (FVC) is less than 30–40% of predicted values (PFVC). The reasons for this decision are a theoretically increased risk of adverse events from a prolonged anaesthetic and extensive surgery. This paper presents a retrospective analysis of 30 patients with DMD scoliosis who underwent posterior spinal fusion at the Royal National Orthopaedic Hospital. Two subgroups of patients were compared: those with more than 30% PFVC (17 patients) and those with less than 30% PVFC (13 patients). One patient in each group required a temporary tracheotomy and there were nine complications in total. The post-operative stay for patients in each group was similar (24 days in the >30% group, 20 days in the <30% group) and the complication rate was comparable with other published series. We conclude that spinal fusion can be offered to patients with DMD even in the presence of a low FVC.
Similar content being viewed by others
Introduction
Duchenne's muscular dystrophy (DMD) is an X-linked recessive disease that typically causes death from respiratory failure in late adolescence or early adulthood. It is the most common of the dystrophies (1 in 5000 live male births) and is characterised by a progressive muscle wasting and weakness leading to a loss of ambulation by the early teens. Muscle weakness is due to lack of the protein dystrophin in skeletal muscle cell membranes, and this can be tested for by immunohistochemical techniques or by western blotting electrophoresis on a muscle biopsy specimen [3, 7, 9, 10, 13, 15, 16, 17].
Most patients with DMD develop a progressive scoliosis starting at the time of loss of ambulatory status [1, 3, 5, 7, 9, 12, 13, 15, 18, 19, 20, 22, 23]. This occurs in 50–95% of patients, and is associated with a deteriorating vital capacity (4% for every 10° Cobb angle). Independent of the scoliosis, vital capacity decreases by 4% per year following loss of ambulation, and this is due to a progressive respiratory muscle weakness. Progression of the scoliosis and an associated pelvic obliquity cause problems with posture and seating to the extent that quality of life may be severely impaired [1, 3, 5, 6, 7, 9, 12, 15, 16, 17, 18, 19, 20, 22, 23].
Whilst orthotic management combined with surgical treatment of contractures may prolong ambulation, there is no effective non-operative way of preventing progression of the scoliosis associated with DMD. Over the last 20 years, surgical intervention has been advocated as the treatment of choice for DMD scoliosis. The aim of surgery is to maintain the seated posture and balance in these patients, and thus their quality of life [2, 3, 5, 6, 7, 9, 12, 13, 15, 17, 18, 19, 20, 21, 22, 23]. Even though surgery removes the scoliotic contribution to deteriorating vital capacity, it improves neither pulmonary function nor life expectancy [7, 10, 11, 15, 19]. Although one study by Galasko et al. [4] found an improvement in respiratory function and survival following spinal fusion, this has not been supported by any other study.
It is recognised that DMD patients are at high risk of complications both during and following surgery, and many studies have been published quantifying them. These include adverse reactions to anaesthetic agents, large blood loss, prolonged ITU admission, temporary or permanent tracheotomies, respiratory infection and ventilator dependency. Patients are commonly in a poor state of health at the time of their surgery, and poor nutritional status, poor bone quality and respiratory compromise are all common. Only a few patients in published studies of surgery for scoliosis in DMD have had low forced vital capacities (FVCs). Indeed most authors suggest an FVC of 30–40% predicted values (PFVC) as being the minimum acceptable for surgery, thus depriving a significant number of patients from a possibly worthwhile intervention [9, 12, 13, 15, 17, 18, 19, 20, 23]. The purpose of this paper was to assess whether surgery could be performed safely in patients with a low FVC (less than 30% PVFC).
Materials and methods
Patients were identified who had a diagnosis of scoliosis secondary to DMD and had undergone spinal fusion procedures at the Royal National Orthopaedic Hospital, Stanmore between January 1990 and December 1999. The first author (A.M.) reviewed notes retrospectively and a standardised data collection form was completed. The following data were recorded: PFVC, FVC and forced expiratory volume in the 1st second (FEV1) estimated immediately pre-operatively, electrocardiogram (ECG) findings, echocardiogram results, weight, curve angle (pre- and post-operative), surgeon and procedure, age at surgery, estimated blood loss, operation ("skin to skin") time, intubation time, time until cessation of ventilatory support, complications and the duration of hospitalisation following surgery. The ventilatory support time was taken as the time from intubation up to the time when the patient was using solely a facemask without any mechanical support. Estimated blood loss was assessed by each anaesthetist at the end of the skin closure and was documented in the anaesthetic record.
Results
Thirty patients with a mean age of 14 years 8 months at surgery (range 11 years 2 months–19 years) were identified. They had become wheelchair dependent at a mean age of 11 years 4 months (range 7–17 years). All patients successfully underwent posterior spinal fusion and were discharged from hospital an average of 22 days post-operatively (range 13–62 days). None of the patients required permanent tracheotomy or ventilatory support on leaving hospital.
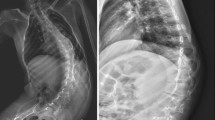
Forced vital capacities ranged from 18 to 60% of predicted values, with a mean of 33%. Thirteen patients had less than 30% PFVC. All patients had normal echocardiograms apart from two with impaired left ventricular function, one with dilated cardiomyopathy and one with a dilated left ventricle. Fourteen patients were tachycardic at rest. The mean pre-operative curve was 61°(range 30°–90°) and the mean number of levels fused was 15 (i.e. T3 to sacrum). The mean correction was 36° (range 16°–61°). Four surgeons performed all the operations, and the average operation time was 212 min (range 120–345 min). Four instrumentation systems were used: Colorado (11 cases), Harrington-Luque (11 cases), AO USS (4 cases) and Synergie (4 cases). Patients were anaesthetised by one of four consultant anaesthetists, all of whom were experienced in anaesthetising patients with myopathies and other syndromes.
Mean blood loss as recorded by the anaesthetist was 4.9 l (range 1.4–10 l), and the mean time intubated was 24 h (range 5 h–3 days, 16 h). Four patients required re-intubation, two of whom required temporary tracheotomy. Mean time on ventilatory support for all 30 patients was 77 h (range 5 h–23 days). If the two patients who required tracheotomy are removed from this series, the mean time on ventilatory support falls to 42 h (range 5 h–6 days, 3 h). Post-operatively, all the patients were managed in an orthopaedic intensive care unit until they no longer required any ventilatory support.
There were two wound infections, one of which required debridement and re-suturing under general anaesthetic. Major complications occurred in nine patients: one required 128 h (5 days, 8 h) of ventilatory support because of poor respiratory effort (25% PFVC), one had a pleural effusion, which was drained under ultrasound guidance (40% PFVC), one had a chest infection, which settled on BIPAP and antibiotics (30% PFVC) and two required re-intubation for respiratory exhaustion secondary to infection. One of these patients was intubated for 76 h with 147 h ventilatory support (31% PFVC) and the other was intubated for 73 h with 80 h ventilatory support (21% PFVC). One patient was successfully resuscitated following a cardiac arrest secondary to hyperkalaemia (55% PFVC) and two required temporary tracheotomies.
Of the two requiring temporary tracheotomies, the first had 34% PFVC and underwent a Colorado fusion from T2 to pelvis. The operation time was 180 min and the blood loss was 3.3 l. He was initially intubated for 30 h, but required re-intubation 8 days later due to pneumonia. A surgical tracheotomy was fashioned 3 days after re-intubation, and he required 552 h (23 days) of ventilatory support in total. His wound broke down and required debridement 19 days post-operatively. The tracheotomy was in place for 39 days and he spent 62 days in hospital. At discharge his wound was well healed and he required no ventilatory support.
The second patient had 20% PVFC and underwent a Harrington-Luque fusion from T3 to pelvis. The operation time was 3 h, with a blood loss of 2 l. He was initially extubated after 27 h, but suffered a respiratory arrest 3 days post-operatively. This was thought to be secondary to a tension pneumothorax, which was treated by needle decompression and intercostal tube drainage. He was re-intubated for 42 h, but developed a persistent pneumonia and required further re-intubation on day 12 post-operatively. A tracheotomy was fashioned the next day and remained in situ for 27 days. He required 510 h (21 days) of ventilatory support and he spent 50 days in hospital. At discharge, his wounds were well healed and he required no ventilatory support. Data for all the patients are presented in Table 1.
These patients can be divided into two groups: those with less than 30% PVFC (13 patients) and those with more than 30% (17 patients). Comparisons between the two groups can be seen in Table 2.
Although there are only small numbers involved in this study, statistical analysis was performed to try to identify any correlation between the data measured and outcome. No significant association was found between blood loss, age, weight, FEV1/FVC ratio, PFVC or curve angle and the duration of ventilatory support or intubation time.
Discussion
Studies have shown that non-ambulatory patients with DMD and scoliosis have a progressive deterioration in their deformity, which is not slowed with the use of orthoses [5, 9, 17]. The scoliosis is said to progress rapidly once ambulatory status is lost and, as their curve progresses, so do the problems associated with scoliosis. These take the form of poor posture and sitting balance, respiratory compromise, back pain and difficulty in handling of the patient.
Historically, curves of greater than 20–35° have been considered suitable for surgery, as the progression of the curve is associated with a marked decline in respiratory function [2, 3, 5, 7, 9, 13, 15, 17, 19, 21]. In addition, early spinal fusion has been suggested, as by the time the curve is greater than 35°, the FVC is almost always less than 40% PFVC [2, 7, 16, 19, 20, 21]. This gives the benefits of a faster procedure with less blood loss, a fuller correction of the scoliosis and a less turbulent post-operative period due to better respiratory function. Earlier surgery can, however, lead to some loss of height from premature growth arrest, though this is not classed as a problem [3].
Our group of 30 patients was divided into two groups for analysis: 13 patients with less than 30% PFVC and 17 with more than 30% PFVC. Considering the currently used criteria for surgery, the group of 13 with low FVCs normally would have been denied surgery.
Several surgical approaches to this condition have been described, and there has been debate regarding whether the fusion should be stopped at L5 or the pelvis [1, 9, 19]. As progression of the curve has been noted in patients fused to L5, fusion to the pelvis is the procedure of choice at our institution. This was also the procedure recommended by Alman and Kim following their review of 48 patients who had undergone spinal fusion for DMD in Toronto [1]. Fusion to L5 has been said to be faster than fusion to the pelvis, with less blood loss. In our series, average operation time (from first skin incision to the end of skin closure—the "skin to skin" time) was 212 min, compared to 270 min reported by Miller et al. [12] for fusions to the pelvis and 175 min reported by Fox et al. [3] for fusions to L5. Mubarak et al. [13] compared two cohorts from San Diego, reporting a mean operation time of 258 min for fusion to the pelvis and 225 min for fusions to L5.
In our group, blood loss was a mean of 4.9 l overall, with a mean loss of 3.8 l in the group with less than 30% PFVC and 5.8 l in the group with more than 30% PFVC. This is higher than most other reported series; volumes of 2.9 l [8], 3.6 l [19], 3.3 l [12] and 1.6 l [13] have been reported for fusions to the pelvis and 1.6 l [13] and 1.2 l [3] for fusion to L5.
It has been shown by Nordeen et al. [14] that patients with DMD bleed more during scoliosis surgery than do patients with other conditions undergoing similar procedures. This has been postulated as being due to a lack of dystrophin in vascular smooth muscle and a resulting poor vaso-constrictive response to surgical trauma. There is no evidence from this series of patients that progression of the disease measured by respiratory function causes increased blood loss. Indeed, there was a lower average blood loss in our low FVC group than in the higher FVC group.
Patients with DMD have a progressive restrictive lung disease that is partly due to the scoliosis and partly due to intercostal myopathy. This is reflected in a progressive decrease in FVC as the patient's age and spinal curvature increase [5, 7, 9, 12]. Decreased chest wall compliance, an ineffective cough and central and obstructive hypoxia also contribute to the respiratory failure. The timing of surgical intervention has been linked to the extent of the scoliosis and the FVC of the patient. Most papers have suggested an FVC of 30–40% PFVC as the cut-off for surgery, stating that the risk of respiratory complications is prohibitively high below this level [3, 9, 13, 15, 20, 21]. In this series of 30 patients, there were nine major complications. This is equivalent to a 30% complication rate, and compares favourably with other published series [3, 4, 8, 12, 13, 15, 22].
The patients with complications were not solely from the group with less than 30% PFVC. Five out of 17 patients (29%) with an FVC above 30% had complications (pleural effusion, pneumonia, cardiac arrest and pneumonia requiring temporary tracheotomy), compared to four out of 13 (30%) with an FVC of less than 30% (pneumonia each time). The mean period of ventilatory support was similar for the two groups, as was the length of post-operative stay. When the two patients who required tracheotomy are removed from the calculations, the difference between the two groups becomes even smaller (see Table 2).
This is the largest cohort of DMD patients with low FVCs to have received spinal fusion procedures, and the incidence of complications was no higher in this group of patients than it was in the group with higher FVCs. Only one patient had cardiomyopathy, and he required almost twice the mean intubation time, twice the mean ventilatory support time (excluding the two patients who required tracheotomies) and almost twice the mean post-operative stay. We feel that patients with cardiomyopathy are at a more advanced stage of the disease process, even though their FVC may be higher than 30% predicted values, and they therefore represent a relatively higher operative risk.
One of the reasons for the good results is the multi-disciplinary team involved with the patients' care. All the spinal fusions were performed by experienced spinal surgeons, with two-thirds of the procedures performed by three surgeons who specialise in spinal deformity. All patients were anaesthetised by one of four consultant anaesthetists, all of whom have considerable experience in the field of paediatric "syndromal" anaesthesia. Post-operatively, the patients were managed on an intensive care unit and, as their dependency decreased, on a high dependency unit, until they were off all ventilatory support. The nursing and physiotherapy staff were all experienced in the care of both disabled patients and their relatives. The final decision to proceed with surgery was made by the anaesthetist in charge, and this was made 2 weeks prior to planned surgery following a short admission for assessment.
Conclusions
The results obtained from this series of patients with an FVC below 30% of predicted values, who historically have been denied surgery, confirm that this group can safely undergo a spinal fusion procedure. These procedures should be performed in units that are staffed by experienced anaesthetists and spinal surgeons, and are equipped with an adequately staffed intensive care facility [7, 23]. Patients with DMD develop a progressive scoliosis that considerably lessens their quality of life. Although there is a weight of evidence to suggest that early operation before their FVC deteriorates below 30% of PFVC is the treatment of choice, on this evidence there is now no reason to deny a patient with DMD a spinal fusion procedure solely because their FVC is under 30% of predicted values.
References
Alman B, Kim H (1999) Pelvic obliquity after fusion of the spine in Duchenne muscular dystrophy. J Bone Joint Surg Br 81:821–824
Brooke M, Fenichel G, Griggs R, Mendell J, Moxley R, Florence J, et al (1989) Duchenne muscular dystrophy: patterns of clinical progression and effects of supportive therapy. Neurology 39:475–481
Fox H, Thomas C, Thompson A (1997) Spinal instrumentation for Duchenne muscular dystrophy: experience of hypotensive anaesthesia to minimise blood loss. J Paediatr Orthop 17:750–753
Galasko C, Delaney C, Morris P (1992) Spinal stabilisation in Duchenne muscular dystrophy. J Bone Joint Surg Br 74:210–214
Galasko C, Williamson J, Delaney C (1995) Lung function in Duchenne muscular dystrophy. Eur Spine J 4:263–267
Hsu JD (1983) The natural history of spine curvature progression in the nonambulatory Duchenne muscular dystrophy patient. Spine 8:771–775
Kennedy J, Staples A, Brook P, Parsons D, Sutherland A, Martin A, Stern L, Foster B (1995) Effect of spinal surgery on lung function in Duchenne muscular dystrophy. Thorax 50:1173–1178
LaPrade R, Rowe D (1992) The operative treatment of scoliosis in Duchenne muscular dystrophy. Orthop Rev 21:39–45
McCarthy R (1999) Management of neuromuscular scoliosis. Orthop Clin North Am 30:435–449
Miller F, Moseley C, Koreska J, Levison H (1988) Pulmonary function and scoliosis in Duchenne dystrophy. J Paediatr Orthop 8:133–137
Miller R, Chalmers A, Dao H, Filler-Katz A, Holman D, Bost F (1991) The effect of spine fusion on respiratory function in Duchenne muscular dystrophy. Neurology 41:38–40
Miller F, Mosely C, Koreska J (1992) Spinal fusion in Duchenne muscular dystrophy. Dev Med Child Neurol 34:775–786
Mubarak S, Morin W, Leach J (1993). Spinal fusion in Duchenne muscular dystrophy—fixation and fusion to the sacropelvis? J Paediatr Orthop 13:752–757
Noordeen MH, Haddad F, Muntoni F, Gobbi P, Hollyer J, Bentley G (1999) Blood loss in Duchenne's muscular dystrophy: vascular smooth muscle dysfunction? J Paediatr Orthop Part B 8:212–215
Ramirez N, Richards S, Warren P, Williams G (1997) Complications after posterior spinal fusion in Duchenne muscular dystrophy. J Paediatr Orthop 17:109–114
Rideau Y (1986) Prophylactic surgery for scoliosis in Duchenne muscular dystrophy. Dev Med Child Neurol 28:398–399
Rideau Y, Glorion B, Delaubier A, Tarle O, Bach J (1984) The treatment of scoliosis in Duchenne muscular dystrophy. Muscle Nerve 7:281–286
Sakai D, Hsu J, Bonnett C, Brown J (1977) Stabilization of the collapsing spine in Duchenne muscular dystrophy. Clin Orthop 128:256–260
Shapiro F, Sethna N, Colan S, Wohl M, Specht L (1992) Spinal fusion in Duchenne muscular dystrophy: a multidisciplinary approach. Muscle Nerve 15:604–614
Smith A, Koreska J, Eng P, Moseley C (1989) Progression of scoliosis in Duchenne muscular dystrophy. J Bone Joint Surg Am 71:1066–1074
Stricker U, Moser H, Aebi M (1996) Predominantly posterior instrumentation and fusion in neuromuscular and neurogenic scoliosis in children and adolescents. Eur Spine J 5:101–106
Sussman M (1985) Treatment of scoliosis in Duchenne muscular dystrophy. Dev Med Child Neurol 27:522–531
Weimann MD, Gibson DA, Moseley CF, Jones DC (1983) Surgical stabilisation of the spine in Duchenne Muscular Dystrophy. Spine 8:776–780
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marsh, A., Edge, G. & Lehovsky, J. Spinal fusion in patients with Duchenne's muscular dystrophy and a low forced vital capacity. Eur Spine J 12, 507–512 (2003). https://doi.org/10.1007/s00586-003-0545-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-003-0545-8