Abstract
Low tidal volume ventilation strategy may lead to atelectasis without proper positive end-expiratory pressure (PEEP) and recruitment maneuver (RM) settings. RM followed by individualized PEEP was a new method to optimize the intraoperative pulmonary function. We conducted a systematic review and network meta-analysis of randomized clinical trials to compare the effects of individualized PEEP + RM on intraoperative pulmonary function and hemodynamic with other PEEP and RM settings. The primary outcomes were intraoperative oxygenation index and dynamic compliance, while the secondary outcomes were intraoperative heart rate and mean arterial pressure. In total, we identified 15 clinical trials containing 36 randomized groups with 3634 participants. Ventilation strategies were divided into eight groups by four PEEP (L: low, M: moderate, H: high, and I: individualized) and two RM (yes or no) settings. The main results showed that IPEEP + RM group was superior to all other groups regarding to both oxygenation index and dynamic compliance. LPEEP group was inferior to LPEEP + RM, MPEEP, MPEEP + RM, and IPEEP + RM in terms of oxygenation index and LPEEP + RM, MPEEP, MPEEP + RM, HPEEP + RM, IPEEP, and IPEEP + RM in terms of dynamic compliance. All comparisons were similar for secondary outcomes. Our analysis suggested that individualized PEEP and RM may be the optimal low tidal volume ventilation strategy at present, while low PEEP without RM is not suggested.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pulmonary gas exchange and respiratory mechanics are impaired during general anesthesia, due to the collapse of alveolar [1]. Conventional ventilation strategy with high tidal volume (VT) > 10 ml/kg predicted body weight, no positive end-expiratory pressure (PEEP), or routine recruitment maneuver (RM) was once recommended to maintain the alveolar open, but was recently proved ineffective and even related to severe volutrauma and barotrauma [2, 3]. The current view suggests that sufficient PEEP and routine RM based on low VT (6-8 ml/kg predicted body weight) are the key points to maintain the alveolar open [2, 4, 5].
However, an excessive high PEEP may lead to barotrauma and hemodynamic instability; thus, the lowest PEEP that keeps the alveoli open is defined as “optimal PEEP”. The conclusions of previous studies showed a consistent controversy on the value of optimal PEEP [6,7,8]. At this background, a new concept named “individualized PEEP” was proposed, aiming at finding out the optimal PEEP according to patients’ individual characteristics such as lung dynamic compliance and driving pressure [9, 10].
The superiority of individualized PEEP over fixed PEEP was proved by recent studies in terms of intraoperative oxygenation index and respiratory mechanisms such as driving pressure and dynamic compliance [9,10,11,12], indicating less atelectrauma and barotrauma separately. However, the superiority was mostly concluded from the comparisons with moderate fixed PEEP (5–8 cm H2O) [13], while meta-analysis involving individualized PEEP is still absent. In addition, hemodynamic instability was another concern in the previous studies as individualized PEEP was usually higher than 10 cm H2O [9, 11].
We aimed at comprehensively evaluate the effects of individualized PEEP and RM based on low VT ventilation strategy on intraoperative pulmonary function and hemodynamics during abdominal surgery, in comparisons of other PEEP and RM settings. Since PEEP (low, moderate, high, and individualized) and RM (yes or no) has multiple levels, the conventional pairwise comparison meta-analysis is difficult to achieve our purpose. We finally performed this network meta-analysis (NMA) and systematic review of randomized controlled trials (RCTs) to provide a strong evidence for the benefits of individualized PEEP.
Materials and methods
The protocol for this NMA was registered with PROSPERO prospectively (identifier: CRD42020170614). The findings of this NMA was reported in accordance with the preferred reporting items for systematic reviews and meta-analyses–network meta-analyses (PRISMA-NMA) guidelines [14]. The PRISMA-NMA checklist can be found in Supplemental Digital Content 1.
Search strategy
Two authors (QZ and QQZ) independently searched PubMed, EMBASE and Cochrane Library for eligible studies. The results were updated in December 23, 2020. Our keywords of PubMed were (((((((((((((("Tidal Volume"[Mesh]) OR Tidal Volumes) OR Volume, Tidal) OR Volumes, Tidal))) OR (((((((((((((((((("Positive-Pressure Respiration"[Mesh]) OR Positive-Pressure Respiration) OR Positive-Pressure Respirations) OR Respiration, Positive-Pressure) OR Respirations, Positive-Pressure) OR Positive-Pressure Ventilation) OR Positive-Pressure Ventilation) OR Positive-Pressure Ventilations) OR Ventilation, Positive-Pressure) OR Ventilations, Positive-Pressure) OR Positive End-Expiratory Pressure) OR End-Expiratory Pressure, Positive) OR End-Expiratory Pressures, Positive) OR Positive End-Expiratory Pressure) OR Positive End-Expiratory Pressures) OR Pressure, Positive End-Expiratory) OR Pressures, Positive End-Expiratory)))) OR recruitment maneuver)) AND Randomized Controlled Trial[Publication Type]) NOT (((animals [Mesh] not (humans [Mesh] and animals [Mesh])))))))) AND abdominal.
Selection criteria
Two authors (ZLN and HLG) independently assessed the eligibility of studies by reading the titles, abstracts, and full texts. The chief investigator (JLC) arbitrated the disagreements and made final decisions. Studies were selected according to the following criteria:
(1) The participants were adult surgical patients undergoing supine position abdominal surgery requiring general anesthesia and low VT ventilation on volume-control mode.
(2) The ventilation strategies were classified by levels of PEEP and RM.
(3) Included studies should report comparisons among two or more different low VT ventilation strategies.
(4) We excluded studies that were not randomized controlled or written in English. Studies containing surgery in the lateral and prone position, and mechanical ventilation conducted by laryngeal mask also were excluded. However, we kept studies related to urology and gynecological surgery in the supine position.
Data extraction and quality assessment
Two authors (XCL and JW) extracted the following data from the original full texts: first author, publication year, study design, procedure and type of surgery, patients’ characteristics [age, gender, body mass index (BMI), ASA class, and sample size], ventilation settings (VT, PEEP, and RMs), and intraoperative pulmonary function and hemodynamic indicators [oxygenation index, dynamic compliance, driving pressure, mean arterial pressure (MAP), and heart rate]. Oxygenation index is calculated by arterial partial pressure of oxygen/inspiratory oxygen fraction, and is determined by the ventilation and gas exchange function of patient's respiratory system. For patients with healthy lungs, the oxygenation index mainly depends on the degree of alveolar opening. Dynamic compliance is calculated by VT/(airway peak pressure – PEEP). Compared with the static compliance [VT/(airway plateau pressure—PEEP)] measured at the end of inspiration period, dynamic compliance represents not only elasticity of lung tissue, but also airway resistance which derives from periodic decruitment/recruitment alveoli and small airways [15, 16]. Thus dynamic compliance is associated with the degree of end-expiration alveolar opening. Driving pressure is calculated by (airway plateau pressure – PEEP), and reflects the degree of ventilator-induced barotrauma [17].
Continuous data were extracted as mean and standard deviation. The continuous data presented as median, interquartile range, and range was transferred to mean and standard deviation according to recommendations from the Cochrane Collaboration: assuming that the median was equivalent to the mean, the interquartile range and range was, respectively, divided by 1.35 and 4 to evaluate the standard deviation [18]. If data were merely available in graphical format, then GetData Graph Digitizer 2.25 (http://getdata-graph-digitizer.com/) was used to quantify it.
The Cochrane Collaboration tool containing randomization bias, allocation bias, subjects blinding bias, outcome blinding bias, incomplete data bias, and selective reporting bias was applied to assess the methodological quality independently by two authors.
Outcomes
The primary outcomes were the intraoperative oxygenation index, dynamic compliance, and driving pressure. Secondary outcomes were the intraoperative heart rate and MAP.
Statistical analysis
We performed this NMA by STATA13.1 (Stata Corporation, College Station, TX) to compare the effects of different PEEP and RM settings based on low VT ventilation strategies on intraoperative oxygenation, lung dynamic compliance, heart rate, and MAP. The difference of mean, corresponding 95% CI, treatment rankings, probability of being best (PrBest), and surface under the cumulative ranking curve (SUCRA) values were estimated using the random-effects model. For indirect comparisons, a node-splitting model was conducted to estimate the degree of inconsistency. Z test was performed to assess the significance of the overall effect size. P < 0.05 was considered statistically significant. To ensure the reliability of the NMA, the number of included RCTs was required to be at least equal to the number of ventilation strategies.
The frequency method was applied to the fitted meta-regression model after constructing a heterogeneity matrix. The model treats covariates as the basic parameters and presumes that heterogeneity is independent of the comparison between effect sizes from multi-arm studies. Inconsistency reflects the differences between direct and indirect effects for the same comparison. We estimated the probability of a treatment being ranked at a specific place using “network rank”. “Comparison-adjusted” funnel plot was used to evaluate the publication bias. The funnel plot should be symmetrical near the zero line if there is no publication bias. The certainty and hence quality of included studies in terms of within-study bias, reporting bias, indirectness, imprecision, heterogeneity, incoherence, and confidence rating was assessed according to the grading of recommendations assessment, development and evaluation (GRADE) system [19] using the CINeMA web app [20].
Results
Baseline characteristics of included studies
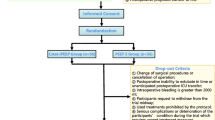
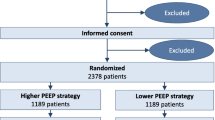
The initial databases search identified 810 studies. Duplicates (n = 320), unrelated to mechanical ventilation (n = 296), protocol without data (n = 11), and intervention beyond our classification criteria (n = 109) were excluded after reviewing the title and abstract. Forty-six of the remaining 74 studies were available for full text. After full-text review, non-randomized design (n = 4), non-English full text (n = 1), without clinical outcomes (n = 5), and unrelated ventilation strategies (n = 21) were further eliminated. Fifteen RCTs (n = 3634) met our selection criteria [6, 8, 11,12,13, 21,22,23,24,25,26,27,28,29,30]. The screening and inclusion process is presented in Fig. 1. In particular: one study reported in data for open and laparoscopic surgery separately, so we divided into 2 separate studies in the NMA [11].
Among the 15 RCTs, patients were divided by levels of PEEP (low, < 5 cm H2O; moderate, 5–8 cm H2O; high, > 8 cm H2O; individualized, decided by titration trial) and RM (yes or no) into eight groups: low PEEP + RM (LPEEP + RM), low PEEP (LPEEP), moderate PEEP + RM (MPEEP + RM), moderate PEEP (MPEEP), high PEEP + RM (HPEEP + RM), high PEEP (HPEEP), individualized PEEP + RM (IPEEP + RM), and individualized PEEP (IPEEP). The detailed baseline characteristics of the included studies are summarized in Table 1.
In this NMA, three studies were included in the IPEEP + RM group. All of them titrated the individualized PEEP through the RM-decremental titration trial-RM process, which consisted of one RM before and after the decremental PEEP titration trial separately [11, 12, 25]. The detailed steps are as follows: first, patients received an RM, usually with an open-lung pressure of 40 cm H2O and a higher one in obese patients, to open the alveoli. Then, a decremental PEEP titration trial was performed by decreasing PEEP step by step from a high level (20 or 25 cm H2O) until 5 cm H2O. The individualized PEEP was defined as the PEEP with optimal value of the titration parameter (electrical impedance tomography-related parameters in two studies [11, 12] and dynamic compliance in one study [25]). For prevention of the alveoli re-decruitment at the end of titration, another RM was performed before the application of individualized PEEP.
One study was included in the IPEEP group [13]. Its titration process was an incremental PEEP titration trial without RM, which had a same definition of individualized PEEP as the decremental trial.
Quality assessment
The details of the risk-of-bias assessment are summarized in Fig. 2. Fourteen studies reported clear randomization. Eleven studies reported allocation measures. Blinding methods for participants were absent in 7 studies and 6 studies lacked blinding methods for outcome assessors. Incomplete data were identified in 3 researches and selective reporting bias existed in 1 study.
The quality of evidence assessed by the GRADE system was moderate in all primary and secondary outcomes.
Evidence network
All network plots are presented in Fig. 3. Connecting lines indicated direct comparison, and indirect comparison among interventions can be performed by NMA. The size of nodes represents the overall sample size of each ventilation strategy and the width of connecting lines reflects the number of trials.
The network plots consisted of 5 triangular loops for oxygenation index, 2 triangular loops for dynamic compliance, 3 triangular loops for MAP, and 2 triangular loops for heart rate. For indirect comparisons, a node-splitting model was performed to estimate the degree of inconsistency. Inconsistency was found statistically significant for oxygenation index (P < 0.001 for loop moderate PEEP–moderate PEEP + RM–individualized PEEP + RM) and MAP (P = 0.016 for loop low PEEP–moderate PEEP–high PEEP, P = 0.035 for loop low PEEP–high PEEP + RM–high PEEP).
Primary outcomes
Oxygenation index
12 RCTs of 569 patients were included and all 8 groups were available for the intraoperative oxygenation index. The IPEEP + RM group was found out superior to all other groups (Table 2). The LPEEP group was proved to be inferior to the LPEEP + RM, MPEEP, and MPEEP + RM group. Furthermore, the IPEEP group was shown to be inferior to the MPEEP + RM group. The SUCRA, PrBest, and mean rank were: 100, 99.9%, and 1.0 for IPEEP + RM; 14.5, 0.0%, and 7.0 for LPEEP; 8.8, 0.0%, and 7.4 for IPEEP (Table 3).
Dynamic compliance
11 RCTs of 1369 patients were included and all 8 groups were available for the dynamic compliance. The IPEEP + RM was found out superior to all other groups (Table 2). The LPEEP group was proved to be inferior to all other groups except the HPEEP group. Furthermore, the HPEEP group was shown to be inferior to the MPEEP + RM and LPEEP + RM group, while the MPEEP group was inferior to the LPEEP + RM group. The SUCRA, PrBest, and mean rank were: 100, 100%, and 1.0 for IPEEP + RM; 0.8, 0.0%, and 7.9 for LPEEP (Table 3).
Driving pressure
There were only 4 studies that reported driving pressure, so the data were insufficient for NMA. The conclusion of raw studies suggested that driving pressure in IPEEP + RM group was lower than that in LPEEP + RM (P < 0.001), moderate PEEP (P < 0.001), and moderate PEEP + RM (P < 0.001) [6, 11, 12, 22]. The ventilation strategies, driving pressure, and P values are presented in Table 4.
Secondary outcomes
Mean arterial pressure
In regard to the mean arterial pressure, 10 RCTs of 2413 patients were included and all groups except IPEEP were available. The mean differences of all direct and indirect comparisons showed no significant difference (Table 2). The SUCRA, PrBest, and mean rank of all comparisons are presented in Table 3.
Heart rate
In regard to the heart rate, 9 RCTs of 3323 patients were included. Only LPEEP, MPEEP, HPEEP, HPEEP + RM, and IPEEP + RM groups were available. The mean differences of all direct and indirect comparisons showed no significant difference (Table 2). The SUCRA, PrBest, and mean rank of all comparisons are presented in Table 3.
Effects of recruitment maneuver
The mean differences between groups with same PEEP but different RM settings were merely significant in IPEEP + RM vs. IPEEP and LPEEP + RM vs. LPEEP, regarding to both intraoperative oxygenation index and dynamic compliance (Table 2).
The SUCRA, PrBest, and mean rank of both two primary outcomes were superior in all groups with RM than that in groups with same PEEP but without RM (Table 3).
Publication bias
The funnel plot of both primary outcomes is presented in Fig. 4 (oxygenation index) and Fig. 5 (dynamic compliance). The included studies were symmetrically distributed on both sides of the vertical line (x = 0), indicating no significant publication bias.
Discussion
The present NMA demonstrate that in terms of intraoperative pulmonary function and hemodynamics, individualized PEEP combined with RM may be the currently optimal low VT ventilation strategy, while low PEEP without RM was the worst low VT ventilation strategy. Also, evidence suggested that RM was associated with improvements in oxygenation index and dynamic compliance.
The lung-protective ventilation strategy (VT of 6 ml/kg, appropriate PEEP and RM) was proved superior to the conventional high VT ventilation strategy on the prognosis of acute respiratory distress syndrome (ARDS) patients, as a consequence of reduced volutrauma and barotrauma [3]. Inspired by this result, researchers tried to apply lung-protective ventilation strategy in patients undergoing intraoperative mechanical ventilation. However, there are two main problems exposed in clinical anesthesia. First, a low VT of 6 ml/kg was reasonable for ARDS patients to avoid excessive airway pressure but unnecessary for patients with healthy lungs. In addition, a tidal volume of 6 ml/kg is too low to be accepted by most anesthesiologists, compared with the traditional tidal volume of 10 ml/kg or higher. Therefore, most studies related to intraoperative ventilation strategy selected 8 ml/kg in groups receiving low tidal volume ventilation. Second, the low VT ventilation strategy also increased the risk of atelectasis due to insufficient PEEP. In the previous studies, low VT combined with low PEEP was associated with more serious atelectrauma and higher 30-day mortality in patients undergoing abdominal surgery and indicated the necessity of “optimal PEEP” setting [31]. Despite a series of efforts, no agreement has been reached on the optimal level of PEEP [6, 8, 31]. This debate may be attributed to applying one fixed PEEP to all patients, as their individual characteristics required different optimal PEEP. The concept of ‘individualized PEEP’ was then proposed to explore a more reasonable ventilation strategy [11].
Our NMA indicated a consistent strength of applying RM followed by individualized PEEP over other fixed PEEP strategies. The recent RCTs mainly revealed the advantages of individualized PEEP over low PEEP and moderate PEEP [9, 11, 32], while our NMA extended the conclusion to other fixed PEEP values. Higher oxygenation index and dynamic compliance suggested fewer collapsed alveoli. Based on current studies, two crucial points of the individualized PEEP may contribute to the alveoli opening effect. One is the variability of individualized PEEP. Even in non-obese patients undergoing open abdominal surgery, individualized PEEP could reach over 12 cm H2O. Such a high PEEP should be able to maintain most alveoli open. However, one included study revealed that compared with fixed PEEP of 2 cm H2O, a fixed PEEP of 12 cm H2O combined with RM did not lead to better intraoperative pulmonary function [6]. This contradictory conclusion can be explained by the other feature, large range of the individualized PEEP which is mostly over 10 cm H2O. The variability of individualized PEEP was probably caused by the individual characteristics such as chest wall compliance, abdominal pressure, pleural pressure, and surgical position. These inevitable high inter-individual heterogeneities strengthen the importance of individualizing the optimal PEEP.
The other crucial point of individualized PEEP is the correct titration process. In this NMA, all three studies in the IPEEP + RM group selected the RM-decremental titration trial-RM process [11, 12, 25]. The individualized PEEP was defined as the PEEP with optimal value of the titration parameter (electrical impedance tomography-related parameters in two studies [11, 12] and dynamic compliance in one study [25]). The included study in the IPEEP group used the incremental PEEP titration without RM, with the same definition of individualized PEEP as the decremental trial [13].
In our current study, the IPEEP + RM group was superior to IPEEP group in terms of both oxygenation index and dynamic compliance. One previous mathematical model revealed the possible reason that there was a consistent relationship between the PEEP level giving maximum lung compliance and the preset “open lung PEEP” (i.e., optimal PEEP) in the decremental trial with RM. This relationship, however, was inconsistent in the incremental trial without RM [33]. This hypothesis was later confirmed by a clinical trial related to obese patients with ARDS [34]. Therefore, we concluded that the individualized PEEP should be titrated under the RM-decremental titration-RM trial for consideration of higher intraoperative oxygenation and lung compliance.
Our NMA showed that RM improved the intraoperative oxygenation index and dynamic compliance in groups with RM especially in individualized PEEP and low PEEP groups, which were in line with previous RCTs [35, 36]. RM improved pulmonary function by overcoming the opening pressure, reverse atelectasis, and promote the benefits of PEEP [37]. The PEEP value applied during mechanical ventilation was usually insufficient for alveolar recruitment [38]; thus, a large amount of dorsal alveoli near the diaphragm may maintain collapsed without RM. In addition, evidence showed that even if RM was absent, the end-expiratory lung volume still increased along with the elevated level of PEEP [34]. That mean applying PEEP without RM ventilated air into the already open alveoli, inducing volutrauma and barotraumas and the injury was more severe when using higher PEEP. As the individualized PEEP is usually at a high level, the importance of RM should be considered seriously.
Based on the aforementioned effects of PEEP and RM, it is reasonable to believe that the low PEEP group has the worst oxygenation index. In the case of low VT, insufficient PEEP and lack of RM significantly increase the amount of atelectasis, leading to the impairment of gas exchange and respiratory mechanism. Previous studies also revealed that simply lowering VT without supplementing PEEP and RM would significantly increase the incidence of PPCs and even mortality in surgical patients, in comparison of high VT, zero PEEP, and no RM strategy [31, 39].
Our analysis of MAP and heart rate revealed a limited impact of different PEEP and RM settings on intraoperative hemodynamic, which is similar to previous studies. It is worth noting that hypotension is common during the titration trial of individualized PEEP though proved one-past and harmless [11, 12]. The possible reason for hemodynamic instability when applying individualized PEEP is that the appropriate level of PEEP keeps most alveoli open, improves oxygenation, and thus reduces pulmonary vascular resistance and right ventricular load [40].
This study is a relatively small NMA. Its limitations are as follows: first, we only included studies related to low VT ventilation strategies, without studies about conventional high VT strategy. Second, the analysis of the incidence of PPCs was absent, which should be an issue worth more attention than oxygenation and lung compliance. Of note, individualized PEEP was previously proved to increase mortality in patients with moderate-to-severe ARDS [41]. Furthermore, the maneuver of RM–titration–RM may induce airway peak pressure to reach even 40 cm H2O. It would inevitably lead to alveolar barotrauma, which is fatal for patients with severe lung injury. The data we initially extracted included the incidence of PPCs, but only 5 included studies reported the events of PPCs, and the data were insufficient for a proper NMA or even a conventional pairwise comparison meta-analysis. Therefore, further evidence is necessary before applying individualized PEEP as a routine strategy, and future studies should focus on the incidence of PPCs. Thirdly, two studies have much larger sample sizes than other studies [6, 8], which may increase the risk of type I and II errors. Fortunately, both two studies lack oxygenation index data, thus not included in the analyses of primary outcome.
Conclusion
In conclusion, our systematic review and NMA suggested that individualized PEEP combined with recruitment maneuver may be the optimal low VT ventilation strategy in abdominal surgery at present, while low PEEP without recruitment maneuver may be the worst one. Recruitment maneuver is able to improve the intraoperative pulmonary function in all PEEP levels. In our opinion, further research should focus on the direct comparison of the individualized PEEP to the high PEEP, in terms of not only functional but also “hard-core” indicators such as the incidence of PPCs and mortality.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- MAP:
-
Mean arterial pressure
- NMA:
-
Network meta-analysis
- PEEP:
-
Positive end-expiratory pressure
- PPC:
-
Postoperative pulmonary complication
- PrBest :
-
Probability of being best
- RCT:
-
Randomized controlled trial
- RM:
-
Recruitment maneuver
- SUCRA:
-
Surface under cumulative ranking curve
- V T :
-
Tidal volume
References
Reinius H, Jonsson L, Gustafsson S, Sundbom M, Duvernoy O, Pelosi P, Hedenstierna G, Freden F. Prevention of atelectasis in morbidly obese patients during general anesthesia and paralysis: a computerized tomography study. Anesthesiology. 2009;111(5):979–87.
Futier E, Constantin JM, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, Marret E, Beaussier M, Gutton C, Lefrant JY, Allaouchiche B, Verzilli D, Leone M, De Jong A, Bazin JE, Pereira B, Jaber S. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369(5):428–37.
Malhotra A. Low-tidal-volume ventilation in the acute respiratory distress syndrome. N Engl J Med. 2007;357(11):1113–20.
Ladha K, Vidal Melo MF, McLean DJ, Wanderer JP, Grabitz SD, Kurth T, Eikermann M. Intraoperative protective mechanical ventilation and risk of postoperative respiratory complications: hospital based registry study. BMJ (Clinical research ed). 2015;351:h3646.
Protti A, Andreis DT, Monti M, Santini A, Sparacino CC, Langer T, Votta E, Gatti S, Lombardi L, Leopardi O, Masson S, Cressoni M, Gattinoni L. Lung stress and strain during mechanical ventilation: any difference between statics and dynamics? Crit Care Med. 2013;41(4):1046–55.
Bluth T, Serpa Neto A, Schultz MJ, Pelosi P, Gama de Abreu M. Effect of intraoperative high positive end-expiratory pressure (PEEP) with recruitment maneuvers vs low PEEP on postoperative pulmonary complications in obese patients: a randomized clinical trial. Jama. 2019 Jun 18;321(23):2292-2305.
Wirth S, Kreysing M, Spaeth J, Schumann S. Intraoperative compliance profiles and regional lung ventilation improve with increasing positive end-expiratory pressure. Acta Anaesthesiol Scand. 2016;60(9):1241–50.
Hemmes SN, Gama de Abreu M, Pelosi P, Schultz MJ. High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet (London, England). 2014;384(9942):495–503.
Ferrando C, Soro M, Unzueta C, Suarez-Sipmann F, Canet J, Librero J, Pozo N, Peiro S, Llombart A, Leon I, India I, Aldecoa C, Diaz-Cambronero O, Pestana D, Redondo FJ, Garutti I, Balust J, Garcia JI, Ibanez M, Granell M, Rodriguez A, Gallego L, de la Matta M, Gonzalez R, Brunelli A, Garcia J, Rovira L, Barrios F, Torres V, Hernandez S, Gracia E, Gine M, Garcia M, Garcia N, Miguel L, Sanchez S, Pineiro P, Pujol R, Garcia-Del-Valle S, Valdivia J, Hernandez MJ, Padron O, Colas A, Puig J, Azparren G, Tusman G, Villar J, Belda J. Individualised perioperative open-lung approach versus standard protective ventilation in abdominal surgery (iPROVE): a randomised controlled trial. Lancet Respir Med. 2018;6(3):193–203.
Park M, Ahn HJ, Kim JA, Yang M, Heo BY, Choi JW, Kim YR, Lee SH, Jeong H, Choi SJ, Song IS. Driving pressure during thoracic surgery a randomized clinical trial. Anesthesiology. 2019;130(3):385–93.
Pereira SM, Tucci MR, Morais CCA, Simoes CM, Tonelotto BFF, Pompeo MS, Kay FU, Pelosi P, Vieira JE, Amato MBP. Individual positive end-expiratory pressure settings optimize intraoperative mechanical ventilation and reduce postoperative atelectasis. Anesthesiology. 2018;129(6):1070–81.
Nestler C, Simon P, Petroff D, Hammermüller S, Kamrath D, Wolf S, Dietrich A, Camilo LM, Beda A, Carvalho AR, Giannella-Neto A, Reske AW, Wrigge H. Individualized positive end-expiratory pressure in obese patients during general anaesthesia: a randomized controlled clinical trial using electrical impedance tomography. Br J Anaesth. 2017;119(6):1194–205.
Van Hecke D, Bidgoli JS, Van der Linden P. Does lung compliance optimization through PEEP manipulations reduce the incidence of postoperative hypoxemia in laparoscopic bariatric surgery? A randomized trial. Obes Surg. 2019;29(4):1268–75.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264-9w64.
Xu D, Wei W, Chen L, Li S, Lian M. Effects of different positive end-expiratory pressure titrating strategies on oxygenation and respiratory mechanics during one-lung ventilation: a randomized controlled trial. Ann Palliative Med. 2021;10(2):1133–1144.
Wirth S, Baur M, Spaeth J, Guttmann J, Schumann S. Intraoperative positive end-expiratory pressure evaluation using the intratidal compliance-volume profile. Br J Anaesth. 2015;114(3):483–90.
Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, Stewart TE, Briel M, Talmor D, Mercat A, Richard JC, Carvalho CR, Brower RG. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372(8):747–55.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions. 2nd Edition. Chichester (UK): John Wiley & Sons, 2019.
Salanti G, Del Giovane C, Chaimani A, Caldwell DM, Higgins JP. Evaluating the quality of evidence from a network meta-analysis. PLoS ONE. 2014;9(7):e99682.
Nikolakopoulou A, Higgins JPT, Papakonstantinou T, Chaimani A, Del Giovane C, Egger M, Salanti G. CINeMA: an approach for assessing confidence in the results of a network meta-analysis. PLoS Med. 2020;17(4):e1003082.
You AH, Song Y, Kim DH, Suh J, Baek JW, Han DW. Effects of positive end-expiratory pressure on intraocular pressure and optic nerve sheath diameter in robot-assisted laparoscopic radical prostatectomy: a randomized, clinical trial. Medicine. 2019;98(14):e15051.
Wei K, Min S, Cao J, Hao X, Deng J. Repeated alveolar recruitment maneuvers with and without positive end-expiratory pressure during bariatric surgery: A randomized trial. Minerva Anestesiol. 2018;84(4):463–72.
Ciftci B, Aksoy M, Ince I, Ahıskalıoglu A, Yılmazel UE. The effects of positive end-expiratory pressure at different levels on postoperative respiration parameters in patients undergoing laparoscopic cholecystectomy. J Invest Surg. 2018;31(2):114–20.
Sargin M, Uluer MS, Özmen S. Comparison of the effects of different positive end-expiratory pressure levels on cerebral oxygen saturation with near infrared spectroscopy during laparoscopic cholecystectomy. Surg Laparosc Endosc Percutaneous Tech. 2017;27(1):30–5.
Ferrando C, Suarez-Sipmann F, Tusman G, Leon I, Romero E, Gracia E, Mugarra A, Arocas B, Pozo N, Soro M, Belda FJ. Open lung approach versus standard protective strategies: effects on driving pressure and ventilatory efficiency during anesthesia—a pilot, randomized controlled trial. PLoS ONE. 2017;12(5):e0177399.
Chin JH, Kim WJ, Lee J, Han YA, Lim J, Hwang JH, Cho SS, Kim YK. Effect of positive end-expiratory pressure on the sonographic optic nerve sheath diameter as a surrogate for intracranial pressure during robot-assisted laparoscopic prostatectomy: a randomized controlled trial. PloS One. 2017;12(1):e0170369
Ahn S, Byun SH, Chang H, Koo YB, Kim JC. Effect of recruitment maneuver on arterial oxygenation in patients undergoing robot-assisted laparoscopic prostatectomy with intraoperative 15 cmH2O positive end expiratory pressure. Korean J Anesthesiol. 2016;69(6):592–8.
Pi X, Cui Y, Wang C, Guo L, Sun B, Shi J, Lin Z, Zhao N, Wang W, Fu S, Li E. Low tidal volume with PEEP and recruitment expedite the recovery of pulmonary function. Int J Clin Exp Pathol. 2015;8(11):14305–14.
Russo A, Di Stasio E, Scagliusi A, Bevilacqua F, Isgrò MA, Marana R, Marana E. Positive end-expiratory pressure during laparoscopy: cardiac and respiratory effects. J Clin Anesth. 2013;25(4):314–20.
Kwak HJ, Park SK, Lee KC, Lee DC, Kim JY. High positive end-expiratory pressure preserves cerebral oxygen saturation during laparoscopic cholecystectomy under propofol anesthesia. Surg Endosc. 2013;27(2):415–20.
Levin MA, McCormick PJ, Lin HM, Hosseinian L, Fischer GW. Low intraoperative tidal volume ventilation with minimal PEEP is associated with increased mortality. Br J Anaesth. 2014;113(1):97–108.
Ferrando C, Mugarra A, Gutierrez A, Carbonell JA, Garcia M, Soro M, Tusman G, Belda FJ. Setting individualized positive end-expiratory pressure level with a positive end-expiratory pressure decrement trial after a recruitment maneuver improves oxygenation and lung mechanics during one-lung ventilation. Anesth Analg. 2014;118(3):657–65.
Hickling KG. Best compliance during a decremental, but not incremental, positive end-expiratory pressure trial is related to open-lung positive end-expiratory pressure: a mathematical model of acute respiratory distress syndrome lungs. Am J Respir Crit Care Med. 2001;163(1):69–78.
Fumagalli J, Santiago RRS, Teggia Droghi M, Zhang C, Fintelmann FJ, Troschel FM, Morais CCA, Amato MBP, Kacmarek RM, Berra L. Lung recruitment in obese patients with acute respiratory distress syndrome. Anesthesiology. 2019;130(5):791–803.
Hedenstierna G, Rothen HU. Respiratory function during anesthesia: effects on gas exchange. Compr Physiol. 2012;2(1):69–96.
Fernandez-Bustamante A, Hashimoto S, Serpa Neto A, Moine P, Vidal Melo MF, Repine JE. Perioperative lung protective ventilation in obese patients. BMC Anesthesiol. 2015;15:56.
Guldner A, Kiss T, Serpa de Neto A, Hemmes SN, Canet J, Spieth PM, Rocco PR, Schultz MJ, Pelosi P, Gama AM. Intraoperative protective mechanical ventilation for prevention of postoperative pulmonary complications: a comprehensive review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuvers. Anesthesiology. 2015;123(3):692–713.
Imber DA, Pirrone M, Zhang C, Fisher DF, Kacmarek RM, Berra L. Respiratory management of perioperative obese patients. Respir Care. 2016;61(12):1681–92.
Stewart TE, Meade MO, Cook DJ, Granton JT, Hodder RV, Lapinsky SE, Mazer CD, McLean RF, Rogovein TS, Schouten BD, Todd TR, Slutsky AS. Evaluation of a ventilation strategy to prevent barotrauma in patients at high risk for acute respiratory distress syndrome. Pressure- and volume-limited ventilation strategy group. N Engl J Med. 1998;338(6):355–61.
Gernoth C, Wagner G, Pelosi P, Luecke T. Respiratory and haemodynamic changes during decremental open lung positive end-expiratory pressure titration in patients with acute respiratory distress syndrome. Crit Care (London, England). 2009;13(2):R59.
Cavalcanti AB, Suzumura ÉA, Laranjeira LN, Paisani DM, Damiani LP, Guimarães HP, Romano ER, Regenga MM, Taniguchi LNT, Teixeira C, Pinheiro de Oliveira R, Machado FR, Diaz-Quijano FA, Filho MSA, Maia IS, Caser EB, Filho WO, Borges MC, Martins PA, Matsui M, Ospina-Tascón GA, Giancursi TS, Giraldo-Ramirez ND, Vieira SRR, Assef M, Hasan MS, Szczeklik W, Rios F, Amato MBP, Berwanger O, Ribeiro de Carvalho CR. Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2017;318(14):1335–45.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conceptualization: Jun-Li Cao, Yuan Han, He Liu, and Xiang Li; methodology: Xiu-Cheng Liu, Qiu Zhao, Qian-Qian Zhang, and Jun Wang; formal analysis: Xiang Li, Ming-Sheng Dai, Yang Zhou, Xiao-Yi Hu, and Xun Sun; investigation: Zhi-Lin Ni, Hui-Lian Guan, Xing Gao, and Jian Zhou; writing—original draft preparation: Zhi-Lin Ni, Xiu-Cheng Liu, Hui-Lian Guan, Ming-Sheng Dai, Xing Gao, Yang Zhou, and Xiao-Yi Hu; writing—review & editing: Jun-Li Cao, Yuan Han, He Liu, Xiang Li, Xun Sun, Jian Zhou, Qiu Zhao, Qian-Qian Zhang, and Jun Wang. Xiang Li, Zhi-Lin Ni, Jun Wang, and Xiu-Cheng Liu are co-first authors and contribute equally to this work. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The author reports no conflicts of interest in this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Li, X., Ni, ZL., Wang, J. et al. Effects of individualized positive end-expiratory pressure combined with recruitment maneuver on intraoperative ventilation during abdominal surgery: a systematic review and network meta-analysis of randomized controlled trials. J Anesth 36, 303–315 (2022). https://doi.org/10.1007/s00540-021-03012-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-021-03012-9