Abstract
Purpose
The aim of the study was to evaluate the effects of high-dose nitroglycerine (NTG) on glucose metabolism, tissue oxygenation and postoperative recovery in cardiac surgical patients.
Methods
Cardiac surgical patients in the retrospective survey were classified into two groups based on the NTG regimen. NTG group had intravenous loading of NTG (infusion rate 10–20 mg/h with total dose of ≥0.5 mg/kg) starting at rewarming of cardiopulmonary bypass (CPB) (n = 101), and control group had no intravenous loading of NTG (n = 151). Data for intraoperative plasma glucose and lactate levels, and regular insulin consumption were collected. Propensity score methodology was utilized to adjust for potential confounders.
Results
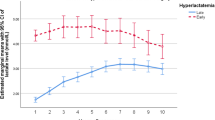
After adjustment for propensity score, the plasma glucose was significantly lower in the NTG group during (161 ± 39 versus 179 ± 45 mg/dl, p = 0.005) and after CPB (167 ± 41 versus 184 ± 48 mg/dl, p = 0.012). Total consumption of regular insulin was significantly lower in the NTG group, median 8 (range 0–50) versus 13 (0–90) international units, p = 0.005. There was a trend towards statistical significance in a lower incidence of hyperlactatemia (>2.2 mmol/l) in the NTG group during CPB, 21/100 (21 %) versus 40/132 (30.3 %), p = 0.065. The mixed venous oxygen saturation in the intensive care unit was higher in the NTG group, 65 ± 9 versus 62 ± 11 %, p = 0.056.
Conclusions
Intravenous loading of NTG during and after CPB is safe and effective for attenuating the hyperglycemic response and reduce the incidence of hyperlactatemia during cardiac surgery with CPB.



Similar content being viewed by others
References
Koning NJ, Vonk AB, Meesters MI, Oomens T, Verkaik M, Jansen EK, Baufreton C, Boer C. Microcirculatory perfusion is preserved during off-pump but not on-pump cardiac surgery. J Cardiothorac Vasc Anesth. 2014;28:336–41.
Atasever B, Boer C, Goedhart P, Biervliet J, Seyffert J, Speekenbrink R, Schwarte L, de Mol B, Ince C. Distinct alterations in sublingual microcirculatory blood flow and hemoglobin oxygenation in on-pump and off-pump coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth. 2011;25:784–90.
De Backer D, Dubois MJ, Schmartz D, Koch M, Ducart A, Barvais L, Vincent JL. Microcirculatory alterations in cardiac surgery: effects of cardiopulmonary bypass and anesthesia. Ann Thorac Surg. 2009;88:1396–403.
Bauer A, Kofler S, Thiel M, Eifert S, Christ F. Monitoring of the sublingual microcirculation in cardiac surgery using orthogonal polarization spectral imaging: preliminary results. Anesthesiology. 2007;107:939–45.
Krinsley JS, Grover A. Severe hypoglycemia in critically ill patients: risk factors and outcomes. Crit Care Med. 2007;35:2262–7.
Thorell A, Nygren J, Ljungqvist O. Insulin resistance: a marker of surgical stress. Curr Opin Clin Nutr Metab Care. 1999;2:69–78.
den Uil CA, Caliskan K, Lagrand WK, van der Ent M, Jewbali LS, van Kuijk JP, Spronk PE, Simoons ML. Dose-dependent benefit of nitroglycerin on microcirculation of patients with severe heart failure. Intensive Care Med. 2009;35:1893–9.
den Uil CA, Lagrand WK, Spronk PE, van der Ent M, Jewbali LS, Brugts JJ, Ince C, Simoons ML. Low-dose nitroglycerin improves microcirculation in hospitalized patients with acute heart failure. Eur J Heart Fail. 2009;11:386–90.
Lima A, van Genderen ME, van Bommel J, Klijn E, Jansem T, Bakker J. Nitroglycerin reverts clinical manifestations of poor peripheral perfusion in patients with circulatory shock. Crit Care. 2014;18:R126.
Hatsuoka S, Sakamoto T, Stock UA, Nagashima M, Mayer JE Jr. Effect of l-arginine or nitroglycerine during deep hypothermic circulatory arrest in neonatal lambs. Ann Thorac Surg. 2003;75:197–203.
Cepeda MS, Boston R, Farrar JT, Strom BL. Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. Am J Epidemiol. 2003;158:280–7.
Anand KJ, Hansen DD, Hickey PR. Hormonal-metabolic stress responses in neonates undergoing cardiac surgery. Anesthesiology. 1990;73:661–70.
van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359–67.
Qaseem A, Humphrey LL, Chou R, Snow V, Shekelle P, Clinical Guidelines Committee of the American College of Physicians. Use of intensive insulin therapy for the management of glycemic control in hospitalized patients: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2011;154:260–7.
Bucerius J, Gummert JF, Walther T, Doll N, Falk V, Onnasch JF, Barten MJ, Mohr FW. Impact of diabetes mellitus on cardiac surgery outcome. Thorac Cardiovasc Surg. 2003;51:11–6.
Boyle EM Jr, Lille ST, Allaire E, Clowes AW, Verrier ED. Endothelial cell injury in cardiovascular surgery: atherosclerosis. Ann Thorac Surg. 1997;63:885–94.
Sellke FW, Boyle EM Jr, Verrier ED. Endothelial cell injury in cardiovascular surgery: the pathophysiology of vasomotor dysfunction. Ann Thorac Surg. 1996;62:1222–8.
Kovacs P, Szilvassy Z, Hegyi P, Nemeth J, Ferdinandy P, Tosaki A. Effect of transdermal nitroglycerin on glucose-stimulated insulin release in healthy male volunteers. Eur J Clin Invest. 2000;30:41–4.
Jedrzkiewicz S, Parker JD. Acute and chronic effects of glyceryl trinitrate therapy on insulin and glucose regulation in humans. J Cardiovasc Pharmacol Ther. 2013;18:211–6.
Fox-Robichaud A, Payne D, Hasan SU, Ostrovsky L, Fairhead T, Reinhardt P, Kubes P. Inhaled NO as a viable antiadhesive therapy for ischemia/reperfusion injury of distal microvascular beds. J Clin Invest. 1998;101:2497–505.
Nevière R, Guery B, Mordon S, Zerimech F, Charré S, Wattel F, Chopin C. Inhaled NO reduces leukocyte-endothelial cell interactions and myocardial dysfunction in endotoxemic rats. Am J Physiol Heart Circ Physiol. 2000;278:H1783–90.
Liu X, Huang Y, Pokreisz P, Vermeersch P, Marsboom G, Swinnen M, Verbeken E, Santos J, Pellens M, Gillijns H, Van de Werf F, Bloch KD, Janssens S. Nitric oxide inhalation improves microvascular flow and decreases infarction size after myocardial ischemia and reperfusion. J Am Coll Cardiol. 2007;50:808–17.
Yu B, Raher MJ, Volpato GP, Bloch KD, Ichinose F, Zapol WM. Inhaled nitric oxide enables artificial blood transfusion without hypertension. Circulation. 2008;117:1982–90.
Baron DM, Yu B, Lei C, Bagchi A, Beloiartsev A, Stowell CP, Steinbicker AU, Malhotra R, Bloch KD, Zapol WM. Pulmonary hypertension in lambs transfused with stored blood is prevented by breathing nitric oxide. Anesthesiology. 2012;116:637–47.
Duncan HP, Cloote A, Weir PM, Jenkins I, Murphy PJ, Pawade AK, Rogers CA, Wolf AR. Reducing stress responses in the pre-bypass phase of open heart surgery in infants and young children: a comparison of different fentanyl doses. Br J Anaesth. 2000;84:556–64.
Bakker J, Gris P, Coffernils M, Kahn RJ, Vincent JL. Serial blood lactate levels can predict the development of multiple organ failure following septic shock. Am J Surg. 1996;171:221–6.
Jansen TC, van Bommel J, Woodward R, Mulder PG, Bakker J. Association between blood lactate levels, sequential organ failure assessment subscores, and 28-day mortality during early and late intensive care unit stay: a retrospective observational study. Crit Care Med. 2009;37:2369–74.
Fall PJ, Szerlip HM. Lactic acidosis: from sour milk to septic shock. J Intensive Care Med. 2005;20:255–71.
McNelis J, Marini CP, Jurkiewicz A, Szomstein S, Simms HH, Ritter G, Nathan IM. Prolonged lactate clearance is associated with increased mortality in the surgical intensive care unit. Am J Surg. 2001;182:481–5.
Arnold RC, Shapiro NI, Jones AE, Schorr C, Pope J, Casner E, Parrillo JE, Dellinger RP, Trzeciak S, Emergency Medicine Shock Research Network (EMShockNet) Investigators. Multicenter study of early lactate clearance as a determinant of survival in patients with presumed sepsis. Shock. 2009;32:35–9.
Pearse R, Dawson D, Fawcett J, Rhodes A, Grounds RM, Bennett ED. Changes in central venous saturation after major surgery, and association with outcome. Crit Care. 2005;9:R694–9.
Pölönen P, Ruokonen E, Hippeläinen M, Pöyhönen M, Takala J. A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients. Anesth Analg. 2000;90:1052–9.
Howard RJ, Crain C, Franzini DA, Hood CI, Hugli TE. Effects of cardiopulmonary bypass on pulmonary leukostasis and complement activation. Arch Surg. 1988;123:1496–501.
McGowan FX Jr, Ikegami M, del Nido PJ, Motoyama EK, Kurland G, Davis PJ, Siewers RD. Cardiopulmonary bypass significantly reduces surfactant activity in children. J Thorac Cardiovasc Surg. 1993;106:968–77.
Bin JP, Doctor A, Lindner J, Hendersen EM, Le DE, Leong-Poi H, Fisher NG, Christiansen J, Kaul S. Effects of nitroglycerin on erythrocyte rheology and oxygen unloading: novel role of S-nitrosohemoglobin in relieving myocardial ischemia. Circulation. 2006;113:2502–8.
Skrzypchak AM, Lafayette NG, Bartlett RH, Zhou Z, Frost MC, Meyerhoff ME, Reynolds MM, Annich GM. Effect of varying nitric oxide release to prevent platelet consumption and preserve platelet function in an in vivo model of extracorporeal circulation. Perfusion. 2007;22:193–200.
Martins e Silva J, Saldanha C. Arterial endothelium and atherothrombogenesis—intact endothelium in vascular and blood homeostasis. Rev Port Cardiol. 2006;25:1061–83.
Pye M, Oldroyd KG, Conkie JA, Hutton I, Cobbe SM. A clinical and in vitro study on the possible interaction of intravenous nitrates with heparin anticoagulation. Clin Cardiol. 1994;17:658–61.
Koh KK, Park GS, Song JH, Moon TH, In HH, Kim JJ, Lee HJ, Cho SK, Kim SS. Interaction of intravenous heparin and organic nitrates in acute ischemic syndromes. Am J Cardiol. 1995;76:706–9.
Vermeulen Windsant IC, de Wit NC, Sertorio JT, Beckers EA, Tanus-Santos JE, Jacobs MJ, Buurman WA. Blood transfusions increase circulating plasma free hemoglobin levels and plasma nitric oxide consumption: a prospective observational pilot study. Crit Care. 2012;16:R95.
Gaies MG, Gurney JG, Yen AH, Napoli ML, Gajarski RJ, Ohye RG, Charpie JR, Hirsch JC. Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med. 2010;11:234–8.
Arnold RC, Dellinger RP, Parrillo JE, Chansky ME, Lotano VE, McCoy JV, Jones AE, Shapiro NI, Hollenberg SM, Trzeciak S. Discordance between microcirculatory alterations and arterial pressure in patients with hemodynamic instability. J Crit Care. 2012;27:531.e1–537.e1.
Boerma EC, Ince C. The role of vasoactive agents in the resuscitation of microvascular perfusion and tissue oxygenation in critically ill patients. Intensive Care Med. 2010;36:2004–18.
De Backer D, Creteur J, Dubois MJ, Sakr Y, Koch M, Verdant C, Vincent JL. The effects of dobutamine on microcirculatory alterations in patients with septic shock are independent of its systemic effects. Crit Care Med. 2006;34:403–8.
Atasever B, Boer C, van der Kuil M, Lust E, Beishuizen A, Speekenbrink R, Seyffert J, de Mol B, Ince C. Quantitative imaging of microcirculatory response during nitroglycerin-induced hypotension. J Cardiothorac Vasc Anesth. 2011;25:140–4.
Hogue CW Jr, Palin CA, Arrowsmith JE. Cardiopulmonary bypass management and neurologic outcomes: an evidence-based appraisal of current practices. Anesth Analg. 2006;103:21–37.
Maier S, Hasibeder WR, Hengl C, Pajk W, Schwarz B, Margreiter J, Ulmer H, Engl J, Knotzer H. Effects of phenylephrine on the sublingual microcirculation during cardiopulmonary bypass. Br J Anaesth. 2009;102:485–91.
Spronk PE, Ince C, Gardien MJ, Mathura KR, Oudemans-van Straaten HM, Zandstra DF. Nitroglycerin in septic shock after intravascular volume resuscitation. Lancet. 2002;360:1395–6.
Boerma EC, Koopmans M, Konijn A, Kaiferova K, Bakker AJ, van Roon EN, Buter H, Bruins N, Egbers PH, Gerritsen RT, Koetsier PM, Kingma WP, Kuiper MA, Ince C. Effects of nitroglycerin on sublingual microcirculatory blood flow in patients with severe sepsis/septic shock after a strict resuscitation protocol: a double-blind randomized placebo controlled trial. Crit Care Med. 2010;38:93–100.
Acknowledgments
YHT contributed to data collection and manuscript drafting. KYC contributed to statistical review. SWL assisted in study design. CCL, KCC and CCS helped manage and care for the patients. CCL and STH were involved in revising the manuscript critically for important intellectual content. MYT gave final approval of the version to be published and agreed to be accountable for ensuring the accuracy or integrity of the work. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no financial or other relationships to disclose that might lead to a conflict of interest regarding this article.
Appendix
About this article
Cite this article
Tai, YH., Chang, KY., Liao, SW. et al. Intravenous loading of nitroglycerin during rewarming of cardiopulmonary bypass improves metabolic homeostasis in cardiac surgery: a retrospective analysis. J Anesth 30, 779–788 (2016). https://doi.org/10.1007/s00540-016-2207-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-016-2207-0