Abstract
Purpose
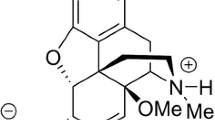
Ketamine, a noncompetitive N-methyl-d-aspartate receptor antagonist, has been used for the treatment of cancer pain as an analgesic adjuvant to opioids. However, ketamine is known to produce psychotomimetic side effects including cognitive impairments under a high-dose situation, presumably as the result of cortical dysfunction. Here, we investigated whether low-dose ketamine was useful as an analgesic adjuvant to morphine for pain control, focusing on frontocortical function.
Methods
To assess the analgesic effects of ketamine with or without morphine, we performed behavioral and histochemical experiments, using the hot plate test and c-Fos expression analysis in rats. The effect on cortical function was also determined by prepulse inhibition (PPI) of the acoustic startle and evoked potentials in the hippocampal CA1-medial prefrontal cortex (mPFC) synapses as measures of synaptic efficacy.
Results
Coadministration of ketamine as a subanalgesic dose significantly enhanced intraperitoneal morphine-induced antinociceptive response, which was measured as the increased reaction latency in the hot plate test. In addition, the noxious thermal stimulus-induced c-Fos expression in the ventrolateral periaqueductal gray matter was significantly suppressed by concomitant ketamine and morphine. In contrast, the subanalgesic dose of ketamine did not impair PPI and synaptic efficacy in the mPFC.
Conclusion
The present results indicate that the morphine-induced analgesic effect is enhanced by a concomitant subanalgesic dose of ketamine without affecting cortical function. Our findings possibly support the clinical notion that low-dose ketamine as an analgesic adjuvant has therapeutic potential to reduce opioid dosage, thereby improving the quality of life in cancer pain patients.





Similar content being viewed by others
References
De Kock MF, Lavand’homme PM. The clinical role of NMDA receptor antagonists for the treatment of postoperative pain. Best Pract Res Clin Anaesthesiol. 2007;21(1):85–98.
Subramaniam K, Subramaniam B, Steinbrook RA. Ketamine as adjuvant analgesic to opioids: a quantitative and qualitative systematic review. Anesth Analg 2004;99(2):482–495.
Salas S, Frasca M, Planchet-Barraud B, Burucoa B, Pascal M, Lapiana JM, Hermet R, Castany C, Ravallec F, Loundou A, Auquier P, Duffaud F, Baumstarck K. Ketamine analgesic effect by continuous intravenous infusion in refractory cancer pain: considerations about the clinical research in palliative care. J Palliat Med. 2012;15(3):287–93.
Luginbühl M, Gerber A, Schnider TW, Petersen-Felix S, Arendt-Nielsen L, Curatolo M. Modulation of remifentanil-induced analgesia, hyperalgesia, and tolerance by small-dose ketamine in humans. Anesth Analg 2003;96(3):726–732.
Bell R, Eccleston C, Kalso E. Ketamine as an adjuvant to opioids for cancer pain. Cochrane Database Syst Rev 2003(1):CD003351.
Kissin I, Bright CA, Bradley EL. The effect of ketamine on opioid-induced acute tolerance: can it explain reduction of opioid consumption with ketamine-opioid analgesic combinations? Anesth Analg. 2000;91(6):1483–8.
Célèrier E, Rivat C, Jun Y, Laulin JP, Larcher A, Reynier P, Simonnet G. Long-lasting hyperalgesia induced by fentanyl in rats: preventive effect of ketamine. Anesthesiology. 2000;92(2):465–72.
Laulin JP, Maurette P, Corcuff JB, Rivat C, Chauvin M, Simonnet G. The role of ketamine in preventing fentanyl-induced hyperalgesia and subsequent acute morphine tolerance. Anesth Analg 2002;94(5):1263–1269.
Rivat C, Laulin JP, Corcuff JB, Célèrier E, Pain L, Simonnet G. Fentanyl enhancement of carrageenan-induced long-lasting hyperalgesia in rats: prevention by the N-methyl-d-aspartate receptor antagonist ketamine. Anesthesiology. 2002;96(2):381–91.
Pelissier T, Laurido C, Kramer V, Hernández A, Paeile C. Antinociceptive interactions of ketamine with morphine or methadone in mononeuropathic rats. Eur J Pharmacol. 2003;477(1):23–8.
Mehta AK, Halder S, Khanna N, Tandon OP, Singh UR, Sharma KK. Role of NMDA and opioid receptors in neuropathic pain induced by chronic constriction injury of sciatic nerve in rats. J Basic Clin Physiol Pharmacol. 2012;23(2):49–55.
Tandon OP, Mehta AK, Halder S, Khanna N, Sharma KK. Peripheral interaction of opioid and NMDA receptors in inflammatory pain in rats. Indian J Physiol Pharmacol. 2010;54(1):21–31.
Rodríguez-Muñoz M, Sánchez-Blázquez P, Vicente-Sánchez A, Berrocoso E, Garzón J. The mu-opioid receptor and the NMDA receptor associate in PAG neurons: implications in pain control. Neuropsychopharmacology. 2012;37(2):338–49.
Morris BJ, Cochran SM, Pratt JA. PCP: from pharmacology to modelling schizophrenia. Curr Opin Pharmacol. 2005;5(1):101–6.
Javitt DC, Rabinowicz E, Silipo G, Dias EC. Encoding vs. retention: differential effects of cue manipulation on working memory performance in schizophrenia. Schizophr Res. 2007;91(1-3):159–68.
Mandillo S, Rinaldi A, Oliverio A, Mele A. Repeated administration of phencyclidine, amphetamine and MK-801 selectively impairs spatial learning in mice: a possible model of psychotomimetic drug-induced cognitive deficits. Behav Pharmacol. 2003;14(7):533–44.
Seillier A, Giuffrida A. Evaluation of NMDA receptor models of schizophrenia: divergences in the behavioral effects of sub-chronic PCP and MK-801. Behav Brain Res. 2009;204(2):410–5.
Newcomer JW, Farber NB, Jevtovic-Todorovic V, Selke G, Melson AK, Hershey T, Craft S, Olney JW. Ketamine-induced NMDA receptor hypofunction as a model of memory impairment and psychosis. Neuropsychopharmacology. 1999;20(2):106–18.
Morgan CJ, Riccelli M, Maitland CH, Curran HV. Long-term effects of ketamine: evidence for a persisting impairment of source memory in recreational users. Drug Alcohol Depend. 2004;75(3):301–8.
Yoshizawa K, Mori T, Ueno T, Nishiwaki M, Shibasaki M, Shimizu N, Narita M, Suzuki T. Involvement of serotonin receptor mechanisms in the discriminative stimulus effects of ketamine in rats. J Pharmacol Sci. 2013;121(3):237–41.
Williams GV, Goldman-Rakic PS. Modulation of memory fields by dopamine D1 receptors in prefrontal cortex. Nature (Lond). 1995;376(6541):572–5.
Kesner RP, Hunt ME, Williams JM, Long JM. Prefrontal cortex and working memory for spatial response, spatial location, and visual object information in the rat. Cereb Cortex. 1996;6(2):311–8.
Ragozzino ME, Kesner RP. The effects of muscarinic cholinergic receptor blockade in the rat anterior cingulate and prelimbic/infralimbic cortices on spatial working memory. Neurobiol Learn Mem. 1998;69(3):241–57.
Volk DW, Pierri JN, Fritschy JM, Auh S, Sampson AR, Lewis DA. Reciprocal alterations in pre- and postsynaptic inhibitory markers at chandelier cell inputs to pyramidal neurons in schizophrenia. Cereb Cortex. 2002;12(10):1063–70.
Harrison PJ, Owen MJ. Genes for schizophrenia? Recent findings and their pathophysiological implications. Lancet. 2003;361(9355):417–9.
Lewis DA, Hashimoto T, Volk DW. Cortical inhibitory neurons and schizophrenia. Nat Rev Neurosci. 2005;6(4):312–24.
Suzuki Y, Jodo E, Takeuchi S, Niwa S, Kayama Y. Acute administration of phencyclidine induces tonic activation of medial prefrontal cortex neurons in freely moving rats. Neuroscience. 2002;114(3):769–79.
Jackson ME, Homayoun H, Moghaddam B. NMDA receptor hypofunction produces concomitant firing rate potentiation and burst activity reduction in the prefrontal cortex. Proc Natl Acad Sci USA. 2004;101(22):8467–72.
Koch M. The neurobiology of startle. Prog Neurobiol. 1999;59(2):107–28.
Kamiyama H, Matsumoto M, Otani S, Kimura SI, Shimamura KI, Ishikawa S, Yanagawa Y, Togashi H. Mechanisms underlying ketamine-induced synaptic depression in rat hippocampus-medial prefrontal cortex pathway. Neuroscience. 2011;177:159–69.
Shikanai H, Yoshida T, Konno K, Yamasaki M, Izumi T, Ohmura Y, Watanabe M, Yoshioka M. Distinct neurochemical and functional properties of GAD67-containing 5-HT neurons in the rat dorsal raphe nucleus. J Neurosci. 2012;32(41):14415–26.
Shikanai H, Izumi T, Matsumoto M, Togashi H, Yamaguchi T, Yoshida T, Yoshioka M. Diazepam-induced increases of synaptic efficacy in the hippocampal-medial prefrontal cortex pathway are associated with its anxiolytic-like effect in rats. J Pharmacol Sci. 2010;114(3):341–6.
Swerdlow NR, Braff DL, Geyer MA. Cross-species studies of sensorimotor gating of the startle reflex. Ann N Y Acad Sci. 1999;877:202–16.
Swerdlow NR, Geyer MA, Braff DL. Neural circuit regulation of prepulse inhibition of startle in the rat: current knowledge and future challenges. Psychopharmacology (Berl). 2001;156(2-3):194–215.
Kumari V, Gray JA, Geyer MA, ffytche D, Soni W, Mitterschiffthaler MT, Vythelingum GN, Simmons A, Williams SC, Sharma T. Neural correlates of tactile prepulse inhibition: a functional MRI study in normal and schizophrenic subjects. Psychiatry Res. 2003;122(2):99–113.
Swerdlow NR, Bakshi V, Waikar M, Taaid N, Geyer MA. Seroquel, clozapine and chlorpromazine restore sensorimotor gating in ketamine-treated rats. Psychopharmacology (Berl). 1998;140(1):75–80.
Fejgin K, Safonov S, Pålsson E, Wass C, Engel JA, Svensson L, Klamer D. The atypical antipsychotic, aripiprazole, blocks phencyclidine-induced disruption of prepulse inhibition in mice. Psychopharmacology (Berl). 2007;191(2):377–85.
Cilia J, Hatcher P, Reavill C, Jones DN. Ketamine-induced prepulse inhibition deficits of an acoustic startle response in rats are not reversed by antipsychotics. J Psychopharmacol. 2007;21(3):302–11.
Ma J, Leung LS. The supramammillo-septal-hippocampal pathway mediates sensorimotor gating impairment and hyperlocomotion induced by MK-801 and ketamine in rats. Psychopharmacology (Berl). 2007;191(4):961–74.
Matsumoto M, Shikanai H, Togashi H, Izumi T, Kitta T, Hirata R, Yamaguchi T, Yoshioka M. Characterization of clozapine-induced changes in synaptic plasticity in the hippocampal-mPFC pathway of anesthetized rats. Brain Res. 2008;1195:50–5.
Lovick TA. Integrated activity of cardiovascular and pain regulatory systems: role in adaptive behavioural responses. Prog Neurobiol. 1993;40(5):631–44.
Bandler R, Shipley MT. Columnar organization in the midbrain periaqueductal gray: modules for emotional expression? Trends Neurosci. 1994;17(9):379–89.
Depaulis A, Keay KA, Bandler R. Longitudinal neuronal organization of defensive reactions in the midbrain periaqueductal gray region of the rat. Exp Brain Res. 1992;90(2):307–18.
Yaksh TL, Al-Rodhan NR, Jensen TS. Sites of action of opiates in production of analgesia. Prog Brain Res. 1988;77:371–94.
Curran T, Morgan JI. Fos: an immediate-early transcription factor in neurons. J Neurobiol. 1995;26(3):403–12.
Sánchez-Blázquez P, Rodríguez-Muñoz M, Berrocoso E, Garzón J. The plasticity of the association between mu-opioid receptor and glutamate ionotropic receptor N in opioid analgesic tolerance and neuropathic pain. Eur J Pharmacol. 2013.
Su YL, Huang J, Wang N, Wang JY, Luo F. The effects of morphine on basal neuronal activities in the lateral and medial pain pathways. Neurosci Lett. 2012;525(2):173–8.
Acknowledgments
This study was supported in part by a Grant-in-Aid for Scientific Research to H.T. (No. 24590117) from the Ministry of Education, Culture, Sports, Sciences and Technology of Japan and a Grant-in-Aid for the 2012–2013 Research Project of the Research Institute of Personalized Health Sciences, Health Sciences University of Hokkaido, Japan.
Conflict of interest
The authors declare no conflict of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
H. Shikanai, S. Hiraide, and H. Kamiyama contributed equally to the study.
About this article
Cite this article
Shikanai, H., Hiraide, S., Kamiyama, H. et al. Subanalgesic ketamine enhances morphine-induced antinociceptive activity without cortical dysfunction in rats. J Anesth 28, 390–398 (2014). https://doi.org/10.1007/s00540-013-1722-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-013-1722-5