Abstract
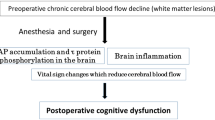
Cerebral dysfunction after cardiac surgery remains a devastating complication and is growing in importance with our aging populations. Neurological complications following cardiac surgery can be classified broadly as stroke, encephalopathy (including delirium), or postoperative cognitive dysfunction (POCD). These etiologies are caused primary by cerebral emboli, hypoperfusion, or inflammation that has largely been attributed to the use of cardiopulmonary bypass. Preventative operative strategies, such as off-pump coronary artery bypass grafting (CABG), can potentially reduce the incidence of postoperative neurological complications by avoiding manipulation of the ascending aorta. Although off-pump CABG is associated with reduced risk of stroke, there are no convincing differences in POCD between off-pump and on-pump CABG. Recently, the focus of postoperative neurological research has shifted from managing cardiopulmonary bypass to patient-related factors. Identifying changes in brains of aged individuals undergoing cardiac surgery may improve strategies for preventing cerebral dysfunction. Advanced age is associated with more undiagnosed cerebrovascular disease and is a major risk factor for stroke and POCD following cardiac surgery. Preoperative cerebrovascular evaluation and adaptation of surgical strategies will provide preventative approaches for cerebral dysfunction after CABG. This review focuses on recent findings of the relationship between perioperative stress and underlying fragility of the brain in cardiac surgical patients.
Similar content being viewed by others
References
Roach GW, Kanchuger M, Mangano CM, Newman M, Nussmeier N, Wolman R, Aggarwal A, Marschall K, Graham SH, Ley C. Adverse cerebral outcomes after coronary bypass surgery. Multicenter study of perioperative ischemia research group and the ischemia research and education foundation investigators. N Engl J Med. 1996;335:1857–63.
McKhann GM, Goldsborough MA, Borowicz LM Jr, Mellits ED, Brookmeyer R, Quaskey SA, Baumgartner WA, Cameron DE, Stuart RS, Gardner TJ. Predictors of stroke risk in coronary artery bypass patients. Ann Thorac Surg. 1997;63:516–21.
Stamou SC, Hill PC, Dangas G, Pfister AJ, Boyce SW, Dullum MK, Bafi AS, Corso PJ. Stroke after coronary artery bypass: incidence, predictors, and clinical outcome. Stroke. 2001;32:1508–13.
Hogue CW Jr, Palin CA, Arrowsmith JE. Cardiopulmonary bypass management and neurologic outcomes: an evidence-based appraisal of current practices. Anesth Analg. 2006;103:21–37.
Misfeld M, Brereton RJ, Sweetman EA, Doig GS. Neurologic complications after off-pump coronary artery bypass grafting with and without aortic manipulation: meta-analysis of 11,398 cases from 8 studies. J Thorac Cardiovasc Surg. 2011;142:e11–7.
Marasco SF, Sharwood LN, Abramson MJ. No improvement in neurocognitive outcomes after off-pump versus on-pump coronary revascularization: a meta-analysis. Eur J Cardiothorac Surg. 2008;33:961–70.
Selnes OA, Grega MA, Bailey MM, Pham LD, Zeger SL, Baumgartner WA, McKhann GM. Cognition 6 years after surgical or medical therapy for coronary artery disease. Ann Neurol. 2008;63:581–90.
Selnes OA, Gottesman RF, Grega MA, Baumgartner WA, Zeger SL, McKhann GM. Cognitive and neurologic outcomes after coronary-artery bypass surgery. N Engl J Med. 2012;366:250–7.
van Harten AE, Scheeren TW, Absalom AR. A review of postoperative cognitive dysfunction and neuroinflammation associated with cardiac surgery and anesthesia. Anaesthesia. 2012;67:280–93.
Avidan MS, Benzinger TL. Surgery and the plastic brain. Anesthesiology. 2012;116:510–2.
Resnick SM, Pham DL, Kraut MA, Zonderman AB, Davatzikos C. Longitudinal magnetic resonance imaging studies of older adults: a shrinking brain. J Neurosci. 2003;23:3295–301.
Peters R. Ageing and the brain. Postgrad Med. 2006;82:84–8.
Simen AA, Bordner KA, Martin MP, Moy LA, Barry LC. Cognitive dysfunction with aging and the role of inflammation. Ther Adv Chronic Dis. 2011;2:175–95.
Sparkman ML, Johnson RW. Neuroinflammation associated with aging sensitizes the brain to the effects of infection or stress. Neuroimmunomodulation. 2008;15:323–30.
Buchanan JB, Sparkman NL, Chen J, Johnson RW. Cognitive and neuroinflammatory consequences of mild repeated stress are exacerbated in aged mice. Psychoneuroendocrinology. 2008;33:755–65.
Terrando N, Rei Fidalgo A, Vizcaychipi M, Cibelli M, Ma D, Monaco C, Feldmann M, Maze M. The impact of IL-1 modulation on the development of lipopolysaccharide-induced cognitive dysfunction. Crit Care. 2010;14:R88.
Gao L, Taha R, Gauvin D, Othmen LB, Wang Y, Blaise G. Postoperative cognitive dysfunction after cardiac surgery. Chest. 2005;128:3664–70.
Wan Y, Xu J, Ma D, Zeng Y, Cibelli M, Maze M. Postoperative impairment of cognitive function in rats: a possible role for cytokine-mediated inflammation in the hippocampus. Anesthesiology. 2007;106:436–43.
del Zoppo GJ. Inflammation and the neurovascular unit in the setting of focal cerebral ischemia. Neuroscience. 2009;158:972–82.
Yang Y, Rosenberg GA. Blood–brain barrier breakdown in acute and chronic cerebrovascular disease. Stroke. 2011;42:3323–8.
Banks WA, Farr SA, Morley JE. Entry of blood-borne cytokines into the central nervous system: effects on cognitive processes. Neuroimmunomodulation. 2002–2003; 10:319−327.
Goto T, Baba T, Honma K, Shibata Y, Arai Y, Uozumi H, Okuda T. Magnetic resonance imaging findings and postoperative neurologic dysfunction in elderly patients undergoing coronary artery bypass grafting. Ann Thorac Surg. 2001;72:137–42.
Vermeer SE, Longstreth WT Jr, Koudstaal PJ. Silent brain infarcts: a systematic review. Lancet Neurol. 2007;6:611–9.
Tang JX, Eckenhoff MF, Echenhoff RG. Anesthetic modulation of neuroinflammation in Alzheimer’s disease. Curr Opin Anaesthesiol. 2011;24:389–94.
Xie Z, Culley DJ, Dong Y, Zhang G, Zhang B, Moir RD, Frosch MP, Crosby G, Tanzi RE. The common inhalation anesthetic isoflurane induces caspase activation and increases amyloid beta-protein level in vivo. Ann Neurol. 2008;6:618–27.
Bittner EA, Yue Y, Xie Z. Brief review: anesthetic neurotoxicity in the elderly, cognitive dysfunction and Alzheimer’s disease. Can J Anaesth. 2011;58:216–23.
Seitz DP, Shah PS, Herrmann N, Beyene J, Siddiqui N. Exposure to general anesthesia and risk of Alzheimer’s disease: a systemic review and meta-analysis. BMC Geriatr. 2011;11:83.
Avidan MS, Searleman AC, Storandt M, Barnett K, Vannucci A, Saager L, Xiong C, Grant EA, Kaiser D, Morris JC, Evers AS. Long-term cognitive decline in older subjects was not attributable to noncardiac surgery or major illness. Anesthesiology. 2009;111:964–70.
Selim M. Perioperative stroke. N Engl J Med. 2007;356:706–13.
Mérie C, Køber L, Olsen PS, Andersson C, Jensen JS, Torp-Pedersen C. Risk of stroke after coronary artery bypass grafting: effect of age and comorbidities. Stroke. 2012;43:38–43.
Tarakji KG, Sabik JF 3rd, Bhudia SK, Batizy LH, Blackstone EH. Temporal onset, risk factors, and outcomes associated with stroke after coronary artery bypass grafting. JAMA. 2011;305:381–90.
Nishiyama K, Horiguchi M, Shizuta S, Doi T, Ehara N, Tanuguchi R, Haruna Y, Nakagawa Y, Fukukawa Y, Fukushima M, Kita T, Kimura T. Temporal pattern of strokes after on-pump and off-pump coronary artery bypass graft surgery. Ann Thorac Surg. 2009;87:1839–44.
Likosky DS, Marrin CA, Caplan LR, Baribeau YR, Morton JR, Weintraub RM, Hartman GS, Hernandez F Jr, Braff SP, Charlesworth DC, Malenka DJ, Ross CS, O’Connor GT, Northern New England Cardiovascular Disease Study Group. Determination of etiologic mechanisms of strokes secondary to coronary artery bypass graft surgery. Stroke. 2003;34:2830–4.
Liddicoat JR, Redmond JM, Vassileva CM, Baumgartner WA, Cameron DE. Hypothermic circulatory arrest in octogenarians: risk of stroke and mortality. Ann Thorac Surg. 2000;69:1048–51.
Dávila-Román VG, Barzilai B, Wareing TH, Murphy SF, Schechtman KB, Kouchoukos NT. Atherosclerosis of the ascending aorta. Prevalence and role as an independent predictor of cerebrovascular events in cardiac patients. Stroke. 1994;25:2010–6.
Goto T, Baba T, Matsuyama K, Honma K, Ura M, Koshiji T. Aortic atherosclerosis and postoperative neurological dysfunction in elderly coronary surgical patients. Ann Thorac Surg. 2003;75:1912–8.
Ura M, Sakata R, Nakayama Y, Goto T. Ultrasonographic demonstration of manipulation-related aortic injuries after cardiac surgery. J Am Coll Cardiol. 2000;35:1303–10.
Kapetanakis EI, Stamou SC, Dullum MK, Hill PC, Haile E, Boyce SW, Bafi AS, Petro KR, Corso PJ. The impact of aortic manipulation on neurologic outcomes after coronary artery bypass surgery: a risk-adjusted study. Ann Thorac Surg. 2004;78:1564–71.
Rosenberger P, Shernan SK, Löffler M, Shekar PS, Fox JA, Tuli JK, Nowak M, Eltschig HK. The influence of epiaortic ultrasonography on intraoperative surgical management in 6051 cardiac surgical patients. Ann Thorac Surg. 2008;85:548–53.
Afilalo J, Rasti M, Ohayon SM, Shimony A, Eisenberg MJ. Off-pump vs. on-pump coronary artery bypass surgery: an updates meta-analysis and meta-regression of randomized trials. Eur Heart J. 2012;33:1257–67.
Li Z, Denton T, Yeo KK, Parker JP, White R, Young JN, Amsterdam EA. Off-pump bypass surgery and postoperative stroke: California coronary bypass outcomes reporting program. Ann Thorac Surg. 2010;90:753–9.
Caplan LR, Hennerici M. Impaired clearance of emboli (washout) is an important link between hypoperfusion, embolism, and ischemic stroke. Arch Neurol. 1998;11:1475–82.
Gottesman RF, Sherman PM, Grega MA, Yousem DM, Borowicz LM Jr, Selnes OA, Baumgartner WA, McKhann GM. Watershed strokes after cardiac surgery: diagnosis, etiology, and outcome. Stroke. 2006;37:2306–11.
Gold JP, Charlson ME, Williams-Russo P, Szatrowski TP, Peterson JC, Pirraglia PA, Hartman GS, Yao FS, Hollenberg JP, Barbut D. Improvement of outcomes after coronary artery bypass. A randomized trial comparing intraoperative high versus low mean arterial pressure. J Thorac Cardiovasc Surg. 1995;110:1302–11.
Naylor AR, Mehta Z, Rothwell PM, Bell PR. Carotid artery disease and stroke during coronary artery bypass: a critical review of the literature. Eur J Vasc Endovasc Surg. 2002;23:283–94.
Li Y, Walicki D, Mathiesen C, Jenny D, Li Q, Isayev Y, Reed JF 3rd, Castaldo JE. Strokes after cardiac surgery and relationship to carotid stenosis. Arch Neurol. 2009;66:1091–6.
Naylor AR. Does the risk of post-CABG stroke merit staged or synchronous reconstruction in patients with symptomatic or asymptomatic carotid disease? J Cardiovasc Surg (Torino). 2009;50:71–81.
Guzman LA, Costa MA, Angiolillo DJ, Zenni M, Wludyka P, Silliman S, Bass TA. A systematic review of outcomes in patients with staged carotid artery stenting and coronary artery bypass graft surgery. Stroke. 2008;39:361–5.
van Dijk D, Keizer AM, Diephuis JC, Durand C, Vos LJ, Hijman R. Neurocognitive dysfunction after coronary artery bypass surgery: a systemic review. J Thorac Cardiovasc Surg. 2000;120:632–9.
Newman MF, Kirchner JL, Phillips-Bute B, Gaver V, Grocott H, Jones RH, Mark DB, Reves JG, Blumenthal JA. Neurological Outcome Research Group and the Cardiothoracic Anesthesiology Research Endeavors Investigators. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med. 2001;344:395–402.
Evered L, Scott DA, Silbert B, Maruff P. Postoperative cognitive dysfunction is independent of type of surgery and anesthetic. Anesth Analg. 2011;112:1179–85.
Rudolph JL, Schreiber KA, Culley DJ, McGlinchey RE, Crosby G, Levisky S, Marcantonio ER. Measurement of post-operative cognitive dysfunction after cardiac surgery: a systemic review. Acta Anaesthesiol Scand. 2010;54:663–77.
Ho PM, Arciniegas DB, Grigsby J, McCarthy M Jr, McDonald GO, Moritz TE, Shroyer AL, Sethi GK, Henderson WG, London MJ, VillaNueva CB, Grover FL, Hammermeister KE. Predictors of cognitive decline following coronary artery bypass graft surgery. Ann Thorac Surg. 2004;77:597–603.
Grigore AM, Grocott HP, Mathew JP, Phillips-Bute B, Stanley TO, Butler A, Landolfo KP, Reves JG, Blumenthal JA, Newman MF, Neurologic Outcome Research Group of the Duke Heart Center. The rewarming rate and increased peak temperature alter neurocognitive outcome after cardiac surgery. Anesth Analg. 2002;94:4–10.
Evered LA, Slibert BS, Scott DA. Postoperative cognitive dysfunction and aortic atheroma. Ann Thorac Surg. 2010;89:1091–7.
Fontes MT, Swift RC, Phillips-Bute B, Podgoreanu MV, Stafford-Smith M, Newman MF, Mathew JP, Neurologic Outcome Research Group of the Duke Heart Center. Predictors of cognitive recovery after cardiac surgery. Anesth Analg. 2013;116:435–42.
Erickson KI, Kramer AF. Aerobic exercise effects on cognitive and neural plasticity in older adults. Br J Sports Med. 2009;43:22–4.
Moody DM, Bell MA, Challa VR, Johnston WE, Prough DS. Brain microemboli during cardiac surgery or aortography. Ann Neurol. 1990;28:477–86.
Brown WR, Thore CR. Review: cerebral microvascular pathology in ageing and neurodegeneration. Neuropathol Appl Neurobiol. 2011;37:56–74.
Djaiani G, Fedorko L, Borger MA, Green R, Carroll J, Marcon M, Karski J. Continuous-flow cell saver reduces cognitive decline in elderly patients after coronary bypass surgery. Circulation. 2007;116:1888–95.
Rodriguez RA, Rubens FD, Wozny D, Nathan HJ. Cerebral emboli detected by transcranial Doppler during cardiopulmonary bypass are not correlated with postoperative cognitive deficits. Stroke. 2010;41:2229–35.
Liu YH, Wang DX, Li LH, Wu XM, Shan GJ, Su Y, Li J, Yu QJ, Shi CX, Huang YN, Sun W. The effects of cardiopulmonary bypass on the number of cerebral microemboli and the incidence of cognitive dysfunction after coronary artery bypass graft surgery. Anesth Analg. 2009;109:1013–22.
Bendszus M, Reents W, Franke D, Müllges W, Babin-Ebell J, Koltzenburg M, Warmuth-Metz M, Solymosi L. Brain damage after coronary artery bypass grafting. Arch Neurol. 2002;59:1090–5.
Knipp SC, Matatko N, Wilhelm H, Schlamann M, Thielmann M, Lösch C, Diener HC, Jakob H. Cognitive outcomes three years after coronary artery bypass surgery: relation to diffusion-weighted magnetic resonance imaging. Ann Thorac Surg. 2008;85:872–9.
Restrepo L, Wityk RJ, Grega MA, Borowicz L Jr, Barker PB, Jacobs MA, Beauchamp NJ, Hillis AE, McKhann GM. Diffusion- and perfusion-weighted magnetic resonance imaging of the brain before and after coronary artery bypass grafting surgery. Stroke. 2002;33:2909–15.
Cook DJ, Huston J 3rd, Trenerry MR, Brown RD Jr, Zehr KJ, Sundt TM 3rd. Postcardiac surgical cognitive impairment in the aged using diffusion-weighted magnetic resonance imaging. Ann Thorac Surg. 2007;83:1389–95.
Sun X, Lindsay J, Monsein LH, Hill PC, Corso PJ. Silent brain injury after cardiac surgery: a review: cognitive dysfunction and magnetic resonance imaging diffusion-weighted imaging findings. J Am Coll Cardiol. 2012;60:791–7.
Maekawa K, Goto T, Baba T, Yoshitake A, Morishita S, Koshiji T. Abnormalities in the brain before elective cardiac surgery detected by diffusion-weighted magnetic resonance imaging. Ann Thorac Surg. 2008;86:1563–9.
Maekawa K, Goto T, Baba T, Yoshitake A, Katahira K, Yamamoto T. Impaired cognition preceding cardiac surgery is related to cerebral ischemic lesions. J Anesth. 2011;25:330–6.
Glass CK, Saijo K, Winner B, Marchetto MC, Gage FH. Mechanisms underlying inflammation in neurodegeneration. Cell. 2010;140:918–34.
Bendlin BB, Newman LM, Ries ML, Puglielli L, Carlsson CM, Sager MA, Rowley HA, Gallagher CL, Willette AA, Alexander AL, Asthana S, Johnson SC. NSAIDs may protect against age-related brain atrophy. Front Aging Neurosci 2010;2:35.
Gong M, Chen G, Zhang XM, Xu LH, Wang HM, Yan M. Parecoxib mitigates spatial memory impairment induced by sevoflurane anesthesia in aged rats. Acta Anaesthesiol Scand. 2012;56:601–7.
Hudetz JA, Gandhi SD, Iqbal Z, Patterson KM, Pagel PS. Elevated postoperative inflammatory biomarkers are associated with short- and medium-term cognitive dysfunction after coronary artery surgery. J Anesth. 2011;25:1–9.
Sanders RD, Avidan MS. Postoperative cognitive trajectories in adults. The role of inflammatory processes. Anesthesiology. 2013;118:484–6.
Kellermann K, Jungwirth B. Avoiding stroke during cardiac surgery. Semin Cardiothorac Vasc Anesth. 2010;14:95–101.
Nakamura M, Okamoto F, Nakanishi K, Maruyama R, Yamada A, Ushikoshi S, Terasaka S, Kuroda S, Sakai K, Higami T. Does intensive management of cerebral hemodynamics and atheromatous aorta reduce stroke after coronary artery surgery? Ann Thorac Surg. 2008;85:513–9.
Ito A, Goto T, Maekawa K, Baba T, Mishima Y, Ushijima K. Postoperative neurological complications and risk factors for preexisting silent brain infarction in elderly patients undergoing coronary artery bypass grafting. J Anesth. 2012;26:405–11.
Silbert BS, Scott DA, Evered LA, Lewis MS, Maruff PT. Preexisting cognitive impairment in patients scheduled for elective coronary artery bypass graft surgery. Anesth Analg. 2007;104:1023–8.
Stroobant N, Vingehoers G. Pre-existing cognitive impairment in candidates for cardiac surgery: an overview. Heart. 2009;95:1820–5.
Crosby G, Culley DJ, Hyman BT. Preoperative cognitive assessment of the elderly surgical patients: a call for action. Anesthesiology. 2011;114:1265–8.
D’Agostino RS, Svensson LG, Neumann DJ, Balkhy HH, Willamson WA, Shahian DM. Screening carotid ultrasonography and risk factors for stroke in coronary artery surgery patients. Ann Thorac Surg. 1996;62:1714–23.
Murkin JM, Adams SJ, Novick RJ, Quantz M, Bainbridge D, Iglesias I, Cleland A, Schaefer B, Irwin B, Fox S. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg. 2007;104:51–8.
Zheng F, Sheinberg R, Yee MS, Ono M, Zheng Y, Hogue CW. Cerebral near-infrared spectroscopy monitoring and neurologic outcomes in adult cardiac surgery patients: a systematic review. Anesth Analg. 2013;116:663–76.
Gold JP, Torres KE, Maldarelli W, Zhuravlev I, Condit D, Wasnick J. Improving outcomes in coronary surgery: the impact of echo-directed aortic cannulation and perioperative hemodynamic management in 500 patients. Ann Thorac Surg. 2004;78:1579–85.
Puskas F, Grocott HP, White WD, Mathew JP, Newman MF, Bar-Yosef S. Intraoperative hyperglycemia and cognitive decline after CABG. Ann Thorac Surg. 2007;84:1467–73.
Murkin JM, Martzke JS, Buchan AM, Bentley C, Wong CJ. A randomized study of the influence of perfusion technique and pH management strategy in 316 patients undergoing coronary artery bypass surgery. II. Neurologic and cognitive outcomes. J Thorac Cardiovasc Surg. 1995;110:349–62.
Edaravone Acute Infarction Study Group. Effect of a novel free radical scavenger, edaravone (MCI-186), on acute brain infarction. Randomized, placebo-controlled, double-blind study at multicenters. Cerebrovasc Dis. 2003;15:222–9.
Cao L, Young N, Liu H, Silvestry S, Sun W, Zhao N, Diehl J, Sun J. Preoperative aspirin use and outcomes in cardiac surgery patients. Ann Surg. 2012;255:399–404.
Bouchard D, Carrier M, Demers P, Cartier R, Pellerin M, Perrault LP, Lambert J. Statin in combination with β-blocker therapy reduces postoperative stroke after coronary artery bypass graft surgery. Ann Thorac Surg. 2011;91:654–9.
Ji F, Li Z, Nguyen H, Young N, Shi P, Fleming N, Liu H. Perioperative dexmedetomidine improves outcomes of cardiac surgery. Circulation. 2013;127:1576–84.
Acknowledgments
The authors thank Dr. Jon Moon for his editorial assistance.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Goto, T., Maekawa, K. Cerebral dysfunction after coronary artery bypass surgery. J Anesth 28, 242–248 (2014). https://doi.org/10.1007/s00540-013-1699-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-013-1699-0