Abstract
Purpose
A decrease in blood pressure is sometimes observed when a postsurgical patient is transferred to another bed after recovering from anesthesia. However, the mechanism behind this hypotension has not been completely elucidated. The purpose of this study was to investigate and compare changes in hemodynamic properties for possible causes of hypotension before and after transfer to another bed of postsurgical patients receiving general anesthesia, combined epidural and general anesthesia, or combined spinal and general anesthesia.
Methods
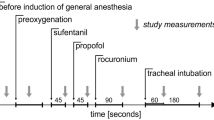
We studied 69 patients undergoing elective surgery who were randomized to receive anesthesia by one of the three methods. After surgery, the tracheal tube was removed, and each patient was transferred to another bed. Hemodynamic data recorded immediately before and after transfer of the patient to another bed were compared.
Results
After transfer of patients receiving general anesthesia or combined epidural and general anesthesia, systolic arterial pressure (SAP), diastolic arterial pressure (DAP), and cardiac output (CO) decreased; heart rate (HR) and systemic vascular resistance (SVR) did not change. However, after transfer of patients receiving combined spinal and general anesthesia, SAP, DAP, HR, and CO decreased, but SVR did not change.
Conclusion
The decrease in blood pressure observed after transfer of a postsurgical patient to another bed after general, combined epidural and general, and combined spinal and general anesthesia was associated with a decrease in CO and no change in SVR, but HR decreased after combined spinal and general anesthesia, whereas it was unchanged after general and combined epidural and general anesthesia. The decrease in blood pressure is assumed to be caused by a decrease in venous return, and several reflexes might participate in this decrease of blood pressure, especially after combined spinal and general anesthesia.



Similar content being viewed by others
References
Verdeyen J, Ory JP, Wyckmans W, Vandermeersch E, Jamaer L, Van Assche A. Prevention of postoperative hypotension following spinal anesthesia for TURP: a double-blind randomized controlled trial comparing ephedrine with placebo. Acta Anaesthesiol Belg. 2008;59:73–8.
Bandi E, Weeks S, Carli F. Spinal block levels and cardiovascular changes during post-Cesarean transport. Can J Anaesth. 1999;46:736–40.
Wajima Z, Shitara T, Ishikawa G, Inoue T, Ogawa R. Analgesia after upper abdominal surgery with extradural buprenorphine with lidocaine. Can J Anaesth. 1998;45:28–33.
Wajima Z, Shitara T, Ishikawa G, Kaneko K, Inoue T, Ogawa R. Analgesia after upper abdominal surgery using extradural administration of a fixed dose of buprenorphine in combination with lignocaine given at two infusion rates: a comparative study. Acta Anaesthesiol Scand. 1997;41:1061–5.
Biais M, Vidil L, Sarrabay P, Cottenceau V, Revel P, Sztark F. Changes in stroke volume induced by passive leg raising in spontaneously breathing patients: comparison between echocardiography and Vigileo/FloTrac device. Crit Care. 2009;13:R195.
Wajima Z, Shiga T, Imanaga K, Inoue T. Assessment of the effect of rapid crystalloid infusion on stroke volume variation and pleth variability index after a preoperative fast. J Clin Monit Comput. 2010;24:385–9.
de Leeuw MA, Slagt C, Hoeksema M, Zuurmond WW, Perez RS. Hemodynamic changes during a combined psoas compartment-sciatic nerve block for elective orthopedic surgery. Anesth Analg. 2011;112:719–24.
Wajima Z, Shiga T, Imanaga K, Inoue T. Do induced hypertension and hypotension affect stroke volume variation in man? J Clin Anesth. 2012;24:207–11.
Cannesson M, Musard H, Desebbe O, Boucau C, Simon R, Hénaine R, Lehot JJ. The ability of stroke volume variations obtained with Vigileo/FloTrac system to monitor fluid responsiveness in mechanically ventilated patients. Anesth Analg. 2009;108:513–7.
Biais M, Nouette-Gaulain K, Cottenceau V, Revel P, Sztark F. Uncalibrated pulse contour-derived stroke volume variation predicts fluid responsiveness in mechanically ventilated patients undergoing liver transplantation. Br J Anaesth. 2008;101:761–8.
Cassoria L, Lee J-W. Patient positioning and anesthesia. In: Miller RD, editor. Miller’s anesthesia, vol 1. Philadelphia, PA: Churchill Livingstone Elsevier; 2010. p. 1163.
Curatolo M, Scaramozzino P, Venuti FS, Orlando A, Zbinden AM. Factors associated with hypotension and bradycardia after epidural blockade. Anesth Analg. 1996;83:1033–40.
Lesser JB, Sanborn KV, Valskys R, Kuroda M. Severe bradycardia during spinal and epidural anesthesia recorded by an anesthesia information management system. Anesthesiology. 2003;99:859–66.
Urmey WF. Case studies of regional anesthesia. In: Finucane BT, editor. Complications of regional anesthesia. 2nd ed. New York: Springer Science + Business Media, LLC.; 2007. p. 417–20.
Scavone BM, Ratliff J, Wong CA. Physiologic effects of neuraxial anesthesia. In: Wong CA, editor. Spinal and epidural anesthesia. Columbus: McGraw–Hill; 2007. p. 115–6.
Tarkkila P. Complications associated with spinal anesthesia. In: Finucane BT, editor. Complications of regional anesthesia. 2nd ed. New York: Springer Science + Business Media, LLC.; 2007. p. 151.
Mackey DC, Carpenter RL, Thompson GE, Brown DL, Bodily MN. Bradycardia and asystole during spinal anesthesia: a report of three cases without morbidity. Anesthesiology. 1989;70:866–8.
Campagna JA, Carter C. Clinical relevance of the Bezold–Jarisch reflex. Anesthesiology. 2003;98:1250–60.
Ponhold H, Vicenzi MN. Incidence of bradycardia during recovery from spinal anaesthesia: influence of patient position. Br J Anaesth. 1998;81:723–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Part of this work was presented at the American Society of Anesthesiologists 2010 Annual Meeting (San Diego, CA, USA).
About this article
Cite this article
Wajima, Z., Shiga, T., Imanaga, K. et al. Vigilance of hemodynamic changes immediately after transferring patients is crucial. J Anesth 27, 521–527 (2013). https://doi.org/10.1007/s00540-013-1568-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-013-1568-x