Abstract
Purpose
Endotracheal tube intra-cuff pressure should be maintained between 20 and 30 cmH2O to prevent damage to the tracheal wall. However, cuff pressure is rarely measured, and clinicians estimate cuff pressure poorly. The goal of the present study was to predict the cuff volume that produces optimal cuff pressure either from tracheal diameter or from patient height and age.
Methods
In the development phase, initial cuff pressure and cuff volume were measured in 240 patients. Optimal cuff volume, defined as the volume halfway between the volumes required to produce cuff pressures of 20 and 30 cmH2O, was determined in each patient. Then, regression equations relating optimal cuff volume to tracheal diameter on chest X-ray, and between optimal cuff volume and a combination of height and age, were calculated. The primary outcome was the proportion of patients in a validation set (n = 104) who achieved a cuff pressure of 20–30 cmH2O when cuff volume was selected by each regression formula.
Results
Only 28 % of the cuffs were optimally inflated using clinical criteria during the development phase. There was good correlation between optimal cuff volume and tracheal diameter and moderate correlation between optimal cuff volume and both height and age. Predicted cuff volume was more likely to provide optimal cuff pressure when based on tracheal diameter (65 % of patients) than when based on both height and age (45 % of patients).
Conclusions
Optimal cuff volume was better estimated from tracheal diameter and patient height and age than from the manual palpation method.
Similar content being viewed by others
Introduction
Endotracheal tubes are carefully chosen in pediatric patients according to characteristics such as age and height [1, 2]. Choosing the correct endotracheal tube size is less important in adults than in children because the trachea is sealed around a small tube through adjustment of intra-cuff volume. However, excessive intra-cuff pressure can lead to complications such as tracheal mucosal edema [3] and fistula [4], and inadequate cuff pressure can lead to insufficient ventilation, poor reliability of end-tidal gas monitoring, leakage of anesthetic gases into the operating room environment, and an increased risk of aspiration [5–8]. Thus, careful attention should be paid to maintain optimal cuff pressure. However, a report showed that 75 % of intensive care units never check cuff pressure [9].
A sore throat is a common side effect of general anesthesia, reported to affect between 14 and 50 % of patients after tracheal intubation [10]. Excessive cuff pressure is a prime cause of the sore throat resulting from general anesthesia [11]. Furthermore, previous studies have shown that when cuff pressure is adjusted by manual palpation, less than 30 % of patients have cuff pressures within the optimal range of 20–30 cmH2O [12, 13].
Chest X-rays are used routinely to verify endotracheal intubation in Japan and in some other countries. Tracheal diameter, determined radiographically, has been used to predict proper endotracheal tube size [14]. Similarly, it is clinically apparent that tracheal diameter gradually increases in proportion to both patient height and age; proper endotracheal tube size should also be predictable from patient height and age [15, 16]. The goal of the present study was to predict optimal cuff volume from tracheal diameter and patient height and age.
Materials and methods
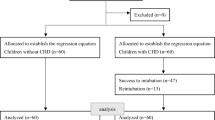
The Review Board for Human Experiments of the Kyoto Prefectural University of Medicine approved this prospective study, and written informed consent was obtained from the patients or their relatives. A total of 344 patients (aged 12–91 years) who were undergoing elective surgery with general anesthesia under tracheal intubation were enrolled. Patients with conditions known or suspected to cause laryngeal and tracheal pathology, emergency intubation, anticipated difficult intubation, as well as pregnant women and those at high risk for aspiration, were excluded.
General anesthesia was induced with intravenous propofol combined with either vecuronium or rocuronium. Patients were intubated with endotracheal tubes with high-volume and low-pressure cuffs (Mallinckrodt Intermediate Tracheal Tubes; Covidien, Tokyo, Japan). The internal diameter of the tubes chosen was 8.0 or 8.5 mm for men and 7.0 or 7.5 mm for women, per routine practice in our hospital and as reported previously [13]. Anesthesia was maintained with volatile anesthetics in a combination of air and oxygen; nitrous oxide was not used. Endotracheal tube cuff pressures between 20 and 30 cmH2O were considered optimal [7, 13, 17–19].
Tracheal diameter at the sternoclavicular junction level on chest X-ray taken preoperatively was recorded with morphometric characteristics including age, gender, height, and weight. All measurements were performed with patients in the supine position with the head in a neutral position. The distance between the X-ray tube and the patient was standardized for all X-rays evaluated in the present study.
Development phase
For 240 patients (120 men and 120 women), data were collected from four age-based groups (12–29, 30–49, 50–69, and ≥70 years; Table 1). An anesthesiologist who was blinded to the experimental design inserted the endotracheal tube and inflated the cuff. The cuff was inflated just enough to stop an audible air leak at a static airway pressure of 20 cmH2O.
Thereafter, investigators blinded to patient morphometric characteristics measured cuff pressure 60 min after induction of anesthesia using a manometer (Mallinckrodt Medical, Athlone, Ireland) connected to the pilot balloon. Initial cuff volume was measured by completely deflating the cuff and measuring the volume of removed air. The cuff was then progressively inflated by injecting air in 0.1-ml increments until a cuff pressure of 10, 20, 30, and 40 cmH2O was achieved. Cuff volumes were recorded at these cuff pressures. The entire process required about 1 min. We measured intra-cuff pressure by using a three-way stopcock to avoid the leakage of the air in the cuff and the effect of compressed air in the syringe. Optimal cuff volume, the volume halfway between cuff volumes at 20 and 30 cmH2O cuff pressure, was determined for each patient. Two regression equations were then calculated: (1) between optimal intra-cuff volume and tracheal diameter and (2) between optimal intra-cuff volume and both patient height and age.
Tracheal diameter was electronically measured at the sternoclavicular junction on chest X-ray as it is an objective landmark and because the endotracheal tube cuff is located near this level. The effect of image magnification was thus adjusted automatically. The tracheal walls tend to be symmetrical at this level, and the diameter is usually consistent from the thoracic inlet to the carina [20].
Validation phase
For the validation phase, another 104 patients (52 men and 52 women) were categorized into the same four age-based subgroups used in the development phase. The cuff was inflated with the optimal intra-cuff volume based on the regression equation created from tracheal diameter and created from the combination of height and age constructed in the development phase. Thereafter, the proportion of patients in whom cuff pressure was optimal (i.e., between 20 and 30 cmH2O) at 60 min after cuff inflation was calculated.
Statistical analysis
Data were analyzed using GraphPad InStat software, version 3.06.32 (GraphPad Software, La Jolla, CA, USA). Chi-square tests were used to compare two groups of patients. Regression and correlation analyses were performed with the method of least-square fitting. Data are reported as mean ± SD unless otherwise indicated. Statistical significance was defined as P < 0.05.
Results
Morphometric and demographic characteristics of the patients were similar in both the development and validation phases (Table 1). Average cuff pressure in the development phase was 21 ± 14 cmH2O, but only 28 % of the patients fell within the optimal range of cuff pressure (20–30 cmH2O). Cuff pressure exceeded 30 cmH2O in 17 % of patients and was less than 20 cmH2O in 55 % of patients.
Using data from the development phase, the regression equation was first constructed between tracheal diameter in millimeters and optimal cuff volume in milliliters (defined as the volume halfway between those necessary to produce a cuff pressure of 20 and 30 cmH2O): optimal cuff volume = 0.71 (tracheal diameter) − 8.25, R 2 = 0.83 (Fig. 1).
There was a poor correlation between tracheal diameter in millimeters and patient height in centimeters: tracheal diameter = 0.10 height + 0.73, adjusted R 2 = 0.19. There was similarly a poor relationship between tracheal diameter in millimeters and patient age in years: tracheal diameter = 0.04 age + 15, adjusted R 2 = 0.16. However, the correlation was improved by multiple regression between tracheal diameter and both height and age: tracheal diameter = 0.06 age + 0.14 height − 8.8, adjusted R 2 = 0.50. Thus, a multiple regression equation was calculated between the optimal cuff volume in milliliters and patient height in centimeters and age in years: optimal cuff volume = 0.11 height + 0.042 age − 15.6, adjusted R 2 = 0.44 (Fig. 2).
In the validation phase, cuff pressure with cuff volume inflation estimated based on tracheal diameter averaged 22 ± 7 cmH2O; 65 % of patients obtained optimal cuff pressure with this method (P < 0.001 compared with that in the development phase (28 %), and P < 0.001 compared with that in the validation phase predicted from the combination of height and age) (45 %, detailed below). Cuff pressure exceeded 30 cmH2O in 8 % of patients and was less than 20 cmH2O in 27 % of patients. Cuff pressure with cuff volume inflation estimated based on patient height and age averaged 22 ± 7 cmH2O; 45 % of patients obtained optimal cuff pressure with this method (P < 0.001 compared with the fraction in the development phase), and cuff pressure exceeded 30 cmH2O in 25 % of patients and was less than 20 cmH2O in 30 % of patients.
Discussion
Excessive cuff pressure can result in tracheal mucosal erosion and postoperative sore throat and hoarseness [11, 21]. Optimal cuff pressure has therefore been defined in previous studies and various guidelines [7, 13, 17–19]. Seegobin and van Hasselt [19], for example, confirmed that excessive cuff pressure contributes to tracheal damage and concluded that cuff pressure should not exceed 30 cmH2O. Inadequate cuff pressure is also dangerous and contributes to ventilator-associated pneumonia [18]. The American Thoracic Society guidelines thus include the recommendation that cuff pressure should be kept at ≥20 cmH2O [8]. Optimal cuff pressure was therefore defined in the present study as being within the range of 20–30 cmH2O.
There were no significant differences in regression coefficient (tracheal diameter, height, and age) between men and women. Using a single regression equation for predicting size is thus clinically practical. Selected endotracheal tube size was selected as internal diameter (ID) 7.0 or 7.5 for females and ID 8.0 or 8.5 mm for males in a previous report [13].
Previous studies have reported that cuff pressure rarely falls within the optimal range of 20–30 cmH2O when manual palpation is used [12, 13]. For example, Sengupta et al. [13] reported that only 27 % of patients had optimal cuff pressure without the use of manometry, a rate similar to that in the present development phase. The primary finding of the present study is that the proportion of patients achieving optimal cuff pressure was improved by using regression equations estimating appropriate inflation volume from tracheal diameter or height and age.
Of the present two approaches, cuff inflation volume was better estimated from tracheal diameter than from height and age (37 vs. 17 % absolute improvement). When tracheal diameter is available from a chest radiograph, inserting the value into the simple equation (optimal cuff volume = 0.71 tracheal diameter − 8.25) was found to be the best approach in the present study. When tracheal diameter is not available, the height and age equation is still considerably better than manual palpation alone.
Both formulas in the present study estimated appropriate cuff volume far better than manual palpation of the pilot balloon. The present formula based on tracheal diameter, which was considerably better than the formula based on height and age, correctly predicted initial cuff volume in only 65 % of patients. In other words, the formula failed in a full third of patients.
The present results are in contrast to those of Valentino et al., who reported that chest radiography is a poor screening tool for unsafe intra-cuff pressure [22]. They obtained tracheal diameter after inflating the cuff, whereas in the present study tracheal diameter was measured from a preoperative chest X-ray. Expansion of the trachea by the inflated cuff might well explain these discrepant conclusions.
The proportion of patients achieving optimal cuff pressure by the tracheal diameter measurement method might have been limited to 65 % for various reasons. First, the endotracheal tube cuff might not have been located at the level of the sternoclavicular junction. Second, the elasticity of the trachea varies among individuals. The trachea has a longitudinal membranous portion posteriorly, and it cannot be predicted how much the trachea actually expands. Third, the tracheal cross section was estimated from the chest X-ray, but this value can suffer from perspective distortion. In the present study, the distance between the X-ray tube and the patient was standardized for all posterior to anterior X-rays evaluated.
Many previous studies have documented the relationship between patient characteristics and tracheal diameter. These studies have found a good correlation between tracheal diameter and patient height in a pediatric population [20] and a poor correlation between tracheal diameter and patient height or age in an adult population [16]. In the present study, multiple regression analysis revealed a moderate correlation between tracheal diameter and height and age.
Although nitrous oxide is still used, the gas is being used in progressively fewer cases [23]. Nitrous oxide was avoided in the present study because of the well-known tendency of nitrogen diffusion to increase cuff volume and pressure [11]. The present results would be valid for initial cuff inflation even with nitrous oxide. In patients given nitrous oxide, it is necessary to continually monitor and adjust cuff pressure to prevent increases to potentially dangerous levels.
A limitation of the present analysis is that cuff volume was assumed to remain constant throughout surgery, and that the pressure–volume relationship was also assumed to remain constant. Cuff pressure does not change over time when the cuff is filled with saline, even during nitrous oxide general anesthesia [11]. Cuff pressure in air-filled cuffs is not thought to change over time when nitrous oxide is not used, but the time-dependence of cuff pressure has not yet been systematically evaluated. Cuff pressure was measured 1 h after induction of anesthesia in this study, as has been previously reported [13]. In the present study, only one brand of endotracheal tube was examined (Mallinckrodt Intermediate Tracheal tubes); the present results might therefore not apply to other brands of endotracheal tubes. Finally, airway complications such as post-extubation stridor or extubation failure caused by airway problems has not been evaluated in this study. Whether the 20–30 cmH2O of “optimal” pressure estimated from studies with long-term intubation could apply intraoperatively remained unresolved.
In summary, only 28 % of the cuffs obtained between 20 and 30 cmH2O of pressure with the manual palpation method. Optimal cuff volume was better estimated from tracheal diameter determined by chest radiograph or from patient height and age than from the manual palpation method.
References
Cole F. Pediatric formulas for the anesthesiologist. AMA J Dis Child. 1957;94(6):672–3.
Luten RC, Wears RL, Broselow J, Zaritsky A, Barnett TM, Lee T, Bailey A, Vally R, Brown R, Rosenthal B. Length-based endotracheal tube and emergency equipment in pediatrics. Ann Emerg Med. 1992;21(8):900–4.
Tu HN, Saidi N, Leiutaud T, Bensaid S, Menival V, Duvaldestin P. Nitrous oxide increases endotracheal cuff pressure and the incidence of tracheal lesions in anesthetized patients. Anesth Analg. 1999;89(1):187–90.
Hameed AA, Mohamed H, Al-Mansoori M. Acquired tracheoesophageal fistula due to high intracuff pressure. Ann Thorac Med. 2008;3(1):23–5.
Svenson JE, Lindsay MB, O’Connor JE. Endotracheal intracuff pressures in the ED and prehospital setting: is there a problem? Am J Emerg Med. 2007;25(1):53–6.
Stewart SL, Secrest JA, Norwood BR, Zachary R. A comparison of endotracheal tube cuff pressures using estimation techniques and direct intracuff measurement. AANA J. 2003;71(6):443–7.
American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416.
Safdar N, Dezfulian C, Collard HR, Saint S. Clinical and economic consequences of ventilator-associated pneumonia: a systematic review. Crit Care Med. 2005;33(10):2184–93.
Vyas D, Inweregbu K, Pittard A. Measurement of tracheal tube cuff pressure in critical care. Anaesthesia. 2002;57(3):275–7.
Yamanaka H, Hayashi Y, Watanabe Y, Uematu H, Mashimo T. Prolonged hoarseness and arytenoid cartilage dislocation after tracheal intubation. Br J Anaesth. 2009;103(3):452–5.
Combes X, Schauvliege F, Peyrouset O, Motamed C, Kirov K, Dhonneur G, Duvaldestin P. Intracuff pressure and tracheal morbidity: influence of filling with saline during nitrous oxide anesthesia. Anesthesiology. 2001;95(5):1120–4.
Fernandez R, Blanch L, Mancebo J, Bonsoms N, Artigas A. Endotracheal tube cuff pressure assessment: pitfalls of finger estimation and need for objective measurement. Crit Care Med. 1990;18(12):1423–6.
Sengupta P, Sessler DI, Maglinger P, Wells S, Vogt A, Durrani J, Wadhwa A. Endotracheal tube cuff pressure in three hospitals, and the volume required to produce an appropriate cuff pressure. BMC Anesthesiol. 2004;4(1):8.
Brodsky JB, Lemmens HJ. Tracheal width and left double-lumen tube size: a formula to estimate left-bronchial width. J Clin Anesth. 2005;17(4):267–70.
Griscom NT, Wohl ME. Dimensions of the growing trachea related to age and gender. AJR Am J Roentgenol. 1986;146(2):233–7.
Breatnach E, Abbott GC, Fraser RG. Dimensions of the normal human trachea. AJR Am J Roentgenol. 1984;142(5):903–6.
Pneumatikos IA, Dragoumanis CK, Bouros DE. Ventilator-associated pneumonia or endotracheal tube-associated pneumonia? An approach to the pathogenesis and preventive strategies emphasizing the importance of endotracheal tube. Anesthesiology. 2009;110(3):673–80.
Rello J, Soñora R, Jubert P, Artigas A, Rué M, Vallés J. Pneumonia in intubated patients: role of respiratory airway care. Am J Respir Crit Care Med. 1996;154(1):111–5.
Seegobin RD, van Hasselt GL. Endotracheal cuff pressure and tracheal mucosal blood flow: endoscopic study of effects of four large volume cuffs. Br Med J. 1984;288(6422):965–8.
Griscom NT. CT measurement of the tracheal lumen in children and adolescents. AJR Am J Roentgenol. 1991;156(2):371–2.
Liu J, Zhang X, Gong W, Li S, Wang F, Fu S, Zhang M, Hang Y. Correlations between controlled endotracheal tube cuff pressure and postprocedural complications: a multicenter study. Anesth Analg. 2010;111(5):1133–7.
Valentino J, Myers RK, Baker MD, Woodring JH. Utility of portable chest radiographs as a predictor of endotracheal tube cuff pressure. Otolaryngol Head Neck Surg. 1999;120(1):51–6.
Chikungwa M. Current nitrous oxide use in general anaesthesia: an electronic survey. Eur J Anaesthesiol. 2009;26(12):1088–90.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Shibasaki, M., Nakajima, Y., Shime, N. et al. Prediction of optimal endotracheal tube cuff volume from tracheal diameter and from patient height and age: a prospective cohort trial. J Anesth 26, 536–540 (2012). https://doi.org/10.1007/s00540-012-1371-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-012-1371-0