Abstract
Purpose
In some thoracic surgical procedures, the insertion of a double-lumen tube (DLT) is not feasible, or the altered use of a DLT and a single-lumen tube (SLT) is justified during the surgery. In the present article we report our experience with a new bronchial blocker, the EZ-blocker, in clinical use.
Methods
Data were obtained from ten patients undergoing thoracic surgery necessitating one-lung ventilation. For lung isolation, a combination of an SLT and an EZ-blocker was used. The time of insertion and positioning of the EZ-blocker, the lung deflation time with the EZ-blocker cuff inflated and deflated, and the cuff’s minimal occlusion volume were recorded. Based on the CT scan, the diameter of the main bronchi and the angle of the bifurcation were measured offline.
Results
The insertion duration of the EZ-blocker was 76 ± 15 s. Two malpositionings were caused by the too-deep positioning of the SLT used for introducing the EZ-blocker, which could be corrected within 65 ± 7 s. The use of the EZ-blocker allowed a short deflation time of the lung without (9.4 ± 0.7 s) and with (4.1 ± 0.7 s) administration of suctioning. The proper block was only dependent on the diameter of the main bronchi and was independent of the bifurcation angle.
Conclusions
Use of the EZ-blocker is easy and safe. The short insertion time and short lung deflation time through the lumen of the SLT allows its use in emergency situations or in cases of a difficult airway.
Similar content being viewed by others
Introduction
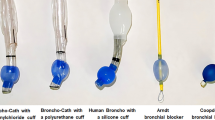
The majority of thoracic surgical procedures may require one-lung ventilation (OLV). To achieve this, for the sake of both fast insertion and the proper insertion of the tube, the double-lumen endotracheal tube (DLT) is the first choice. However, there are certain cases when intubation with DLT is not possible, or when the alternate use of a single-lumen tube (SLT) and a DLT during surgery is necessary. In those cases, bronchial blockers (BB) serve as ideal devices. Different BBs are commercially available, among which the EZ-blocker® (AnaesthIQ, Rotterdam, The Netherlands) is a newly developed device [1]. In the present study we report on our clinical experience with the introduction and intraoperative use of this BB. We also intended to assess how the individual anatomy of the main bronchi influences proper blocking with this type of blocking devices.
Subjects and methods
Inclusion of patients started after we had obtained permission from the local medical ethics committee (permission number: DEOEC RKEB/IKEB 3283-2010). All subjects gave written informed consent before surgery.
Description of the EZ-blocker
The main part of the device is a 650-mm-long catheter, 7 Fr. in diameter, containing four lumina. Its ending forms a symmetrical, double-stem, 4-cm-long Y-shape. Among the four lumina, two (one on each side) enable the connection between the lumen of the main bronchi and the environment, creating suction and providing oxygen. The other two lumina (one on each side) serve for inflating and deflating the cuff located at the stems of the Y-shaped ending. The extensions are fully symmetrical and are color coded for identification purposes [1, 2].
Anesthetic procedure
All patients received 5 mg midazolam and 0.5 mg atropine before induction of anesthesia. A thoracic epidural catheter was introduced at thoracic V–VII level, and after the testing dose 0.1 mg/ml bupivacaine plus 5 μg/ml fentanyl was administered at a rate of 0.1 ml/kg/h. Before induction, a radial artery cannula was introduced for continuous blood pressure measurements and for blood gas analysis. During the entire course of anesthesia, relaxometry (TOF Watch SX, NV Organon, Oss, The Netherlands) and BIS monitoring were performed (Aspect Medical Systems, Natick, MA, USA). General anesthesia was induced by fentanyl (2 μg/kg), propofol (2 mg/kg), and cis-atracurium (0.2 mg/kg). After induction, a single-lumen tube (SLT) (Rüschelit, Rüsch, Kernen, Germany) 9 mm in diameter was introduced under direct laryngoscopy. The positioning of the tube was performed and controlled by bronchoscopy; it was desired that the position should allow the opening of the stems of the Y-shaped bronchial blocker in the later course of anesthesia and surgery. After intubation, two-lung ventilation (TLV) was started by a tidal volume of 10 ml/kg and zero positive end-expiratory pressure (ZEEP, with maintenance of the peak airway pressure below 40 cmH2O until opening the pleural cavity (Draeger Primus anesthesia device; Draeger Lübeck, Germany). Maintenance of anesthesia was performed by administration of a mixture of sevoflurane and oxygen to maintain an appropriate depth of anesthesia. When the fixation of the single-lumen endotracheal tube was completed, the EZ-blocker was introduced under bronchoscopic control. Until this point, both cuffs of the blocker were deflated. Before opening the pleural cavity, the SLT was disconnected from the anesthesia device. Opening of the pleural cavity resulted in the collapse of the nondependent lung. At this point, the cuff of the bronchial blocker was inflated on the dependent side, and OLV was initiated with 5 ml/kg TV and a PEEP of 5 cmH2O.
Measurements during the procedure
Assessment of EZ-blocker® positioning
After fixation of the SLT, the time necessary for proper positioning of the blocker was recorded. The time required for laryngoscopy and intubation was not included in the time needed for proper positioning of the EZ-blocker. Measurement of insertion time started at the opening of the orifice of the multiport connector for insertion of the EZ-blocker and was stopped when the correct position was verified by bronchoscopy. Whenever proper positioning of the tube was not successful (two cases), the time necessary for correcting the position was also recorded in seconds.
Assessment of cuff pressures and minimal occlusion volumes
In supine position under closed chest condition, TLV was started with pressure-controlled mode using decelerating flow pattern with 25 cmH2O of peak and plateau inspiratory pressure. After a stabilization period of 1 min, tidal volume was recorded. The right cuff of the blocker was inflated under manometer control until reaching the pressure necessary to halve the tidal volume as compared to the initial value. This stage was considered proper endobronchial block. At this point, the cuff was deflated by a syringe and the volume that was aspirated from the cuff was measured. The same procedure was repeated with the cuff on the left side. With inflated cuffs we also registered the cuff pressures (in cmH2O and mmHg). Thus, we gathered information on the amount of air and cuff pressures necessary for proper blocking on the two sides.
Assessment of duration that is necessary for the lung to collapse (lung deflation time)
At open chest in lateral decubitus position with deflated blocker cuffs, the lungs were inflated until the nondependent lung reached the lower border of the rib cage. Duration of lung collapse was determined in different ways.
Collapsing the lung through the stem of the BB
After inflating the nondependent lung, the cuff on the same side was inflated while the cuff on the dependent side was deflated. The nondependent stem was made open to the air, and OLV was continued. We measured the duration of spontaneous deflation of the nondependent lung through the lumen of the BB.
Spontaneous lung collapse through the endotracheal tube
In a second setup, after reinflation of the nondependent lung, the BB cuff on the nondependent side was inflated for a short time, the dependent cuff remained deflated, and OLV was continued. After a short stabilization time, SLT was disconnected from the ventilator and the BB cuff on the nondependent side was deflated. Herewith the duration of spontaneous lung collapse through the lumen of the endotracheal tube was measured.
Facilitated lung collapse through the endotracheal tube
The setup here was the same as for the previous point. Additionally, after disconnecting from the endotracheal tube, a suction system with a force of 20 cmH2O was attached to the system and the duration of facilitated lung collapse was determined.
Proper collapse of the lung was defined by measuring the distance between the upper border of the superior lobe and the rib cage. A distance of 5.5 cm was considered appropriate. Determination of the appropriate distance was based on our previous measurements in which DLTs were used in ten patients. In this study, we asked the thoracic surgeons to determine the ideal collapse of the lung, and we measured the distance between the lung pleural surface and the upper border of the superior rib cage. In this series the distance for appropriate lung collapse was 5.5 cm on average. In the present study, in each case we reached the 5.5-cm lung collapse. The distance was measured with a sterile centimeter scale with open chest condition (Fig. 1).
A three-dimensional reconstruction was completed from all preoperative lung CT scans off-line in all patients (eFilm Lite software; MergeeMed, Division of Merge Healthcare, Milwaukee, WI, USA). We could obtain the particular images by utilizing the eFilm Lite software’s built-in multiplanar reconstruction function. The MPR function produces three sets of reconstructive images: coronal, sagittal, and transverse scans, by means of the appropriate tool icons. With this function we were able to select the appropriate planes that depict clearly the trachea, the bifurcation, and the origins of both bronchi. The diameters of the two main bronchi were measured perpendicular to the axis of the bronchus at the bifurcation. The angle of the bifurcation is the angle produced by the axes of the left and right bronchi. Measurements are shown in Fig. 2.
Measurement of bronchial anatomy on computed tomography (CT) scan. Diameters of the main bronchi and the angle of bifurcation were measured on the reconstruction scans at 1 cm below the tracheal bifurcation. a Measurement of diameter of right main bronchus. b Measurement of tracheal angle. c Measurement of diameter of left main bronchus
Statistical analysis
The Shapiro–Wilk test was used for assessment of data distribution. The Mann–Whitney test was used for comparison of the data. Regression analysis was used to assess the relationship between the diameters of the bronchi and cuff pressures as well as minimal occlusion volumes (MOVs). A P value <0.05 was considered as statistically significant.
Results
Demographic parameters and preoperative lung function test results are summarized in Table 1. Insertion and proper positioning of the EZ-blocker required 71 ± 12 s. Of the ten cases, malposition occurred in two. In both cases the reason for improper first positioning was the too-deep insertion of the endotracheal tube used for guidance of the blocker. With this too-deep positioning, the ending of the single-lumen endotracheal tube was less than 4 cm, making opening and proper positioning of the Y-shaped bronchial blocker impossible. In the case of initial malposition, the correction lasted for 150 and 180 s, respectively.
Comparison of deflation times using different methods
The deflation time of the lung through the lumen of the bronchial blocker was 755 ± 113 s for the left and 676 ± 61.7 s for the right side (P = 0.18). When doing lung deflation with the blocker cuff deflated (with lung collapse thus occurring through the lumen of the single-lumen endotracheal tube), the spontaneous deflation time was 9.4 ± 0.7 s, which could be further decreased by administration of a negative pressure of 20 cmH2O to 4.1 ± 0.7 s.
Relationship between the morphological properties of tracheal bifurcation and endobronchial block
When assessing the diameters of the left and right main bronchi, a significant difference was found (13.9 ± 2.6 mm for left side vs. 16.7 ± 2.1 mm for right side; P = 0.047). The average angle of the tracheal bifurcation was 73.8° + 15.9°. The amounts of air necessary for proper blocking as well as the corresponding cuff pressures on the two sides are summarized in Table 2. A greater amount of air was necessary for a proper endobronchial block on the right side than was necessary on the left side, with a correspondingly higher cuff pressure in the right-side cuff.
In a further analysis, we assessed whether a relationship exists between the ratios of main bronchial diameters and the ratios of MOV. It was found that a significant positive relationship exists between the two parameters; e.g., the greater the diameter of the main bronchus, the larger the amount of air that was necessary for proper endobronchial block (r 2 = 0.43; P = 0.04).
In contrast to this, no relationship could be detected between the angle of tracheal bifurcation and the MOV values, thus indicating that the angle has no impact on the proper endobronchial block (r 2 = 0.06; P = 0.487). Similarly, the bifurcation of the main bronchi did not have any impact on the time that was necessary for proper blocking (r 2 = 0.26; P = 0.19).
Discussion
In the present study, we report our clinical experience with a relatively new endobronchial device, the EZ-blocker. During thoracic anesthesia, double-lumen endotracheal tubes (DLT) are widely used in cases where one-lung ventilation is necessary. However, in some cases (such as difficult intubation, tracheostomy, or traumatized patients previously intubated with a SLT), the use of double-lumen tubes or the change from a single-lumen to a double-lumen tube may become difficult or risky. In such cases, endobronchial blockers (BB) may be indicated. Their use is, however, restricted to certain cases because DLTs are characterized by faster lung deflation time, a simpler introduction technique, and easier positioning and bronchial toilet, as well as lower costs [2–4].
When taking the insertion and positioning time into consideration, the average insertion time for a bronchial blocker is reported to be as high as 4–6 min [2]. In accordance with the present study, a previous report showed that the EZ-blocker may be positioned more quickly (1–3 min), more safely, and more easily than previously used types of bronchial blockers [1, 2, 4]. The unique design of the EZ-blocker makes proper positioning easier compared with classic BBs. This study does have an important limitation: there were no control groups to compare the EZ-blocker with the other types of BBs. Our aim was to present our experience with this BB and present some technical data that have not been previously reported in the literature. Regarding the other aspect, the rate of malpositions during insertion, in the present study malposition occurred in two cases. The reason for the improper first position was a too-deep initial introduction of the endotracheal tube that served as a guidance for the bronchial blocker. As described in the Methods section, these malpositionings can be avoided by a careful checking of the endotracheal tube position using a bronchoscope. A distance of at least 4 cm from the tracheal bifurcation is necessary to reach the correct position of the BB. Additionally, when the initial insertion of the BB was improper, the correction lasted a maximum of 3 min, which could be handled safely by administering additional oxygenation to the patients before repositioning the BB.
One disadvantage of the present blocking tube is the long deflation time of the lung through the lumen of the bronchial blocker. This delay might be tolerable during elective surgeries; however, the deflation time of more than 600 s seems to be too long in emergency surgical procedures and in special cases. For instance, in cases where the surgeon wants to open the chest safely as soon as possible and with minimal possible injury to the lung, or in cases where the two sides of the lung have to be ventilated alternatively during surgery (such as the Nuss procedure; [5]), these long deflation times seem to be inappropriate [6]. In such cases, as demonstrated in our study, by deflating the cuff of the BB and opening the endotracheal tube toward the environment (eventually combined with additional suctioning of air through the endotracheal tube), the deflation times may be gradually decreased.
We also intended to assess how individual variations of the tracheobronchial anatomy influence the insertion times and the amount of air necessary for proper inflation of the BB blocker cuffs. It has been demonstrated in previous studies that the diameter of the right main bronchus is larger by 2 mm on average [7]. Recently, it has also been demonstrated that the angle of the bifurcation shows individual variation [8]. Therefore, we hypothesized that anatomical variations possibly do influence proper insertion of and blocking by the EZ-blocker. It has been demonstrated that neither the angle of the bifurcation nor the diameters of the main bronchi influence the time necessary for proper BB insertion. In contrast to this, as the diameter of the right main bronchus was larger on the right side, correspondingly more air was necessary for BB cuff inflation on this side. A significant positive relationship was demonstrated between diameters of the main bronchi and MOV values.
A further critical question regarding endotracheal and blocker tubes is the cuff pressure and the pressure exerted by the cuff on the tracheal wall. In previous tests of the blocker tube cuff pressures, a 25 cmH2O positive airway pressure was used for testing the proper blocking with tubes [9]. In accordance with these tests, we also used this value for predetermination of critical airway pressure while testing the cuff pressures. In a previous study, Roscoe et al. demonstrated that the pressures exerted by the cuffs of DLTs ranged from 16 to 155 mmHg. Pressures exerted by the BB cuffs ranged from 39 to 194 mmHg. At intra-cuff volumes required to create a seal to 25 cmH2O positive pressure, the pressures exerted by the cuffs of all the devices were less than 30 mmHg [10]. In the present study we found that average cuff pressures were 39.79 ± 4 mmHg on the left side and 84.6 ± 5 mmHg on the right side, respectively. Taking into consideration that pressures exerted by the cuffs on the tracheal wall usually correspond to 10–20% of the cuff pressures [10], it may be estimated that in our series they correspond to 4–8 and 8.5–16 mmHg, which is far below the critical perfusion pressure of the bronchial wall (30 mmHg). The pressures exerted by the cuffs on the tracheal wall could be affected by the elasticity of cuff materials, and the relationship of the diameters between the cuff and the bronchus; thus, we need some basic research to prove our hypothesis for the EZ-blocker. We can suggest that the cuff of the EZ-blocker should be inflated at the minimum volume and at the minimum pressure for the maintenance of one-lung ventilation to prevent bronchial mucosal ischemia. Also, cuff pressure monitoring seems to be essential.
In summary, we have demonstrated in our study that the insertion of the EZ-blocker tube with bronchoscopic guidance is safe and may be performed easily. In cases of malpositioning, the correct positioning can be achieved within a fairly acceptable time. Proper blocking with the device is not influenced by anatomical variations of the tracheal bifurcation. The EZ-blocker allows for short lung deflation time through the endotracheal tube used for guidance of BB insertion, especially if it is combined with additional suctioning. Based on these properties, the use of this bronchial blocker may be recommended in thoracic anesthesia, especially in cases of emergency surgical procedures and in special situations.
References
Mungroop HE, Tjong Yoe Wai P, Morei MN, Loef BG, Epema AH. Lung isolation with a new Y-shaped endobronchial blocking device, the EZ-blocker®. Br J Anaesth. 2010;104:119–20.
Ruetzler K GG, Schmid W, Papp D, Nabecker S, Hutschala D, Lang G, Hager H. Randomized clinical trial comparing double-lumen tube and EZ-blocker for single-lung ventilation. Br J Anaesth. 2011;106:896–902.
Benumof JL. Difficult tubes and difficult airways. J Cardiothorac Vasc Anesth. 1998;12:131–2.
Narayanaswamy M, McRae K, Slinger P, Dugas G, Kanellakos GW, Roscoe A, Lacroix M. Choosing a lung isolation device for thoracic surgery: a randomized trial of three bronchial blockers versus double lumen tubes. Anesth Analg. 2009;108:1097–101.
Nuss D, Kelly RE Jr. Indications and technique of Nuss procedure for pectus excavatum. Thorac Surg Clin. 2010;20:583–97.
Ko R, McRae K, Darling G, Waddell TK, McGlade D, Cheung K, Katz J, Slinger P. The use of air in the inspired gas mixture during two-lung ventilation delays lung collapse during one-lung ventilation. Anesth Analg. 2009;108:1092–6.
Hampton T, Armstrong S, Russel WJ. Estimating the diameter of the left main bronchus. Anaesth Intensive Care. 2000;28:540–2.
Karabulut N. CT Assessment of tracheal carinal angle and its determinants. Br J Radiol. 2005;78:787–90.
Weiss M, Doell C, Koepfer N, Madjdpour C, Woitzek K, Bernet V. Rapid pressure compensation by automated cuff pressure controllers worsens sealing in tracheal tubes. Br J Anaesth. 2009;102:273–8.
Roscoe A, Kanellakos GW, McRae K, Slinger P. Pressure exerted by endobronchial devices. Anesth Analg. 2007;104:655–8.
Acknowledgments
The authors thank Daniel I. Sessler, MD, Michael Cudahy Professor and Chair, Department of Outcomes Research, Cleveland Clinic, Cleveland, OH, USA, and László L. Szegedi, MD, PhD, Professor of Anesthesiology, Department of Anesthesiology, Free University of Brussels, Brussels, Belgium, for their suggestions for this manuscript.
Conflict of interest
The authors have no conflict of interest to report.
Author information
Authors and Affiliations
Corresponding authors
About this article
Cite this article
Végh, T., Juhász, M., Enyedi, A. et al. Clinical experience with a new endobrochial blocker: the EZ-blocker. J Anesth 26, 375–380 (2012). https://doi.org/10.1007/s00540-011-1315-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-011-1315-0