Abstract
Purpose
Our intent was to identify whether cerebrovascular CO2 reactivity in diabetic patients is a risk factor for postoperative cognitive dysfunction after coronary artery bypass graft (CABG) surgery.
Methods
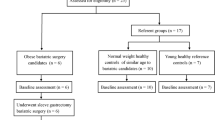
One hundred twenty-four diabetic patients undergoing elective CABG were studied and analyzed. Diabetic patients were divided into three groups: normal CO2 reactivity group (above 5%/mmHg), medium CO2 reactivity group (between 5 and 3%/mmHg), or impaired CO2 reactivity group (below 3%/mmHg). After the induction of anesthesia and before the start of surgery, cerebrovascular CO2 reactivity was measured for all patients. Hemodynamic parameters (arterial and jugular venous blood gas values) were measured during cardiopulmonary bypass. All patients underwent a battery of neurological and neuropsychological tests the day before surgery, 7 days after surgery, and 6 months after surgery.
Results
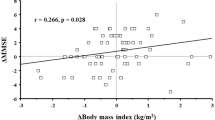
At 7 days, the rate of cognitive dysfunction in the impaired CO2 group was higher than in the other three groups (normal, 30%; medium, 25%; impaired, 57%; *P < 0.01 compared with the other groups). In contrast, at 6 months postoperatively, no significant difference in the rate of cognitive dysfunction was found among the three groups. Age, hypertension, CO2 reactivity, the duration for which jugular venous oxygen saturation (SjvO2) was less than 50%, ascending aorta atherosclerosis, diabetic retinopathy, and insulin therapy were independent predictors of short-term cognitive dysfunction in diabetic patients, and HbA1c, diabetic retinopathy, and insulin therapy were independent predictors of long-term cognitive dysfunction in diabetic patients.
Conclusions
We found that impaired cerebrovascular CO2 reactivity was associated with postoperative short-term cognitive dysfunction in diabetic patients.

Similar content being viewed by others
References
Hogue CW, Murphy SF, Schechtman KB, Davila-Roman VG. Risk factors for early or delayed stroke after cardiac surgery. Circulation. 1999;100:642–7.
Newman MF, Wolman R, Kanchuger M, Marschall K, Mora-Mangano C, Roach G, Smith LR, Aggarwal A, Nussmeier N, Herskowitz A, Mangano DT. Multicenter prospective stroke risk index for patients undergoing coronary artery bypass graft surgery. Circulation. 1996;94(suppl II):74–80.
Roach GW, Kanchuger M, Mangano CM, Newman M, Nussmeier N, Wolman R, Aggarwal A, Marschall K, Graham SH, Ley C. Adverse cerebral outcomes after coronary bypass surgery. N Engl J Med. 1996;335:1857–63.
Newman MF, Kirchner JL, Phillips-Bute B, Gaver V, Grocott H, Jones RH, Mark DB, Reves JG, Blumenthal JA. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med. 2001;344:395–402.
Newman MF, Croughwell ND, Blumenthal JA, Lowry E, White WD, Spillane W, Davis RD Jr, Glower DD, Smith LR, Mahanna EP. Predictors of cognitive decline after cardiac operation. Ann Thorac Surg. 1995;59:1326–30.
Croughwell N, Lyth M, Quill TJ, Newman M, Greeley WJ, Smith LR, Reves JG. Diabetic patients have abnormal cerebral autoregulation during cardiopulmonary bypass. Circulation. 1990;82(suppl):IV407–12.
Kadoi Y, Saito S, Fujita N, Goto F. Risk factors for cognitive dysfunction after coronary artery bypass graft surgery in patients with type 2 diabetes. J Thorac Cardiovasc Surg. 2005;129:576–83.
Kadoi Y, Saito S, Goto F, Fujita N. Decrease in jugular venous oxygen saturation during normothermic cardiopulmonary bypass predicts short-term postoperative neurologic dysfunction in elderly patients. J Am Coll Cardiol. 2001;38:1450–5.
Kadoi Y, Saito S, Kawahara F, Goto F, Owada R, Fujita N. Jugular venous bulb oxygen saturation in patients with preexisting diabetes mellitus or stroke during normothermic cardiopulmonary bypass. Anesthesiology. 2000;92:1324–9.
Kadoi Y, Saito S, Goto F, Someya T, Kamiyashiki S, Fujita N. Time course of changes in jugular venous oxygen saturation during hypothermic or normothermic cardiopulmonary bypass in patients with diabetic mellitus. Acta Anaesthesiol Scand. 2001;45:858–62.
Kadoi Y, Saito S, Yoshikawa D, Goto F, Fujita N, Kunimoto F. Increasing mean arterial blood pressure has no effect on jugular venous oxygen saturation in insulin-dependent patients during tepid cardiopulmonary bypass. Anesth Analg. 2002;95:266–72.
Kadoi Y, Saito S, Goto F, Fujita N. Slow rewarming has no effects on the decrease in jugular venous oxygen hemoglobin saturation and long-term cognitive outcome in diabetic patients. Anesth Analg. 2002;94:1395–401.
Kadoi Y, Hinohara H, Kunimoto F, Saito S, Ide M, Hiraoka H, Kawahara F, Goto F. Diabetic patients have an impaired cerebral vasodilatory response to hypercapnia under propofol anesthesia. Stroke. 2003;34:2399–403.
Miyoshi S, Morita T, Kadoi Y, Goto F. Analysis of the factors related to a decrease in jugular venous oxygen saturation in patients with diabetes mellitus during normothermic cardiopulmonary bypass. Surg Today. 2005;35:530–4.
Kessler C, Junge HM, Walker ML, Busack R, Albrecht DM, Ackeren KV. Reduced cerebral vasomotor reactivity as an indicator of postoperative confusion. Anaesthesia. 1997;52:433–7.
Kadoi Y, Kawauchi C, Ide M, Kuroda M, Takahashi K, Saito S, Mizutani A. Preoperative depression is a risk factor for postoperative short-term and long-term cognitive dysfunction in patients with diabetes mellitus. J Anesth. 2011;25:10–7.
Murkin JM, Newman SP, Stump DA, Blumenthal JA. Statement of consensus on assessment of neurobehavioral outcomes after cardiac surgery. Ann Thorac Surg. 1995;59:1289–95.
Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, Hadden D, Turner RC, Holman RR. Association of glycemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405012.
Pallas F, Larson DF. Cerebral blood flow in the diabetic patients. Perfusion. 1996;11:363–70.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kadoi, Y., Kawauchi, C., Kuroda, M. et al. Association between cerebrovascular carbon dioxide reactivity and postoperative short-term and long-term cognitive dysfunction in patients with diabetes mellitus. J Anesth 25, 641–647 (2011). https://doi.org/10.1007/s00540-011-1182-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-011-1182-8