Abstract
Purpose
Tracheal extubation and emergence procedures induce abrupt changes in hemodynamics and humoral responses. We conducted a prospective randomized study to examine the effects of the short-acting beta-1 blocker, landiolol, on hemodynamics during emergence from anesthesia in elderly patients with and without hypertension.
Methods
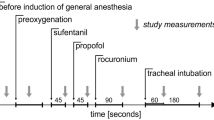
Thirty-one hypertensive and 32 normotensive elderly patients were randomly divided into two groups: a control (placebo group) and a landiolol infusion group. Landiolol was dissolved in 20 ml of saline and administered as an infusion at the rate of 0.125 mg·kg−1·min−1 for 1 min and then decreased to 0.04 mg·kg−1·min−1 until extubation. Control patients received an equal volume of saline. Heart rate and blood pressure were recorded every minute from immediately before the administration of landiolol up to the discontinuation of landiolol, and every 5 min from the discontinuation of landiolol to 30 min after termination of the infusion.
Results
Systolic blood pressure in the control group patients with hypertension increased during anesthesia emergence and tracheal extubation, as did the heart rate. Landiolol infusion in the elderly patients with hypertension partially prevented the increase in systolic blood pressure and completely prevented the increase in heart rate associated with emergence from anesthesia. Landiolol infusion in the elderly patients without hypertension brought about a decrease in heart rate during emergence and tracheal extubation.
Conclusion
This study indicates that the use of a landiolol infusion for preventing hemodynamic instability in elderly patients during the emergence period would be dependent on the presence or absence of hypertension in these patients.
Similar content being viewed by others
References
Miller KA, Harkin CP, Bailey PL. Postoperative tracheal extubation. Anesth Analg. 1995;80:149–172.
Kurian SM, Evans R, Fernandes NO, Sherry KM. The effect of an infusion of esmolol on the incidence of myocardial ischemia during tracheal extubation following coronary artery surgery. Anaesthesia. 2001;56:1163–1168.
Grillo P, Bruder N, Auquier P, Pellissier D, Gouin F. Esmolol blunts the cerebral blood flow velocity increase during emergence from anesthesia in neurosurgical patients. Anesth Analg. 2003;96:1145–1149.
Kovac A, Masiongale A. Comparison of nicardipine versus esmolol in attenuating the hemodynamic responses to anesthesia emergency and extubation. J Cardiothoracic Vasc Anesth. 1999;16:145–149.
Dryden CM, Smith DM, McLintic AJ, Pace NA. The effect of preoperative beta-blocker therapy on cardiovascular responses to weaning from mechanical ventilation and extubation after coronary artery bypass grafting. J Cardiothorac Vasc Anesth. 1993;7:547–550.
Muzzi DA, Black S, Losasso TJ, Cucchiara RF. Labetalol and esmolol in the control of hypertension after intracranial surgery. Anesth Analg. 1990;70:68–71
Mio Y. New ultra-short-acting beta-blockers: landiolol and esmolol—the effects on cardiovascular system. Masui. 2006;55:841–848.
Sasao J, Tarver SD, Kindscher JD, Taneyama C, Benson KT, Goto H. In rabbits, landiolol, a new ultra-short-acting betablocker, exerts a more potent negative chronotropic effect and less effect on blood pressure than esmolol. Can J Anaesth. 2001;48:985–989.
Dyson A, Isaac PA, Pennant JH, Giesecke AH, Lipton JM. Esmolol attenuates cardiovascular responses to extubation. Anesth Analg. 1990;71:675–678.
Nonaka A, Suzuki S, Abe F. The effects of continuous infusion of landiolol on heart rate changes after neostigmine-atropine administration during recovery from general anesthesia. Masui. 2006;55:1459–1462.
Minamizono T, Goyagi T, Nishikawa T. Effects of landiolol on hemodynamic changes during tracheal extubation (in Japanese). J Clin Anesth (Jpn). 2006;30:533–537
Ohata H, Ando T, Sudani T, Nagasaka Y, Fukuoka N, Dohi S. Effects of landiolol on hemodynamic changes during recovery from general anesthesia (in Japanese). J Clin Anesth (Jpn). 2004;24:579–585.
Shirasaka T, Iwasaki T, Hosokawa N, Komatsu M, Kasaba T, Takasaki M. Effects of landiolol on the cardiovascular response during tracheal extubation. J Anesth. 2008;22:322–325.
Prys-Roberts C, Meloche R, Poex P. Studies of anesthesia in relation to hypertension. I: cardiovascular responses of treated and untreated patients. Br J Anesth. 1971;43:122–137.
Muravchick S. Nervous system aging. In: McLeskey CH, editor. Geriatric anesthesiology. Baltimore: Williams & Wilkins; 1997. p. 29–41.
Kadoi Y, Saito S, Takahashi K. The comparative effects of sevo-flurane vs isoflurane on cerebrovascular carbon dioxide reactivity in patients with hypertension. Acta Anaesthesiol Scand. 2007;51:1382–1387.
Coriat P, Mundler O, Bouseau D, Fauchet M, Rous AC, Echter E, Viars P. Response of left ventricular ejection fraction to recovery from general anesthesia: measurement by gated radionuclide angiography. Anesth Analg. 1986;65:593–600.
Wellwood M, Aylmer A, Teasdale S. Extubation and myocardial ischemia (abstract). Anesthesiology. 1984;61:A132.
Stone JG, Foex P, Sear JW, Johnson LL, Khambatta HJ, Riner L. Risk of myocardial ischemia in treated and untreated hypertensive patients. Br J Anesth. 1988;61:675–679.
Sugiura S, Seki S, Hidaka K, Masuoka M, Tsuchida H. The hemodynamic effects of landiolol, an ultra-short-acting β1-selective blocker, on endotracheal intubation in patients with and without hypertension. Anesth Analg. 2007;104:124–129.
Slogoff S, Keats AS. Does perioperative myocardial ischemia lead to postoperative myocardial infarction? Anesthesiology. 1985;62:107–114.
Kimura T, Tanaka M, Nishikawa T. Comparison of heart rate changes after neostigmine-atropine administration during recovery from propofol-N2O and isoflurane-N2O anesthesia. J Anesth. 2002;16:23–27.
Naguib M, Gomaa M. Atropine-neostigmine mixture: a doseresponse study. Can J Anaesth. 1989;36:412–417.
Author information
Authors and Affiliations
About this article
Cite this article
Miyazaki, M., Kadoi, Y. & Saito, S. Effects of landiolol, a short-acting beta-1 blocker, on hemodynamic variables during emergence from anesthesia and tracheal extubation in elderly patients with and without hypertension. J Anesth 23, 483–488 (2009). https://doi.org/10.1007/s00540-009-0805-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-009-0805-9