Abstract
Purpose
For direct laryngoscopy, we compared midline and left-molar approaches with respect to ease of intubation, using a Macintosh blade. We investigated the relationship between failure of the left-molar approach and preoperative risk factors for difficult intubation.
Methods
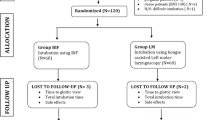
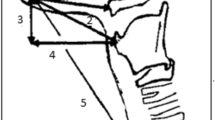
With local ethics committee approval, 200 consecutive adult, nonpregnant patients were included in the study. The demographic data, body mass index, Mallampati modified score, interincisor gap, and mentohyoid and thyromental distances were measured preoperatively. First, the Macintosh blade was inserted using the midline approach, and then optimal external laryngeal manipulation (OELM) was applied. Second, the blade was inserted using the left-molar approach. The glottic views were assessed according to the Cormack-Lehane classification before and after OELM in both approaches. In cases where tracheal intubation failed with the left-molar approach, the midline approach was applied again and endotracheal intubation took place.
Results
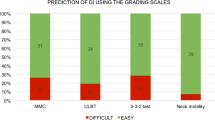
The grade I glottic view obtained using the midline approach without OELM did not change in 94.3% of the patients with the left-molar approach without OELM; in addition, the grade II glottic view improved to grade I in 52.8% of the patients with the same technique (P < 0.001). Although the number of patients with a grade I or II glottic view in the left-molar approach was 197, only 37 patients could be intubated using the left-molar approach. In addition, 59.5% of them were intubated at the second attempt with the left-molar approach, while the incidence of a second attempt was 1.2% with the midline approach (P < 0.001). There was no correlation between the preoperative risk factors for difficult intubation and failure of the left-molar approach.
Conclusion
Difficulty in the insertion of the endotracheal tube limits the efficacy of the left-molar approach. It is not possible to predict the failure of intubation with the left-molar approach by considering the preoperative risk factors.
Similar content being viewed by others
References
el-Ganzouri AR, McCarthy RJ, Tuman KJ, Tanck EN, Ivankovich AD. Preoperative airway assessment: predictive value of a multivariate risk index. Anesth Analg. 1996;82:1197–1204.
Henderson JJ. The use of paraglossal straight blade laryngoscopy in difficult tracheal intubation. Anaesthesia. 1997;52:552–560.
Yamamoto K, Tsubokawa T, Ohmura S, Itoh H, Kobayashi T. Left-molar approach improves the laryngeal view in patients with difficult laryngoscopy. Anesthesiology. 2000;92:70–74.
Arino JJ, Valesco JM, Gasco C, Lopez-Timoneda F. Straight blades improve visualization of the larynx while curved blades increase ease of intubation: a comparison of the Macintosh, Miller, McCoy, Belscope and Lee-Fiberview blades. Can J Anaesth. 2003;50:501–506.
Mallampati SR, Gatt SP, Gugino LD, Desai SP, Waraksa B, Freiberger D, Liu PL. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985;32:429–435.
Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia. 1987;42:487–490.
Cattano D, Panicucci E, Paolicchi A, Forfori F, Giunta F, Hagberg C. Risk factors assessment of the difficult airway: an Italian survey of 1956 patients. Anesth Analg. 2004;99:1774–1779.
Benumof JL, Cooper SD. Quantitative improvement in laryngoscopic view by optimal external laryngeal manipulation. J Clin Anesth. 1996;8:136–140.
Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–1111.
Sato N, Shingu K. Another reason to choose the left molar approach of laryngoscopy: to spare the incisor teeth. Anesthesiology. 2002;96:1279.
Farley C, Bowler I, Stacey M. The left molar approach assisting fiberoptic intubation. Anaesthesia. 2002;57:1031–1033.
Mentzelopoulos SD, Armaganidis A, Niokou D, Matsota P, Tzoufi M, Kelekis N, Soultanis K, Oikonomopoulos N, Kostopanagiotou G. MRI of the upper airway and McCoy-balloon laryngoscopy with left molar approach in a patient with arthrogyroposis multiplex congenita and previous unsuccessful endotracheal intubation. Anesth Analg. 2004;99:1879–1880.
Author information
Authors and Affiliations
About this article
Cite this article
Cuvas, O., Basar, H., Gursoy, N. et al. Left-molar approach for direct laryngoscopy: is it easy?. J Anesth 23, 36–40 (2009). https://doi.org/10.1007/s00540-008-0694-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-008-0694-3