Abstract
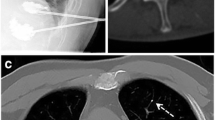
We reviewed long-term pain relief in four patients undergoing percutaneous vertebroplasty (PVP) for lumbar or back pain due to metastatic vertebral tumors. The patients received anesthesiological palliative care with analgesics until their death after PVP. Pain intensity, the presence or absence of recurrence of pain, changes in dosage of analgesics given before and after PVP, and complications associated with PVP were evaluated. A numerical rating scale (NRS) from 0 (no pain) to 10 (worst pain imaginable) was used to measure pain. The patients were three men and one woman (mean age, 58 years). PVP was performed in five vertebrae (one thoracic and four lumbar). The NRS scores on moving before PVP were 10, 8, 10, and 10. After PVP, NRS decreased to 0, 3, 5, and 0, respectively, within 72 h. No recurrence of pain in the treated area occurred until death in any of these patients. The dosages of analgesics given were decreased in two cases, but no changes were made in the other two cases. There were no complications associated with PVP. Percutaneous vertebro-plasty is a safe and effective treatment for long-time pain relief in patients with metastatic vertebral tumors.
Similar content being viewed by others
Author information
Authors and Affiliations
About this article
Cite this article
Yamada, K., Matsumoto, Y., Kita, M. et al. Long-term pain relief effects in four patients undergoing percutaneous vertebroplasty for metastatic vertebral tumor. J Anesth 18, 292–295 (2004). https://doi.org/10.1007/s00540-004-0252-6
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s00540-004-0252-6