Abstract
Background
Combination therapy with glecaprevir (GLE) and pibrentasvir (PIB) has high efficacy for pan-genotypic hepatitis C virus (HCV)-infected patients. However, the efficacy of the therapy for failures to prior direct-acting antiviral (DAA) regimens in real-world practice is not well known.
Methods
Thirty patients infected with HCV genotype 1b, 2a, 2b, or 3a who failed to respond during prior DAA therapies were treated with GLE/PIB for 12 weeks. HCV NS3 and NS5A drug resistance-associated variants (RAVs) were determined by direct sequencing.
Results
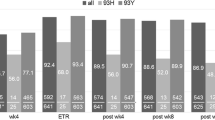
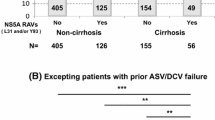
Twenty-eight out of 30 patients (93.3%) achieved SVR12 by GLE/PIB treatment. SVR12 rates were similar between patients with and without advanced liver fibrosis (94.7% and 91.0%, respectively). All 9 patients with genotype 2a, 2b, or 3a HCV infection achieved SVR12. However, two genotype 1b HCV-infected patients who failed previous daclatasvir plus asunaprevir treatment experienced HCV relapse after the end of GLE/PIB treatment. Direct sequence analysis showed the presence of NS3-D168E plus NS5A-L31I/P58S/Y93H RAVs in one patient and NS5A-L31F/P32del RAVs in another patient before GLE/PIB treatment. In the former patient, NS3-D168E plus NS5A-L31I/P58S/Y93H RAVs persisted, and additional NS5A-L28M/V75A variants emerged after HCV relapse.
Conclusions
GLE/PIB treatment for HCV-infected patients who did not respond to prior DAA treatments was highly effective regardless of liver fibrosis stage. However, some genotype 1b HCV-infected patients, especially those with NS5A-P32del, may have low susceptibility to the treatment.


Similar content being viewed by others
Abbreviations
- ASV:
-
Asunaprevir
- BEC:
-
Beclabuvir
- DAA:
-
Direct-acting antiviral
- DCV:
-
Daclatasvir
- GLE:
-
Glecaprevir
- HCV:
-
Hepatitis C virus
- LDV:
-
Ledipasvir
- PIB:
-
Pibrentasvir
- P32del:
-
P32 deletion
- RAV:
-
Resistance-associated variant
- RBV:
-
Ribavirin
- SOF:
-
Sofosbuvir
- SVR:
-
Sustained virological response
References
Kumada H, Suzuki Y, Ikeda K, et al. Daclatasvir plus asunaprevir for chronic HCV genotype 1b infection. Hepatology. 2014;59:2083–91.
Akuta N, Sezaki H, Suzuki F, et al. Ledipasvir plus sofosbuvir as salvage therapy for HCV genotype 1 failures to prior NS5A inhibitors regimens. J Med Virol. 2017;89:1248–54.
Teraoka Y, Uchida T, Imamura M, et al. Limitations of daclatasvir/asunaprevir plus beclabuvir treatment in cases of NS5A inhibitor treatment failure. J Gen Virol. 2018;99:1058–65.
Ng T, Tripathi R, Dekhtyar T, et al. In vitro antiviral activity and resistance profile of the next-generation HCV NS3-4A protease inhibitor glecaprevir. Antimicrob Agents Chemother. 2017;62:e01620.
Ng TI, Krishnan P, Pilot-Matias T, et al. In vitro antiviral activity and resistance profile of the next-generation hepatitis C virus NS5A inhibitor pibrentasvir. Antimicrob Agents Chemother. 2017;61:e02558.
Kwo PY, Poordad F, Asatryan A, et al. Glecaprevir and pibrentasvir yield high response rates in patients with HCV genotype 1–6 without cirrhosis. J Hepatol. 2017;67:263–71.
Asselah T, Kowdley KV, Zadeikis N, et al. Efficacy of glecaprevir/pibrentasvir for 8 or 12 Weeks in patients with HCV genotype 2, 4, 5, or 6 infection without cirrhosis. Clin Gastroenterol Hepatol. 2017;16:417–26.
Forns X, Lee SS, Valdes J, et al. Glecaprevir plus pibrentasvir for chronic hepatitis C virus genotype 1, 2, 4, 5, or 6 infection in adults with compensated cirrhosis (EXPEDITION-1): a single-arm, open-label, multicentre phase 3 trial. Lancet Infect Dis. 2017;17:1062–8.
Gane E, Lawitz E, Pugatch D, et al. Glecaprevir and pibrentasvir in patients with HCV and severe renal impairment. N Engl J Med. 2017;377:1448–55.
Poordad F, Felizarta F, Asatryan A, et al. Glecaprevir and pibrentasvir for 12 weeks for hepatitis C virus genotype 1 infection and prior direct-acting antiviral treatment. Hepatology. 2017;66:389–97.
Yoshimi S, Imamura M, Murakami E, et al. Long term persistence of NS5A inhibitor-resistant hepatitis C virus in patients who failed daclatasvir and asunaprevir therapy. J Med Virol. 2015;87:1913–20.
Sterling RK, Lissen E, Clumeck N, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43:1317–25.
Akuta N, Sezaki H, Suzuki F, et al. Retreatment efficacy and predictors of ledipasvir plus sofosbuvir to HCV genotype 1 in Japan. J Med Virol. 2017;89:284–90.
Backus LI, Belperio PS, Shahoumian TA, et al. Real-world effectiveness of ledipasvir/sofosbuvir in 4,365 treatment-naive, genotype 1 hepatitis C-infected patients. Hepatology. 2016;64:405–14.
Krishnan P, Schnell G, Tripathi R, et al. Integrated resistance analysis of CERTAIN-1 and CERTAIN-2 studies in HCV infected patients receiving glecaprevir and pibrentasvir in Japan. Antimicrob Agents Chemother. 2017;62:e02217–e02217.
Itakura M, Kurosaki C, Hasebe Y, et al. Complex pattern of resistance-associated substitutions of hepatitis C virus after daclatasvir/asunaprevir treatment failure. PLoS One. 2016;11:e0165339.
Gottwein JM, Pham LV, Mikkelsen LS, et al. Efficacy of NS5A inhibitors against hepatitis C virus genotypes 1–7 and escape variants. Gastroenterology. 2018;154:1435–48.
Kumada H, Watanabe T, Suzuki F, et al. Efficacy and safety of glecaprevir/pibrentasvir in HCV-infected Japanese patients with prior DAA experience, severe renal impairment, or genotype 3 infection. J Gastroenterol. 2017;53:566–75.
Teraoka Y, Uchida T, Imamura M, et al. Prevalence of NS5A resistance associated variants in NS5A inhibitor treatment failures and an effective treatment for NS5A-P32 deleted hepatitis C virus in humanized mice. Biochem Biophys Res Commun. 2018;500:152–7.
Gane EJ, Shiffman ML, Etzkorn K, et al. Sofosbuvir-velpatasvir with ribavirin for 24 weeks in hepatitis C virus patients previously treated with a direct-acting antiviral regimen. Hepatology. 2017;66:1083–9.
Lawitz E, Poordad F, Wells J, et al. Sofosbuvir-velpatasvir-voxilaprevir with or without ribavirin in direct-acting antiviral—experienced patients with genotype 1 hepatitis C virus. Hepatology. 2017;65:1803–9.
Acknowledgments
The authors thank Nobuko Yokoyama, Emi Nishio and Akemi Sata for clerical assistance. This research is partially supported by research funding from the Research Program on Hepatitis from the Japan Agency for Medical Research and Development, AMED (Grant number: 17fk0210104h0001). This study was performed at Hiroshima University and hospitals belonging to the Hiroshima Liver Study Group.
Members of the Hiroshima Liver Study Group include Shiomi Aimitsu (Matsuishi Hospital), Takahiro Azakami (Hiroshima Memorial Hospital), Koji Kamada (Shobara Red Cross Hospital), Yoshio Katamura (Onomichi General Hospital), Hiroiku Kawakami and Yoshiiku Kawakami (Kawakami Clinic), Takashi Kimura (Kimura Clinic), Shoichi Takahashi (Koyo New Town Hospital), Keiji Tsuji, Shintaro Takaki and Nami Mori (Hiroshima Red Cross Hospital & Atomic-bomb Survivors Hospital), Yuko Nagaoki (Mazda Hospital), Takashi Moriya (Chugoku Rosai Hospital) and Shuji Yamaguchi (Kure mutual aid Hospital).
Funding
The study was supported in part by research funding from the Research Program on Hepatitis from the Japan Agency for Medical Research and Development, AMED (Grant number: 17fk0210104h0001). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. There was no additional external funding received for this study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Kazuaki Chayama has received honoraria from Bristol-Myers Squibb and MSD K.K. and research funding from Dainippon Sumitomo Pharma and AbbVie. Michio Imamura has received research funding from Bristol-Myers Squibb.
Additional information
Members of Hiroshima Liver Study Group are listed in acknowledgments.
Rights and permissions
About this article
Cite this article
Osawa, M., Imamura, M., Teraoka, Y. et al. Real-world efficacy of glecaprevir plus pibrentasvir for chronic hepatitis C patient with previous direct-acting antiviral therapy failures. J Gastroenterol 54, 291–296 (2019). https://doi.org/10.1007/s00535-018-1520-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-018-1520-9