Abstract
Background and aims
The risk factors in the progression of nonalcoholic fatty liver disease (NAFLD) have not been fully clarified. Porphyromonas gingivalis (P.g) has been considered to be a confounding risk factor for systemic diseases. We aimed to evaluate the effect of P.g infection on risk of progression to NASH.
Methods
(1) Serum IgG antibody titers against P.g fimbriae (fimA) in 200 biopsy-proven NAFLD patients were measured by ELISA and compared with histological findings. (2) C57BL/6J mice were fed a control diet (CD) or high-fat diet (HFD) with or without P.g-odontogenic infection and analyzed histologically. Mouse livers were analyzed using CE–TOFMS and LC–TOFMS.
Results
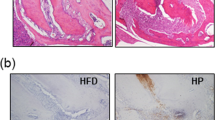
(1) A significant correlation between fibrosis progression and antibody titers against P.g possessing fimA type 4 was identified (P = 0.0081). Multivariate analysis identified older age and type 4 P.g-positivity as risk factors for advanced fibrosis. (2) Fibrosis and steatosis were more severe in HFD P.g(+) mice compared with HFD P.g(−) mice. In metabolome analysis, fatty acid metabolism was significantly disrupted with HFD in P.g-infected mouse livers. Monounsaturated/saturated fatty acid ratios were significantly higher in the HFD P.g(+) group than in the HFD P.g(−) group (P < 0.05). Moreover, expression levels of SCD1 and ELOVL6 were significantly reduced.
Conclusions
These results suggest that P.g infection is an important risk factor for pathological progression in NAFLD. Increase in the monounsaturated/saturated fatty acid ratio may be an important change that facilitates progression of NAFLD.





Similar content being viewed by others
Abbreviations
- NAFLD:
-
Nonalcoholic fatty liver disease
- P.g :
-
Porphyromonas gingivalis
- ELISA:
-
Enzyme-linked immunosorbent assay
- CE–TOFMS:
-
Capillary electrophoresis–time of flight mass spectrometry
- LC–TOFMS:
-
Liquid chromatography–time of flight mass spectrometry
- NASH:
-
Nonalcoholic steatohepatitis
- LPS:
-
Lipolysaccharide
- SCD:
-
Stearoyl-CoA desaturase
- Elovl:
-
Elongation of very long chain fatty acids
References
Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–31.
Ludwig J, Viggiano TR, McGill DB, et al. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55:434–8.
Marchesini G, Bugianesi E, Forlani G, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37:917–23.
Amarapurkar DN, Hashimoto E, Lesmana LA, et al. How common is non-alcoholic fatty liver disease in the Asia-Pacific region and are there local differences? J Gastroenterol Hepatol. 2007;22:788–93.
Hamaguchi M, Kojima T, Takeda N, et al. The metabolic syndrome as a predictor of nonalcoholic fatty liver disease. Ann Intern Med. 2005;143:722–8.
Kojima S, Watanabe N, Numata M, et al. Increase in the prevalence of fatty liver in Japan over the past 12 years: analysis of clinical background. J Gastroenterol. 2003;38:954–61.
Nakahara T, Hyogo H, Yoneda M, et al. Type 2 diabetes mellitus is associated with the fibrosis severity in patients with nonalcoholic fatty liver disease in a large retrospective cohort of Japanese patients. J Gastroenterol. 2014;49:1477–84.
Hamada S, Fujiwara T, Morishima S, et al. Molecular and immunological characterization of the fimbriae of Porphyromonas gingivalis. Microbiol Immunol. 1994;38:921–30.
Hamada S, Takada H, Ogawa T, et al. Lipopolysaccharides of oral anaerobes associated with chronic inflammation: chemical and immunomodulating properties. Int Rev Immunol. 1990;6:247–61.
Wilson M. Biological activities of lipopolysaccharides from oral bacteria and their relevance to the pathogenesis of chronic periodontitis. Sci Prog. 1995;78(Pt 1):19–34.
Seymour GJ, Ford PJ, Cullinan MP, et al. Relationship between periodontal infections and systemic disease. Clin Microbiol Infect. 2007;13(Suppl 4):3–10.
Pizzo G, Guiglia R, Lo Russo L, et al. Dentistry and internal medicine: from the focal infection theory to the periodontal medicine concept. Eur J Intern Med. 2010;21:496–502.
Wada K, Kamisaki Y. Roles of oral bacteria in cardiovascular diseases—from molecular mechanisms to clinical cases: involvement of Porphyromonas gingivalis in the development of human aortic aneurysm. J Pharmacol Sci. 2010;113:115–9.
Figuero E, Sanchez-Beltran M, Cuesta-Frechoso S, et al. Detection of periodontal bacteria in atheromatous plaque by nested polymerase chain reaction. J Periodontol. 2011;82:1469–77.
Iwamoto K, Kanno K, Hyogo H, et al. Advanced glycation end products enhance the proliferation and activation of hepatic stellate cells. J Gastroenterol. 2008;43:298–304.
Dickinson DP, Kubiniec MA, Yoshimura F, et al. Molecular cloning and sequencing of the gene encoding the fimbrial subunit protein of Bacteroides gingivalis. J Bacteriol. 1988;170:1658–65.
Tabeta K, Tanabe N, Yonezawa D, et al. Elevated antibody titers to Porphyromonas gingivalis as a possible predictor of ischemic vascular disease—results from the Tokamachi–Nakasato cohort study. J Atheroscler Thromb. 2011;18:808–17.
Yoneda M, Naka S, Nakano K, et al. Involvement of a periodontal pathogen, Porphyromonas gingivalis on the pathogenesis of non-alcoholic fatty liver disease. BMC Gastroenterol. 2012;12:16.
Furusho H, Miyauchi M, Hyogo H, et al. Dental infection of Porphyromonas gingivalis exacerbates high fat diet-induced steatohepatitis in mice. J Gastroenterol. 2013;48:1259–70.
Hyogo H, Tazuma S, Arihiro K, et al. Efficacy of atorvastatin for the treatment of nonalcoholic steatohepatitis with dyslipidemia. Metabolism. 2008;57:1711–8.
Ricci C, Longo R, Gioulis E, et al. Noninvasive in vivo quantitative assessment of fat content in human liver. J Hepatol. 1997;27:108–13.
Matteoni CA, Younossi ZM, Gramlich T, et al. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116:1413–9.
Brunt EM, Janney CG, Di Bisceglie AM, et al. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol. 1999;94:2467–74.
Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–21.
Yoneda M, Fujii H, Sumida Y, et al. Platelet count for predicting fibrosis in nonalcoholic fatty liver disease. J Gastroenterol. 2011;46:1300–6.
Liou I, Kowdley KV. Natural history of nonalcoholic steatohepatitis. J Clin Gastroenterol. 2006;40(Suppl 1):S11–6.
Abdelmalek MF, Diehl AM. Nonalcoholic fatty liver disease as a complication of insulin resistance. Med Clin N Am. 2007;91:1125–49.
Darveau RP. Periodontitis: a polymicrobial disruption of host homeostasis. Nat Rev Microbiol. 2010;8:481–90.
Nakano K, Inaba H, Nomura R, et al. Distribution of Porphyromonas gingivalis fimA genotypes in cardiovascular specimens from Japanese patients. Oral Microbiol Immunol. 2008;23:170–2.
Amano A, Kuboniwa M, Nakagawa I, et al. Prevalence of specific genotypes of Porphyromonas gingivalis fimA and periodontal health status. J Dent Res. 2000;79:1664–8.
Arimatsu K, Yamada H, Miyazawa H, et al. Oral pathobiont induces systemic inflammation and metabolic changes associated with alteration of gut microbiota. Sci Rep. 2014;4:4828.
Firneisz G. Non-alcoholic fatty liver disease and type 2 diabetes mellitus: the liver disease of our age? World J Gastroenterol. 2014;20:9072–89.
Romeo S, Kozlitina J, Xing C, et al. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet. 2008;40:1461–5.
Basantani MK, Sitnick MT, Cai L, et al. Pnpla3/Adiponutrin deficiency in mice does not contribute to fatty liver disease or metabolic syndrome. J Lipid Res. 2011;52:318–29.
Yamada K, Mizukoshi E, Sunagozaka H, et al. Characteristics of hepatic fatty acid compositions in patients with nonalcoholic steatohepatitis. Liver Int. 2015;35:582–90.
Wang X, Cao Y, Fu Y, et al. Liver fatty acid composition in mice with or without nonalcoholic fatty liver disease. Lipids Health Dis. 2011;10:234.
Puri P, Baillie RA, Wiest MM, et al. A lipidomic analysis of nonalcoholic fatty liver disease. Hepatology. 2007;46:1081–90.
Matsuzaka T, Atsumi A, Matsumori R, et al. Elovl6 promotes nonalcoholic steatohepatitis. Hepatology. 2012;56:2199–208.
Wang X, Ren Q, Wu T, et al. Ezetimibe prevents the development of nonalcoholic fatty liver disease induced by highfat diet in C57BL/6J mice. Mol Med Rep. 2014;10:2917–23.
Fernandez Gianotti T, Burgueno A, Gonzales Mansilla N, et al. Fatty liver is associated with transcriptional downregulation of stearoyl-CoA desaturase and impaired protein dimerization. PLoS One. 2013;8:e76912.
Author information
Authors and Affiliations
Contributions
TN: study concept and design, data acquisition, data analysis and interpretation, generation of figures, preparation of manuscript. HH: data acquisition, study concept and design, literature search. AO: data acquisition. YN: data acquisition. TK: data acquisition. DM: data acquisition. MT: data acquisition. NH: data acquisition. CNH: preparation of manuscript. AH: data acquisition. MI: data acquisition. YK: data acquisition. HA: data acquisition. HO: data acquisition. HA-C: data acquisition. HF: data acquisition, literature search. TS: data acquisition. HK: data acquisition. MM: data acquisition. TT: study concept and design, data acquisition. KA: staining of human liver biopsy samples. KC: study concept and design, data acquisition, data analysis and interpretation.
Corresponding author
Ethics declarations
Financial support
This work was supported in part by a research grant of the Suzuken Memorial Foundation.
Conflict of interest
All authors have no conflict of interest related to this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
535_2017_1368_MOESM1_ESM.pdf
Supplemental Figure 1 Metabolites in the principle metabolic pathways of HFD or HFD and P.-infected mouse liver (PDF 439 kb)
Rights and permissions
About this article
Cite this article
Nakahara, T., Hyogo, H., Ono, A. et al. Involvement of Porphyromonas gingivalis in the progression of non-alcoholic fatty liver disease. J Gastroenterol 53, 269–280 (2018). https://doi.org/10.1007/s00535-017-1368-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-017-1368-4