Abstract
Background
Studies of colorectal cancer (CRC) have suggested different mechanisms of carcinogenesis in men and women, young and old patients, right- and left sided tumors, and sporadic and familial tumors. These differences might be reflected in morphology.
Methods
CRCs from 1613 patients operated on in 2004–2006 in Sweden were histologically reviewed. Morphology was examined in relation to sex, age groups, location, and family history.
Results
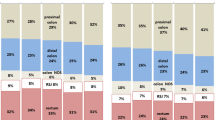
Tumors in the right colon were larger, of higher stage, more often poorly differentiated, more mucin-producing, more often had a peritumoral lymphocytic infiltrate and a high level of tumor-infiltrating lymphocytes (TILs), and more seldom had an infiltrating margin than tumors in the left colon and rectum (p < 0.0001 for most features). Young patients (<60 years) more seldom had multiple tumors but more often had perineural invasion, an infiltrative tumor margin, and high-stage tumors. Three features, TILs, medullary tumors, and invasive tumor margin, were related to sex. Only vascular invasion was related to familiality.
Conclusion
Location is the factor that has the most influence on tumor morphology. The results support the idea that different carcinogenic mechanisms may be involved in the right and left colon. Age is the most important determinant for the presence of multiple tumors and is a crucial factor for the aggressiveness of the disease.

Similar content being viewed by others
References
George B, Kopetz S. Predictive and prognostic markers in colorectal cancer. Curr Oncol Rep. 2011 [Epub ahead of print].
Woods SE, Narayanan K, Engel A. The influence of gender on colon cancer stage. J Womens Health. 2005;14:502–6.
Koo JH, Jalaludin B, Wong SK, Kneebone A, Connor SJ, Leong RW. Improved survival in young women with colorectal cancer. Am J Gastroenterol. 2008;6:1488–95.
Woods SE, Basho S, Engel AJ. The influence of gender on colorectal cancer stage: the state of Ohio, 1996–2001. J Womens Health. 2006;15:877–81.
Fairley TL, Cardinez CJ, Martin J, Alley L, Friedman C, Edwards B, et al. Colorectal cancer in U.S. adults younger than 50 years of age, 1998–2001. Cancer. 2006;107:1153–61.
Heys SD, Sherif A, Bagley JS, Brittenden J, Smart C, Eremin O. Prognostic factors and survival of patients aged less than 45 years with colorectal cancer. Br J Surg. 1994;81:685–8.
Snaebjornsson P, Jonasson L, Jonsson T, Möller PH, Theodors A, Jonasson JG. Colon cancer in Iceland—a nationwide comparative study on various pathology parameters with respect to right and left tumor location and patients’ age. Int J Cancer. 2010;127:2645–53.
Nawa T, Kato J, Kawamoto H, Okada H, Yamamoto H, Kohno H, et al. Difference in right- and left-sided colon cancer in patient characteristics, cancer morphology and histology. J Gastroenterol Hepatol. 2008;23:418–23.
Meguid RA, Slidell MB, Wolfgang CL, Wolfgang CL, Chang DC, Ahuja N. Is there a difference in survival between right- versus left-sided colon cancers? Ann Surg Oncol. 2008;15:2388–94.
Levi F, Randimbison L, La Vecchia C. Trends in subsite distribution of colorectal cancers and polyps from the Vaud Cancer Registry. Cancer. 1993;72:46–50.
Obrand DI, Gordon PH. Continued change in the distribution of colorectal carcinoma. Br J Surg. 1998;85:246–8.
Grady WM. Genetic testing for high-risk colon cancer patients. Gastroenterology. 2003;124:1574–94.
Lindblom A, Ghazi S, Liu T, Lagerstedt K, Papadogiannakis N. Hereditary non-polyposis colorectal cancer (HNPCC); definition and diagnostics in 2005. Research Trends. 2006;2:21–31.
Fink D, Aebi S, Howell SB. The role of DNA mismatch repair in drug resistance. Clin Cancer Res. 1998;4:1–6.
Ward R, Meagher A, Tomlinson I, O’Connor T, Norrie M, Wu R, et al. Microsatellite instability and the clinicopathological features of sporadic colorectal cancer. Gut. 2001;48:821–9.
Vasen HF, Mecklin JP, Khan PM, Lynch HT. The International Collaborative Group on Hereditary Non-Polyposis Colorectal Cancer (ICG-HNPCC). Dis Colon Rectum. 1991;34:424–5.
Ghazi S, von Holst S, Picelli S, Lindforss U, Tenesa A, Farrington SM, et al. Colorectal cancer susceptibility loci in a population-based study: associations with morphological parameters. Am J Pathol. 2010;177:2688–93.
Wittekind C, Greene FL, Hutter RV, Sobin LH, Klimpfinger M. TNM atlas. 5th ed. Paris: Springer; 2005.
Hamilton SR, Aaltonen LA. World Health Organization classification of tumors, pathology and genetics of tumors of the digestive system. Lyon: IARC Press; 2000.
Chandler I, Houlston RS. Interobserver agreement in grading colorectal cancers–findings from a nationwide web-based survey of histopathologists. Histopathology. 2008;52:494–9.
Young J, Simms LA, Biden KG, Wynter C, Whitehall V, Karamatic R, et al. Features of colorectal cancers with high-level microsatellite instability occurring in familial and sporadic settings: parallel pathways of tumorigenesis. Am J Pathol. 2001;159:2107–16.
Smyrk TC, Watson P, Kaul K, Lynch HT. Tumor infiltrating lymphocytes are a marker for microsatellite instability in colorectal carcinoma. Cancer. 2001;91:2417–22.
Jass JR. Role of the pathologist in the diagnosis of hereditary non-polyposis colorectal cancer. Dis Marker. 2004;20:215–24.
Ueno H, Murphy J, Jass JR, Mochizuki H, Talbot IC. Tumor “budding” as an index to estimate the potential of aggressiveness in rectal cancer. Histopathology. 2002;40:127–32.
Jass JR, Ajioka Y, Allen JP, Chan YF, Cohen RJ, Nixon JM, et al. Assessment of invasive growth pattern and lymphocytic infiltration in colorectal cancer. Histopathology. 1996;28:543–8.
Samowitz WS, Curtin K, Ma KN, Schaffer D, Coleman LW, Leppert M, et al. Microsatellite instability in sporadic colon cancer is associated with an improved prognosis at the population level. Cancer Epidemiol Biomarkers Prev. 2001;9:917–23.
Wong NA, Malcomson RD, Jodrell DI, Groome NP, Harrison DJ, Saunders PT. ERbeta isoform expression in colorectal carcinoma: an in vivo and in vitro study of clinicopathological and molecular correlates. J Pathol. 2005;207:53–60.
Breivik J, Lothe RA, Meling GI, Meling GI, Rognum TO, Børresen-Dale AL, et al. Different genetic pathways to proximal and distal colorectal cancer influenced by sex-related factors. Int J Cancer. 1997;74:664–9.
Slattery ML, Potter JD, Curtin K, Edwards S, Ma KN, Anderson K, et al. Estrogen reduces and withdrawal of estrogens increase risk of microsatellite instability-positive colon cancer. Cancer Res. 2001;61:126–30.
Börger ME, Gosens MJEM, Jeuken JWM, van Kempen LC, van de Velde CJ, van Krieken JH, et al. Signet ring cell differentiation in mucinous colorectal carcinoma. J Pathol. 2007;212:278–86.
Gopalan V, Smith RA, Ho YH, Lam AK. Signet-ring cell carcinoma of colorectum–current perspectives and molecular biology. Int J Colorectal Dis. 2011;26:127–33.
Li F-Y, Lai M-D. Colorectal cancer, one entity or three. J Zhejiang Univ Sci B. 2009;10:219–29.
Compton CC. Colorectal carcinoma: diagnostic, prognostic, and molecular features. Mod Pathol. 2003;16:376–88.
Horn A, Dahl O, Morild I. Venous and neural invasion as predictors of recurrence in rectal adenocarcinoma. Dis Colon Rectum. 1991;34:798–804.
Lee YT. Local and regional recurrence of carcinoma of the colon and rectum: tumour-host factors and adjuvant therapy. Surg Oncol. 1995;4:283–93.
Harrison JC, Dean PJ, el-Zeky F, Vander Zwaag R. From Dukes through Jass: pathological prognostic indicators in rectal cancer. Hum Pathol. 1994;25:498–505.
Heys SD, O’Hanrahan TJ, Brittenden J, Eremin O. Colorectal cancers in young patients: a review of the literature. Eur J Surg Oncol. 1994;3:225–31.
Newland RC, Dent OF, Lyttle MN, Chapuis PH, Bokey EL. Pathologic determinants of survival associated with colorectal cancer with lymph node metastases. A multivariate analysis of 579 patients. Cancer. 1994;73:2076–82.
Michelassi F, Ayala JJ, Balestracci T, Goldberg R, Chappell R, Block GE. Verification of a new clinicopathologic staging system for colorectal adenocarcinoma. Ann Surg. 1991;214:11–8.
Takebayashi Y, Akiyama SI, Yamada K, Akiba S, Aikou T. Angiogenesis as an unfavorable prognostic factor in human colorectal carcinoma. Cancer. 1996;78:226–31.
Compton CC, Fielding L, Burgart LJ. Prognostic factors in colorectal cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med. 1999;124:979–94.
Sternberg A, Amar A, Alfici R, Groisman G. Conclusions from a study of venous invasion in stage IV colorectal adenocarcinoma. J Clin Pathol. 2002;55:17–21.
Blenkinsopp WK, Stewart-Brown S, Blesovsky L, Kearney G, Fielding LP. Histopathology reporting in large bowel cancer. J Clin Pathol. 1981;34:509–13.
Zlobec I, Höller S, Tornillo L, Terracciano L, Lugli A. Combined histomorphologic and immunohistochemical phenotype to predict the presence of vascular invasion in colon cancer. Dis Colon Rectum. 2009;52:1114–21.
Lin M, Lin H-Z, Ma S-P, Ji P, Xie D, Yu JX. Vascular endothelial growth factor-A and -C: expression and correlations with lymphatic metastases and prognosis in colorectal cancer. Med Oncol. 2011;28:151–8.
Lagerstedt Robinson K, Liu T, Vandrovcova J, Halvarsson B, Clendenning M, Frebourg T, et al. Lynch syndrome (hereditary nonpolyposis colorectal cancer) diagnostics. J Natl Cancer Inst. 2007;99:291–9.
Olsson L, Lindblom A. Family history of colorectal cancer in a Swedish county. Fam Cancer. 2003;2:87–93.
Ueno H, Jones AM, Wilkinson KH, Jass JR, Talbot IC. Histological categorization of fibrotic cancer stroma in advanced rectal cancer. Gut. 2004;53:581–6.
Acknowledgments
We thank all patients and their spouses. We also thank Berith Wejderot for excellent technical assistance.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The members of The Low-Risk Colorectal Cancer Study Group are listed in the Appendix.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
The members of the Low-Risk Colorectal Cancer Study Group are: David Edler, Karolinska Universitetssjukhuset/Solna (Stockholm); Claes Lenander, Mag-tarm-centrum, Ersta sjukhus (Stockholm); Johan Dalén, S:t Görans sjukhus (Stockholm); Fredrik Hjern, Danderyds sjukhus (Danderyd); Nils Lundqvist, Norrtälje sjukhus (Norrtälje); Ulrik Lindforss, Södertälje sjukhus (Södertälje); Lars Påhlman, Akademiska sjukhuset (Uppsala); Kennet Smedh, Centrallasarettet (Västerås); Anders Törnqvist, Centralsjukhuset (Karlstad); Jörn Holm, Länssjukhuset Gävle-Sandviken (Gävle); Martin Janson, Karolinska Universitetssjukhuset/Huddinge (Huddinge); Magnus Andersson, Universitetssjukhuset (Örebro); Susanne Ekelund, Södersjukhuset (Stockholm); and Louise Olsson, Mälarsjukhuset (Eskilstuna).
Rights and permissions
About this article
Cite this article
Ghazi, S., Lindforss, U., Lindberg, G. et al. Analysis of colorectal cancer morphology in relation to sex, age, location, and family history. J Gastroenterol 47, 619–634 (2012). https://doi.org/10.1007/s00535-011-0520-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-011-0520-9