Abstract
Pancreatic cancer is the fourth leading cause of cancer death in our society, with a mortality that virtually parallels its incidence, a median survival of <12 months even with maximal therapy, and a 5-year survival rate of <5 %. The diversity of clinical outcomes and the molecular heterogeneity of histopathologically similar cancer types, incomplete knowledge of the genomic aberrations that drive carcinogenesis and the lack of therapeutics that specifically target most known genomic aberrations necessitates large-scale detailed analysis of cancer genomes to identify novel potential therapeutic strategies. As part of the International Cancer Genome Consortium (ICGC), the Australian Pancreatic Cancer Genome Initiative (APGI) used exomic sequencing and copy number analysis to define genomic aberrations that characterize a large, clinically focused, prospectively accrued cohort of patients with pancreatic cancer. The cohort consisted of early (clinical stages I and II) non-pre-treated patients with pancreatic ductal adenocarcinoma who underwent operative resection with curative intent. We devised approaches to adjust for low epithelial content in primary tumours and to define the genomic landscape of pancreatic cancer to identify novel candidate driver genes and mechanisms. We aim to develop stratified, molecular phenotype-guided therapeutic strategies using existing therapeutics that are either rescued, repurposed, in development, or are known to be effective in an undefined subgroup of PC patients. These are then tested in primary patient-derived xenografts and cell lines from the above deeply characterized cohort. In addition, we return information to treating clinicians that influences patient care and are launching a clinical trial called IMPaCT (Individualized Molecular Pancreatic Cancer Therapy). This umbrella design trial randomizes patients with metastatic disease to either standard first-line therapy with gemcitabine, or a molecular phenotype-guided approach using next-generation sequencing strategies to screen for actionable mutations defined through the ICGC effort.
Similar content being viewed by others
Introduction
Pancreatic cancer is the fourth leading cause of cancer death, with an overall 5-year survival rate of <5 % [1]. Pancreatectomy remains the single most effective treatment modality, with recent advances in neoadjuvant and adjuvant chemotherapeutic regimens resulting in some added improvement in outcomes. Only 20 % of patients present with disease which is suitable for resection [2]. Those who undergo resection and receive adjuvant therapy have a median survival of 12–22 months and a 5-year survival of 20–25 % [3]. Although there is evidence of significant efficacy in subgroups of patients, systemic therapies on the whole are only modestly effective, and the median survival for patients with metastatic disease remains around 6 months. A better understanding of the molecular pathology of pancreatic cancer will facilitate the delineation of molecular phenotypes and as a consequence define subgroups of patients that respond to specific therapies.
Molecular pathology of pancreatic cancer
Pancreatic cancer most commonly develops through a series of intraductal epithelial lesions called pancreatic intraepithelial neoplasms (PanIN) [4], where minimally dysplastic epithelium progresses to more severe dysplasia and finally to invasive carcinoma with the successive accumulation of genetic mutations. The molecular events include the activation of the KRAS oncogene, inactivation of the CDKN2A tumour suppressor gene (p16INK4A), and mutation and/or inactivation of TP53 and SMAD4 tumour suppressor genes. Pancreatic cancer can also arise from other precursor lesions including intraductal papillary mucinous neoplasms (IPMN) and mucinous cystic neoplasms (MCN).
Almost all pancreatic cancers harbour one or more of these four genetic aberrations; however, as we understand more about the genomic landscape of pancreatic cancer, we are uncovering significant complexity and heterogeneity. Despite this heterogeneity of individual genetic events, they can be organized into 12 functional cancer-related pathways (Fig. 1) [5].
The genomic landscape of pancreatic cancer
The International Cancer Genome Consortium (ICGC; http://www.icgc.org/) was organized to coordinate the generation of comprehensive catalogues of the genomic abnormalities present in 50 different cancer types and/or subtypes that are of clinical and societal importance around the world [6]. The APGI is Australia’s main contribution to the ICGC, and aims to sequence the genome, epigenome and transcriptome of ~350 pancreatic cancers in a project primarily incorporating the Garvan Institute of Medical Research in Sydney and the Institute of Molecular Biosciences (University of Queensland) in Brisbane, with centres Australia-wide. Strict Standards of Procedure (SOP) relating to sample acquisition, clinical data management and biospecimen handling were put in place from the outset, allowing for a high-quality, well annotated clinical cohort to be collected with real-time follow-up in a prospective non-intervention cohort design.
Cellularity, mutation detection and copy number variation analysis
Desmoplasia is a key feature of pancreatic cancer and is a major challenge for genomic research and clinical diagnostics. The extensive desmoplastic reaction results in a low percentage of neoplastic epithelial content, which in turn reduces the sensitivity for detecting somatic mutations, copy number events, tumour-specific expression and alterations in DNA methylation. In order to better inform the impact of tumour cellularity on the sensitivity of mutation detection, we recently described two novel approaches. First, deep amplicon-based sequencing of KRAS (average depth of 1,000×) to estimate mutant allele counts for KRAS, and second, high-density single nucleotide polymorphism (SNP) array-based cellularity estimates using a novel algorithm (qpure) [7]. KRAS mutation was identified in 93 % of samples with cellularity ranging from 5 to 85 %. The sensitivity of mutation detection was estimated by sequencing samples from a mixing experiment with a known proportion of DNA from a cancer cell line and matched germline. This provided the ability to predict the confidence of mutation detection across samples.
In a set of 99 samples, we detected 2,627 high-confidence mutations, 2,016 of which were non-silent (Fig. 2). Approximately 75 % of these events (1,502 of 2,016) were independently validated via an orthogonal sequencing method such as targeted sequencing using Ion Torrent®. There was an average of 26 mutations per patient and they ranged between one and 116 mutations. In the 79 mutated genes that were observed to occur more than once, 38 (48 %) were reported previously by Jones et al. [8] and 189 of all 998 (19 %) mutated genes were reported by the same study of 24 samples. However, 1,456 novel mutations were also identified, most of which occurred at low frequency, further demonstrating the molecular heterogeneity of pancreatic ductal adenocarcinoma (PDAC).
The genomic landscape of pancreatic cancer. This word cloud represents mutated somatic genes of 99 patients with PDACs [10]. The font size of each gene corresponds to the frequency of mutation. KRAS, TP53, CDKN2A and SMAD4, making up the top four frequently mutated genes, dominate a landscape where the vast majority of genes are mutated at low frequency (word cloud created using wordle.net)
We then used Significant Mutated Gene analysis [9] with genes containing non-silent mutations that occurred in two or more cancers, and identified 16 genes. These 16 genes included those known to occur in PDAC: KRAS, TP53, CDKN2A, SMAD4, MLL3, TGFBR2, ARID1A and SF3B1. Novel significantly mutated genes [10] were also identified and included genes involved in chromatin modification (EPC1 and ARID2) and ATM. ATM was recently implicated as a PDAC susceptibility gene through bi-allelic inactivation in a case of familial PDAC [11]. Additionally, there were also mutations detected in five other genes not previously reported: ZIM2, MAP2K4, NALCN, SLC16A4 and MAGEA6. When copy-number variation analysis was performed, GISTIC2.0 analysis [12] identified 30 genes affected by copy-number alterations with a Q < 0.0001, which included losses of CDKN2A and SMAD4 [10].
Making sense of genomic data
Simply cataloguing mutations or copy number alterations in a tumor is informative, but it does not define oncogenic drivers, tumor dependencies or targetable mechanisms to inform novel therapeutic strategies. This requires in-depth understanding of the functional importance of the genetic aberrations, which often requires multi-disciplinary input of functional data and the application of other approaches such as comparative genomics. To this end, we have adopted an integrative approach to enrich for “driver” as compared to “passenger” mutations. Briefly, this includes:
-
1.
Definition of recurrent events, particularly affecting specific functional regions; this has been the mainstay of historic oncogene discovery, but the discovery of such events is diminishing.
-
2.
Exploration of known characteristics of cancer genes (e.g. multiple forms of inactivation of tumor suppressor genes) and computational approaches that predict the functional consequences of specific mutations (e.g. Polyphen2).
-
3.
Integrative analysis of genomic, transcriptomic and epigenomic data and other approaches such as proteomics, phosphoproteomics and metabolomics, which likely enriches for drivers, particularly since multiple forms of regulation are a characteristic of normal cellular processes which can be dysregulated in many different ways in cancer.
-
4.
Correlation with independent large-scale functional screens including in-vitro shRNA knockdown and murine Sleeping-Beauty-mediated transposon screens.
-
5.
Pathway analysis.
-
6.
Comparative genomics through sequencing genetically engineered and other mouse models of PDAC.
-
7.
Correlation with clinico-pathological variables.
Integrative functional genomics of PDAC
Despite significant advances in computational algorithms, experimental evidence of functional relevance is pivotal, and computational approaches only enrich and prioritize candidate driver genes for ongoing investigation. In our recent study, we integrated data from three experimental biological screens to infer functional consequences for the individual genomic events and pathways (Fig. 3). These included data from two independent Sleeping Beauty transposon (SB) mutagenesis screens in Kras transgenic mouse models of PDAC [13, 14] and an in-vitro short hairpin RNA (shRNA) screen which examined the consequences for survival of down-regulating 11,194 putative cancer genes in a panel of 102 cell lines [15]. Data from these screens confirmed the functional importance of KRAS, TP53, CDKN2A and SMAD4 mutations and attributed potential functional relevance to other significantly mutated genes in our study—MLL3, TGFBR2, SF3B1, EPC1, ARID1A, ARID2, MAP2K4, ATM, NALCN, ZIM2, SLC16A4—and many other genes mutated at low frequency.
Integrative strategy to enrich for driver mutations in PDAC. Genes affected by a range of mechanisms, including mutation and copy number alteration, are identified from genome sequencing and array-based analyses. In-vivo Sleeping Beauty mutagenesis screens were performed in mice with conditional KRAS G12D mutant pancreases, which result in tumor formation if the transposon insertion disrupts a key tumor suppressor or oncogene. In-vitro functional screens target cancer cell lines with short hairpin RNA, which results in either diminished or enhanced ability to survive, depending on whether an oncogene or tumor suppressor gene is targeted, respectively. The intersection of these datasets can identify high-priority driver genes and pathways. (Reprinted and adapted with permission from Macmillan Publishers Ltd: Nature Reviews Cancer [23], copyright 2012)
Pathway analysis and the Axon Guidance Pathway
To gain greater insight into underlying mechanisms of importance in PDAC, a series of pathway analyses was performed. Genes that were recurrently mutated in two or more individual cancers were analyzed using GeneGO [16]. Mechanisms known to be important in cancer––G1/S checkpoint machinery, apoptosis, regulation of angiogenesis and TGF-β––signaling were identified as previously described (Fig. 1). Novel gene signatures were also enriched, including axon guidance, which had one of the strongest associations. Published mutation data of the 24 PDACs from Jones et al. [8] was subsequently included, and strengthened this association.
Genes traditionally described as being involved in axon guidance (semaphorins, slits, netrins and ephrins) are involved in regulating normal neuronal migration and positioning during embryonic development. They have recently been implicated in cancer cell growth, survival, invasion and angiogenesis [17]. Mutations in SLIT2 and its receptors ROBO1 and ROBO2, and copy number loss to SLIT2 and ROBO1 were identified in 20 % of the cohort. Based on these findings, we hypothesized that aberrant SLIT/ROBO signaling may be a common feature of PDAC. In addition, 21 % of tumors had mutations (3 %) or copy number amplification (18 %) in class 3 semaphorins (SEMA3A and SEMA3E). SEMA3A amplification correlated with high mRNA expression and patients with high SEMA3A and PLXNA1 (another molecule central to semaphorin signaling) mRNA expressing tumors had a poor prognosis. Further supportive evidence for the potential importance of axon guidance came from experiments using in-vitro acinar-to-ductal metaplasia and in-vivo pancreatic injury models. Expression levels of components of SLIT/ROBO and semaphorin signaling changed progressively from normal pancreas, through acinar-to-ductal metaplasia and pancreatic injury, to genetically engineered murine PDAC. These findings further supported a role for the dysregulation of axon guidance genes in pancreatic cancer initiation and progression.
Although characterization of the genomic events present in PDAC enriches for candidate driver genes and mechanisms, promising novel strategies will require validation in well-characterized pre-clinical models and well-designed biomarker-driven early-phase clinical trials. Efficient translation into clinical patient care remains challenging, but holds the promise of improved outcomes for cancer.
Translation into patient care
Developing genotype-guided therapies for pancreatic cancer
Dramatic improvements in overall survival have been observed in various other cancer types such as breast cancer and haematological malignancies owing in large part to the development of targeted therapeutic strategies. Pancreatic cancer is characterized by substantial genomic heterogeneity. Based on this heterogeneity, responsive phenotypes for each targeted therapy are likely to fall below the detection threshold of even large randomized trials. A molecular taxonomy in addition to the existing organ and morphology-based classification where individual cancers are grouped and selected for optimal therapy based on their molecular phenotype or “biotype” may improve outcomes for PDAC (Fig. 4).
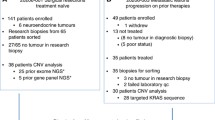
Currently, the common recurrent mutations in pancreatic cancer, namely KRAS, TP53, SMAD4 and CDKN2A, are not treatable with drugs. Therefore, in the case of pancreatic cancer, genotype-guided therapeutic strategy could be developed on two fronts. First, known molecular aberrations with target–drug combinations that are approved for treatment in other malignancies could be tested in the appropriate molecular subtype. Second, novel molecular aberrations defined through genomic sequencing efforts that may or may not have a specific inhibitor would focus ongoing investigation. To advance such genotype-guided strategies, novel approaches are being developed to test molecular target–drug combinations. For target–drug combinations ready for clinical testing, a biomarker-driven early-phase clinical trial has been designed for PC and is now open for recruitment (see below). For target–drug combinations not yet ready for clinical testing, well-characterized pre-clinical models including ~25 patient-derived cell lines (PDCL) and ~70 patient-derived xenografts (PDX) have been generated for functional interrogation and validation (Fig. 5) [18].
Translation and implementation strategy for APGI. Genomic sequence data is used to inform a biomarker-driven early-phase clinical trial for target–drug combinations ready for clinical testing. The study has been designed and is now open for recruitment. For target–drug combinations yet to be ready for clinical testing, the data is used to inform well-characterized pre-clinical therapeutic testing models for functional interrogation and validation
Individualized Molecular Pancreatic Cancer Therapy
The Individualized Molecular Pancreatic Cancer Therapy (IMPaCT) trial screens patients for actionable molecular phenotypes using genomic sequencing and other assays and randomizes between standard therapy and a personalized therapeutic approach (Fig. 6). Initially, patients with tumors of specific molecular phenotypes (that have been comprehensively determined through the APGI) are being recruited. Three subgroups with pre-defined actionable mutations will be tested initially. This trial was designed to be “adaptive” so that additional arms can be added as molecular sub-types and/or novel agents targeting these specific pathways are identified.
The three actionable mutations tested initially include
-
1.
HER2 amplified: Targeting HER2 amplified disease with trastuzumab has proven benefit in malignancies other than early and advanced breast cancer, as exemplified by the improvement in overall survival when trastuzumab was administered in HER2-positive metastatic gastric cancer [19]. Furthermore, the encouraging results observed with TDM-1 in patients with advanced breast cancer suggest that novel HER2 targeting agents may have additional benefit [20].
-
2.
DNA damage response (DDR) defective: Clinical observations have demonstrated that there are subsets of PDAC patients who are sensitive to DNA-damaging anti-cancer agents such as cisplatin and radiation: an assertion suggested by the recent demonstration of efficacy with the FOLFIRINOX regimen in metastatic PDAC [21]. DDR defects can be detected using next-generation sequencing (manuscript submitted), and are associated with response to platinums and mitomycin C.
-
3.
Anti-EGFR responsive: Small improvements in overall survival may be achieved with the addition of erlotinib to gemcitabine in combination therapy regimens in unselected patients with advanced disease [22]. By extrapolating findings from colorectal cancer, we hypothesize that patients with mutations in KRAS are unlikely to benefit from inhibition of EGFR, and therefore patients with KRAS wild-type tumors will be recruited.
The ability to forecast prognosis and predict response to a specific therapy could better stratify patients to optimal therapy without delay. This approach would improve overall outcomes and quality of life by minimizing unnecessary side effects of ineffective treatments. Furthermore, directing ongoing studies towards resistant phenotypes would facilitate the development of novel therapeutic strategies. Advances in genomic sequencing provide the potential opportunity to measure actionable genomic aberrations in parallel to facilitate the development of personalized (stratified) therapeutic strategies for cancer.
Conclusion
Novel technologies have provided significant opportunities for a deeper understanding of disease pathophysiology. Early results have indicated extensive genomic diversity, which requires novel approaches to tackle tumor heterogeneity. Purpose-built translational infrastructure and informatics systems, together with well-characterized pre-clinical models, are required to facilitate translation into clinical care.
References
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA: A Cancer J Clin. 2012;62(1):10–29. doi:10.3322/caac.20138.
Butturini G, Stocken DD, Wente MN, Jeekel H, Klinkenbijl JH, Bakkevold KE, et al. Influence of resection margins and treatment on survival in patients with pancreatic cancer: meta-analysis of randomized controlled trials. Arch Surg. 2008;143(1):75–83. doi:10.1001/archsurg.2007.17 (Discussion).
Neoptolemos JP, Stocken DD, Bassi C, Ghaneh P, Cunningham D, Goldstein D, et al. Adjuvant chemotherapy with fluorouracil plus folinic acid vs gemcitabine following pancreatic cancer resection: a randomized controlled trial. JAMA. 2010;304(10):1073–81. doi:10.1001/jama.2010.1275.
Hruban RH, Maitra A, Goggins M. Update on pancreatic intraepithelial neoplasia. Int J Clin Exp Pathol. 2008;1(4):306–16.
Samuel N, Hudson TJ. The molecular and cellular heterogeneity of pancreatic ductal adenocarcinoma. Nat Rev Gastroenterol Hepatol. 2011;. doi:10.1038/nrgastro.2011.215.
Hudson TJ, Anderson W, Artez A, Barker AD, Bell C, Bernabe RR, et al. International network of cancer genome projects. Nature. 2010;464(7291):993–8. doi:10.1038/nature08987.
Song S, Nones K, Miller D, Harliwong I, Kassahn KS, Pinese M, et al. qpure: a tool to estimate tumor cellularity from genome-wide single-nucleotide polymorphism profiles. PLoS ONE. 2012;7(9):e45835. doi:10.1371/journal.pone.0045835.
Jones S, Zhang X, Parsons DW, Lin JC, Leary RJ, Angenendt P, et al. Core signaling pathways in human pancreatic cancers revealed by global genomic analyses. Science. 2008;321(5897):1801–6. doi:10.1126/science.1164368.
Dees ND, Zhang Q, Kandoth C, Wendl MC, Schierding W, Koboldt DC, et al. MuSiC: identifying mutational significance in cancer genomes. Genome Res. 2012;22(8):1589–98. doi:10.1101/gr.134635.111.
Biankin AV, Waddell N, Kassahn KS, Gingras MC, Muthuswamy LB, Johns AL, et al. Pancreatic cancer genomes reveal aberrations in axon guidance pathway genes. Nature. 2012;491(7424):399–405. doi:10.1038/nature11547.
Roberts NJ, Jiao Y, Yu J, Kopelovich L, Petersen GM, Bondy ML, et al. ATM mutations in patients with hereditary pancreatic cancer. Cancer Discov. 2012;2(1):41–6. doi:10.1158/2159-8290.cd-11-0194.
Mermel CH, Schumacher SE, Hill B, Meyerson ML, Beroukhim R, Getz G. GISTIC2.0 facilitates sensitive and confident localization of the targets of focal somatic copy-number alteration in human cancers. Genome Biol. 2011;12(4):R41. doi:10.1186/gb-2011-12-4-r41.
Mann KM, Ward JM, Yew CC, Kovochich A, Dawson DW, Black MA, et al. Sleeping beauty mutagenesis reveals cooperating mutations and pathways in pancreatic adenocarcinoma. Proc Natl Acad Sci USA. 2012;109(16):5934–41. doi:10.1073/pnas.1202490109.
Perez-Mancera PA, Rust AG, van der Weyden L, Kristiansen G, Li A, Sarver AL, et al. The deubiquitinase USP9X suppresses pancreatic ductal adenocarcinoma. Nature. 2012;486(7402):266–70. doi:10.1038/nature11114.
Cheung HW, Cowley GS, Weir BA, Boehm JS, Rusin S, Scott JA, et al. Systematic investigation of genetic vulnerabilities across cancer cell lines reveals lineage-specific dependencies in ovarian cancer. Proc Natl Acad Sci USA. 2011;108(30):12372–7. doi:10.1073/pnas.1109363108.
Sun W, Wright FA, Tang Z, Nordgard SH, Van Loo P, Yu T, et al. Integrated study of copy number states and genotype calls using high-density SNP arrays. Nucleic Acids Res. 2009;37(16):5365–77. doi:10.1093/nar/gkp493.
Mehlen P, Delloye-Bourgeois C, Chedotal A. Novel roles for slits and netrins: axon guidance cues as anticancer targets? Nat Rev Cancer. 2011;11(3):188–97. doi:10.1038/nrc3005.
Pajic M, Scarlett CJ, Chang DK, Sutherland RL, Biankin AV. Preclinical strategies to define predictive biomarkers for therapeutically relevant cancer subtypes. Hum Genet. 2011;130(1):93–101. doi:10.1007/s00439-011-0990-0.
Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010;376(9742):687–97. doi:10.1016/s0140-6736(10)61121-x.
Blackwell K, Miles D, Gianni L. Primary results from EMILIA, a phase III study of trastuzumab emtansine (T-DM1) versus capecitabine (X) and lapatinib (L) in HER2-positive locally advanced or metastatic breast cancer (MBC) previously treated with trastuzumab (T) and a taxane. J Clin Oncol. 2012;30(18 Suppl):810.
Conroy T, Desseigne F, Ychou M, Bouche O, Guimbaud R, Becouarn Y, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364(19):1817–25. doi:10.1056/NEJMoa1011923.
Moore MJ, Goldstein D, Hamm J, Figer A, Hecht JR, Gallinger S, et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol. 2007;25(15):1960–6. doi:10.1200/JCO.2006.07.9525.
Eifert C, Powers RS. From cancer genomes to oncogenic drivers, tumour dependencies and therapeutic targets. Nat Rev Cancer. 2012;12(8):572–8. doi:10.1038/nrc3299.
Acknowledgments
We thank the members of the Australian Pancreatic Cancer Genome Initiative (APGI) for their invaluable contributions to this work. For a full list of participants, please visit http://www.pancreaticcancer.net.au/apgi/collaborators. Research Funding Support: The National Health & Medical Research Council of Australia, The Cancer Council NSW, Cancer Institute NSW, Royal Australasian College of Surgeons, St Vincent’s Clinic Foundation, R.T. Hall Trust, Avner Nahmani Pancreatic Cancer Foundation and Jane Hemstritch in memory of Philip Hemstritch.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Cowley, M.J., Chang, D.K., Pajic, M. et al. Understanding pancreatic cancer genomes. J Hepatobiliary Pancreat Sci 20, 549–556 (2013). https://doi.org/10.1007/s00534-013-0610-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00534-013-0610-6