Background/Purpose
Mortality and morbidity rates after liver resections have decreased with better surgical techniques and perioperative care. The aim of this study was to evaluate the short- and longterm results in patients who had undergone extensive hepatectomies.
Methods
From January 1985 to December 2000, 237 patients underwent 275 liver resections for colorectal metastases. Extensive liver resections were defined as follows: technical reasons (extended hepatectomies, associated vascular resections); disease extent (diameter, ≫10 cm; number, ≫5; associated extrahepatic resection). The total number of extensive liver resections was 74. There were 51 radical resections (68.9%), while in the nonextensive resections group, 152 resections were radical (90.7%; P = 0.1).
Results
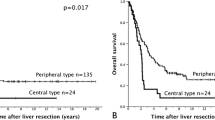
Postoperative mortality (60 days) was 1.6% (1.3% in the extensive resections group; P = 0.3), while morbidity was 22.7% (31% in the extensive resections group vs 19% in the nonextensive resections group; P = 0.1). One-, 3-, and 5-year overall actuarial survival rates were 91.8%, 44.9%, and 25.3%. The survival rates of patients who underwent an extensive resection were similar to those in the nonextensive resections group.
Conclusions
Technical difficulties and neoplastic extension are not, nowadays, a contraindication for hepatectomy for colorectal liver metastases, unless a radical resection is performed.
Similar content being viewed by others
Author information
Authors and Affiliations
About this article
Cite this article
Ferrero, A., Polastri, R., Muratore, A. et al. Extensive resections for colorectal liver metastases. J Hepatobiliary Pancreat Surg 11, 92–96 (2004). https://doi.org/10.1007/s00534-002-0792-9
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s00534-002-0792-9