Abstract
Purpose
Head and neck cancer (HNC) will be diagnosed in approximately 54,000 Americans in 2022 with more than 11,000 dying as a result. The treatment of HNC often involves aggressive multimodal therapy including surgery, radiotherapy, and systemic therapy. HNC and its treatments are associated with multiple painful and function-limiting neuromusculoskeletal and visceral long-term and late effects. Among these is head and neck lymphedema (HNL), the abnormal accumulation of protein rich fluid, in as many as 90% of survivors. Though HNL is common and potentially contributory to other function-limiting issues in this population, it is notoriously understudied, underrecognized, underdiagnosed, and undertreated. This study seeks to determine the incidence of HNC-related lymphedema diagnosis and treatment in a large US healthcare claims repository database.
Methods
A retrospective observational cohort design and data from an integrated US healthcare claims repository—the IBM MarketScan Commercial Claims and Encounters (CCAE) and Medicare Supplemental and Coordination of Benefits (MDCR) Databases spanning the period April 1, 2012 through March 31, 2020.
Results
Of the 16,654 HNC patients eligible for evaluation, 1,082 (6.5%) with a diagnosis of lymphedema were identified based on eligibility criteria. Of the 521 HNC patients evaluated for lymphedema treatment, 417 (80.0%) patients received 1.5 courses of MLD, 71 (13.6%) patients were prescribed compression garments, and 45 (8.6%) patients received an advanced pneumatic compression device.
Conclusion
HNL in this population of HNC survivors was underdiagnosed and treated compared with contemporary assessments HNL incidence.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
The American Cancer Society estimates that 54,000 Americans will develop head and neck cancer (HNC) in 2022 and more than 11,000 will die as a result [1]. Aggressive, multi-modal therapy is the mainstay of treatment for patients with locally advanced disease. Such treatments, though potentially curative, often come at the price of severe, painful, function- and quality of life-limiting acute and late effects [2]. The epidemic of human papilloma virus (HPV)-associated HNC, a disease that is generally more curable, but also most prevalent in younger individuals, has shifted the burden of HNC-related impairments to a younger cohort [3]. Improved treatment outcomes coupled with this changing epidemiology will result in many more HNC survivors destined to live their lives, often from a relatively young age, with the late effects of HNC and its treatment [4, 5].
Lymphedema is characterized by several pathophysiological events, including lymph stasis, lymphatic vessel remodeling and dysfunction, inflammation, adipose tissue deposition, and ultimately fibrosis [6]. Head and neck lymphedema (HNL), a common complication of HNC, results from treatments such as neck dissection and/or radiation. HNL can progress and cause chronic inflammatory, fibrosclerotic and fibrofatty deposition resulting in permanent deformity and disability [7, 8]. The reported prevalence of lymphedema in HNC survivors ranges from 12% to more than 90% [8,9,10,11,12]. This variation is due to methodological differences between studies with contemporary studies favoring the high range of prevalence. [8, 12]
HNL is not simply a cosmetic issue. It is both an external and internal phenomenon with significant clinical sequelae [13, 14]. Ongoing fibrosis and inflammation associated with HNL are likely to contribute to progression of associated late effects [5, 8, 15]. Functional sequelae associated with HNL include skin changes, pain, range of motion limitations, contracture, dysphagia, dysarthria, dyspnea, postural abnormalities, trismus, and reduced quality of life among other issues [5, 8, 14, 16,17,18,19]. Progression of HNL and fibrosis is associated with increasing symptom burden, functional impairment, and reduced quality of life [5, 17]. There is growing evidence in the breast cancer literature that early recognition and effective treatment of breast cancer-related lymphedema improves outcomes [20, 21]. Though less robust, evidence also suggests that the early identification and effective treatment of HNL may improve functional outcomes including dyspnea, pain, and dysphagia in HNC survivors [22, 23].
Despite a prevalence of more than 90% in HNC survivors and the potential benefits of early and effective treatment, HNL is understudied, underrecognized, underdiagnosed, and undertreated [8, 9, 13]. The magnitude of this deficiency has not been well defined. This study seeks to determine the incidence of HNC-related lymphedema diagnosis and treatment in a large US healthcare claims repository database.
Methods
Study design and data source
A retrospective observational cohort design and data from an integrated US healthcare claims repository—the IBM MarketScan Commercial Claims and Encounters (CCAE) and Medicare Supplemental and Coordination of Benefits (MDCR) Databases—were employed. For this study, data spanned the period April 1, 2012 through March 31, 2020.
The CCAE Database includes healthcare claims and enrollment information from employer-sponsored plans throughout the US that provide health benefits to working persons aged < 65 years annually, including the employees, their spouses, and their dependents. The MDCR Database includes healthcare claims and enrollment information for retirees who are Medicare-eligible and have elected to enroll in employer-sponsored Medicare supplemental plans (and for which both the Medicare-paid amounts and employer-paid amounts are available).
Healthcare claims include medical (i.e., facility and professional service) and outpatient pharmacy claims. Data available for each facility and professional service claim include the dates and places of service, diagnoses, procedures performed/services rendered, and quantity of services (professional-service claims). Data available for each outpatient pharmacy claim include the drug dispensed, dispensing date, dose, quantity dispensed, and number of therapy days supplied. Medical and pharmacy claims also include amounts paid (i.e., reimbursed) by health plans and patients to healthcare providers for services rendered. Selected demographic and eligibility information also is available. Patient-level data can be arrayed chronologically to provide a detailed longitudinal profile of all medical and pharmacy services used by each plan member.
Study population
Two populations of patients were identified from this dataset – those with HNC-related lymphedema and those who received treatment for HNC-related lymphedema.
HNC incidence
For analyses of HNC incidence, the study population comprised patients aged ≥ 18 years who had first evidence of HNC between April 1, 2013 and March 31, 2019, and who received treatment for this condition during the 3-month period following the initial diagnosis. Evidence of HNC was ascertained based on ≥ 1 diagnosis code in the acute-care hospital (inpatient) setting, or ≥ 2 diagnosis codes—at least seven days apart—in the ambulatory (outpatient) setting; evidence of HNC treatment was ascertained based on corresponding procedure codes (Appendix). Patients were excluded from the study population if they were not continuously enrolled during the 1-year period preceding, and during the 1-year period following, first evidence of HNC, or if they had evidence of lymphedema or other etiologies for lymphedema (e.g., other cancers, venous leg ulcers, chronic venous insufficiency) prior to the initial HNC diagnosis.
HNC-related lymphedema incidence
For analyses of HNC-related lymphedema incidence, the study population comprised patients aged ≥ 18 years who had first evidence of lymphedema between April 1, 2013 and March 31, 2019, and who had evidence of HNC—as well as cancer-related treatment—during the 1-year period preceding the initial diagnosis of lymphedema. Evidence of lymphedema (primary/secondary) was ascertained based on ≥ 1 diagnosis code for lymphedema in the acute-care hospital (inpatient) setting, or ≥ 2 diagnosis codes for lymphedema—at least seven days apart—in the ambulatory (outpatient) setting (Appendix). Patients were excluded from the study population if they were not continuously enrolled during the 1-year period preceding, and during the 1-year period following, first evidence of lymphedema, or if they had evidence of other etiologies for lymphedema (e.g., other cancers, venous leg ulcers, chronic venous insufficiency).
Baseline characteristics
Baseline characteristics of lymphedema patients with head/neck cancer were ascertained during the 1-year period prior to the initial diagnosis of lymphedema, and included: demographic profile (age, sex); clinical profile (lymphedema-related conditions, comorbidities); and cancer treatment profile (chemotherapy, radiation, surgery). Lymphedema-related conditions and comorbidities were identified based on encounters with a corresponding diagnosis code. Operational algorithms and codes used to ascertain baseline characteristics are set forth in the Appendix.
HNC-related lymphedema treatment incidence
Use of lymphedema treatment among HNC patients was ascertained during the 1-year period following first evidence of lymphedema. Treatments included conservative (CONS) therapy (manual lymphatic drainage [MLD], compression garments [CG]) and advanced pneumatic compressions devices (APCD).
Each unique treatment course was identified, beginning with the first, and all qualifying encounters (i.e., with the same Current Procedural Terminology [CPT] or Healthcare Common Procedure Coding System [HCPCS] code) occurring within 30 days of each other was deemed to be part of the same treatment course.
Results
Patient demographics and baseline characteristics are detailed in Table 1.
HNC incidence
81,963 patients aged ≥18 years who had first evidence of HNC between April 1, 2013 and March 31, 2019 were identified. Of these, 26,904 were continuously enrolled during the 1-year period preceding and 1-year period following first evidence of HNC and 16,654 received HNC treatment during the 3-month period following their first HNC diagnosis.
HNC-related lymphedema incidence
Of the 16,654 HNC patients eligible for evaluation, 1,082 (6.5%) with a diagnosis of lymphedema were identified based on the criteria detailed above.
Baseline characteristics
The patient population of patients with HNC-related lymphedema is primarily comprised of men (76.8%) with an average age of 58.0 years. Most frequently noted comorbidities included hypertension (50.9%), depression (31.1%), diabetes (15.5%), and renal disease (11.5%). Cancer therapy included radiation (67.2%), chemotherapy (63.3%), and surgery (46.3%).
HNC-related lymphedema treatment incidence
123,236 patients aged ≥18 years who had first evidence of lymphedema between April 1, 2013 and March 31, 2019 were identified. Of these, 61,890 were continuously enrolled during the 1-year period preceding and 1-year period following first evidence of lymphedema. 521 (0.84%) of the patients had evidence of HNC within one year prior their first documented evaluation for lymphedema treatment.
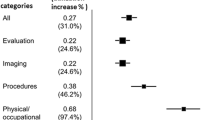
The details of lymphedema treatment are detailed in Table 2. Of the 521 HNC patients evaluated for lymphedema treatment, 417 (80.0%) patients received 1.5 courses of MLD. 71 (13.6%) patients were prescribed compression garments, and 45 (8.6%) patients received an APCD.
Discussion
Only 6.5% of the 16,654 HNC survivors in this cohort were diagnosed with lymphedema. This is just over half of the historically reported low range of 12% and a small fraction of the incidence of 90% reported in contemporary studies [8,9,10,11,12]. Our database only identified 521 HNC survivors who received treatment for lymphedema suggesting marked undertreatment of the disorder. The primary treatment modality for those referred was MLD (80%) with only a small percentage receiving compassion garments (13.6%) and even fewer (8.6%) receiving APCD.
Under recognition, underdiagnosis, and undertreatment of HNL has potentially profound implications at many levels. Like radiation fibrosis syndrome (RFS), lymphedema is a progressive process associated with protein deposition, fibrosis and sclerosis [5, 8, 24]. Unlike RFS, the protein deposition and fibrosis resulting from lymphedema may be mitigated, at least to some degree, by effective lymphedema therapies such as MLD, compression and APCD utilization [25,26,27,28,29]. This raises the possibility that not identifying and addressing HNL may contribute to progression of fibrosis-related issues by superimposing lymphedema-related fibrosis on top of radiation-related fibrosis. Early evidence suggests APCD has positive benefits for lymphedema control, neck pain, dysphagia, and dyspnea [29]. At the population level, addressing lymphedema in HNC survivors may hold the potential for reduced cost of care to payers and reduced burden of care on oncology clinicians.
HNL is understudied, underrecognized, underdiagnosed, and undertreated despite a growing body of evidence that successfully addressing it in HNC survivors may confer a multitude of benefits. Clinicians involved in the care of HNC patients should familiarize themselves with the epidemiology, diagnostic features, and principles of treating HNL. In addition to traditional MLD, newer tools such APCD may facilitate treatment of HNL and mitigate associated sequelae.
Change history
15 May 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00520-023-07809-0
References
Cancer Facts and Figures (2022) https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2022/2022-cancer-facts-and-figures.pdf. Accessed 26 Jul 2022
Murphy BA, Gilbert J, Ridner SH (2007) Systemic and global toxicities of head and neck treatment. Expert Rev Anticancer Ther 7:1043–1053
Lechner M, Liu J, Masterson L, Fenton TR (2022) HPV-associated oropharyngeal cancer: epidemiology, molecular biology and clinical management. Nat Rev Clin Oncol 19:306–327
Cohen EE, LaMonte SJ, Erb NL et al (2016) American cancer society head and neck cancer survivorship care guideline. CA Cancer J Clin 66:203–239
Parke SC, Langelier DM, Cheng JT, Kline-Quiroz C, Stubblefield MD (2022) State of rehabilitation research in the head and neck cancer population: Functional impact vs. impairment-focused outcomes. Curr Oncol Rep 24:517–532
Azhar SH, Lim HY, Tan BK, Angeli V (2020) The unresolved pathophysiology of lymphedema. Front Physiol 11:137
Cucchi F, Rossmeislova L, Simonsen L, Jensen MR, Bülow J (2017) A vicious circle in chronic lymphoedema pathophysiology? An adipocentric view. Obes Rev 18:1159–1169
Ridner SH, Dietrich MS, Niermann K, Cmelak A, Mannion K, Murphy B (2016) A prospective study of the lymphedema and fibrosis continuum in patients with head and neck cancer. Lymphat Res Biol 14:198–205
Deng J, Ridner SH, Dietrich MS et al (2012) Prevalence of secondary lymphedema in patients with head and neck cancer. J Pain Symptom Manage 43:244–252
Jeans C, Brown B, Ward EC et al (2020) Comparing the prevalence, location, and severity of head and neck lymphedema after postoperative radiotherapy for oral cavity cancers and definitive chemoradiotherapy for oropharyngeal, laryngeal, and hypopharyngeal cancers. Head Neck 42:3364–3374
Tribius S, Pazdyka H, Tennstedt P et al (2020) Prognostic factors for lymphedema in patients with locally advanced head and neck cancer after combined radio(chemo)therapy- results of a longitudinal study. Oral Oncol 109:104856
Fadhil M, Singh R, Havas T, Jacobson I (2022) Systematic review of head and neck lymphedema assessment. Head Neck 44(10):2301–2315
Deng J, Ridner SH, Murphy BA (2011) Lymphedema in patients with head and neck cancer. Oncol Nurs Forum 38:E1–E10
Murphy BA, Gilbert J (2009) Dysphagia in head and neck cancer patients treated with radiation: assessment, sequelae, and rehabilitation. Semin Radiat Oncol 19:35–42
Stubblefield MD (2017) Clinical evaluation and management of radiation fibrosis syndrome. Phys Med Rehabil Clin N Am 28:89–100
Smith BG, Lewin JS (2010) Lymphedema management in head and neck cancer. Curr Opin Otolaryngol Head Neck Surg 18:153–158
Deng J, Murphy BA, Dietrich MS et al (2013) Impact of secondary lymphedema after head and neck cancer treatment on symptoms, functional status, and quality of life. Head Neck 35:1026–1035
Stubblefield MD (2018) Cancer rehabilitation - principles and practice, 2nd edn. Demos Medical, New York
Jeans C, Ward EC, Cartmill B et al (2019) Patient perceptions of living with head and neck lymphoedema and the impacts to swallowing, voice and speech function. Eur J Cancer Care (Engl) 28:e12894
Shah C, Arthur DW, Wazer D, Khan A, Ridner S, Vicini F (2016) The impact of early detection and intervention of breast cancer-related lymphedema: a systematic review. Cancer Med 5:1154–1162
Stout Gergich NL, Pfalzer LA, McGarvey C, Springer B, Gerber LH, Soballe P (2008) Preoperative assessment enables the early diagnosis and successful treatment of lymphedema. Cancer 112:2809–2819
Gutiérrez C, Mayrovitz HN, Naqvi SHS, Karni RJ (2020) Longitudinal effects of a novel advanced pneumatic compression device on patient-reported outcomes in the management of cancer-related head and neck lymphedema: A preliminary report. Head Neck 42:1791–1799
Ridner SH, Dietrich MS, Cowher MS et al (2019) A randomized trial evaluating bioimpedance spectroscopy versus tape measurement for the prevention of lymphedema following treatment for breast cancer: Interim analysis. Ann Surg Oncol 26:3250–3259
Donahue MJ, Donahue PCM, Rane S et al (2016) Assessment of lymphatic impairment and interstitial protein accumulation in patients with breast cancer treatment-related lymphedema using CEST MRI. Magn Reson Med 75:345–355
Blom KY, Johansson KI, Nilsson-Wikmar LB, Brogårdh CB (2022) Early intervention with compression garments prevents progression in mild breast cancer-related arm lymphedema: a randomized controlled trial. Acta Oncol 61:897–905
Leduc O, Leduc A, Bourgeois P, Belgrado JP (1998) The physical treatment of upper limb edema. Cancer 83:2835–2839
Deng J, Wulff-Burchfield EM, Murphy BA (2019) Late soft tissue complications of head and neck cancer therapy: lymphedema and fibrosis. JNCI Monographs 2019(53):lgz005
Gutierrez C, Karni RJ, Naqvi S et al (2019) Head and neck lymphedema: treatment response to single and multiple sessions of advanced pneumatic compression therapy. Otolaryngol Head Neck Surg 160:622–626
Gutiérrez C, Mayrovitz HN, Naqvi SHS, Karni RJ (2020) Longitudinal effects of a novel advanced pneumatic compression device on patient‐reported outcomes in the management of cancer‐related head and neck lymphedema: A preliminary report. Head Neck 42(8):1791–1799
Acknowledgements
Thanks to Sarah Yonak and Michelle Wetherby for their invaluable assistance with this manuscript.
Funding
Tactile Medical (Minneapolis, MN).
Author information
Authors and Affiliations
Contributions
MS conceptualization, writing, review, and editing. DW data analysis.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was not required for this study.
Competing interests
Michael Stubblefield is a consultant to Tactile Medical.
Derek Weycker received consultative reimbursement from Tactile Medical for his independent performance of the health economic analysis.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to a retrospective Open Access order.
Appendix
Appendix
This data extract includes all healthcare claims and enrollment information for all patients with any evidence of the following conditions or procedures from January 2012 through December 2019 (the “study period”):
-
≥ 1 diagnosis code (irrespective of care setting) for lymphedema (ICD-9: 457.0, 457.1, 757.0; ICD-10: I97.2, I89.0, Q82.0);
-
≥ 1 diagnosis code (irrespective of care setting) for edema (ICD-9: 782.3; ICD-10: R60.x);
-
≥ 1 procedure code (irrespective of care setting) for pneumatic compressor segmental home model without calibrated gradient pressure (E0651) or pneumatic compressor segmental home model with calibrated gradient pressure (E0652);
-
≥ 1 diagnosis code (irrespective of care setting) for head/neck cancer (ICD-9: 140.x-149.x, 160.x, 161.x, 162.0, 170.0–170.1, 176.2, 195.0; ICD-10: C00.x-C14.x, C30.x-C46.x, C76.0); or
-
≥ 1 diagnosis code (irrespective of care setting) for:
-
Venous ulcer/venous insufficiency (ICD-9: 459.81; ICD-10: I87.2)
-
Varicose veins (ICD-9: 454.x; ICD-10: I83.xxx)
-
Ulcer of lower limbs (ICD-9: 707.1x; ICD-10: L97.xxx)
-
Chronic venous hypertension with ulcer/inflammation (ICD-9: 459.3x; ICD-10: I87.3x)
-
Post-thrombotic syndrome (ICD-9: 459.1x; ICD-10: I87.0xx)
-
Iliocaval venous obstruction (ICD-9: 459.2; ICD-10: I87.1)
-
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Stubblefield, M.D., Weycker, D. Under recognition and treatment of lymphedema in head and neck cancer survivors – a database study. Support Care Cancer 31, 229 (2023). https://doi.org/10.1007/s00520-023-07698-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07698-3