Abstract
Aim
To evaluate a web-based tool for estimating and explaining three scenarios for expected survival time to people with advanced cancer (patients), their family members (FMs), and other healthcare professionals (HCPs).
Methods
Thirty-three oncologists estimated the “median survival of a group of similar patients” for patients seeking quantitative prognostic information. The web-based tool generated worst-case, most likely, and best-case scenarios for survival based on the oncologist’s estimate. Oncologists presented the scenarios to each patient and provided a printed summary to patients, FMs, and HCPs. Attitudes to the information were assessed by questionnaires. Observed survival for each patient was compared with the oncologist’s estimated survival and the three scenarios.
Results
Prognosis was discussed with 222 patients: median age 67 years; 61% male; most common primary sites pancreas 15%, non-small-cell lung 15%, and colorectal 12%. The median (range) for observed survival times was 9 months (0.5–43) and for oncologist’s estimated survival times was 12 months (2–96). Ninety-one percent of patients, 91% of FMs, and 84% of HCPs agreed that it was helpful having life expectancy explained as three scenarios. The majority (77%) of patients judged the information presented about their life expectancy to be the same or better than they had expected before the consultation. The survival estimates met a priori criteria for calibration, precision, and accuracy.
Conclusions
Patients, FMs, and HCPs found it helpful to receive personalized prognostic information formatted as three scenarios for survival. It was feasible, acceptable, and safe to use a web-based resource to do this.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Conversations about prognosis are important for people affected by incurable cancer and help patients and their families make decisions about treatment, plans for the future, and choices about end-of-life care. Patients who have a good understanding of their life expectancy are less likely to choose futile treatments and aggressive medical interventions toward the end of life; are more likely to accept palliative care services earlier; have better quality of life at the end of life; and have surviving carers with better quality of life during the bereavement period [1,2,3].
Despite this, many oncologists provide patients with minimal information about life expectancy or avoid such discussions altogether [4,5,6]. Reported reasons for this include fear of upsetting patients, fear of providing inaccurate information, and insufficient training in prognostication [7, 8]. As a consequence, many patients do not fully understand their situation and goals of treatment. Conversations about prognosis are often deferred until the last months of life, robbing patients and families the opportunity to plan and discuss their wishes while they are well. When conversations about prognosis do occur, they are rarely documented in the patient’s medical record or letters to other healthcare professionals [9, 10]. This makes it difficult for all healthcare professionals involved in the patient’s care to know what has been discussed and may result in patients receiving inconsistent information.
Most patients want some information about their expected survival time, and many want information about specific scenarios, for example, the longest survival with treatment, average survival, and shortest survival without treatment [11,12,13]. We previously surveyed 505 people with a cancer experience about their preferred format for presenting information on expected survival time to a hypothetical patient with advanced cancer and found that 88% preferred three scenarios for survival (worst-case, most likely, and best-case), and only 5% preferred a single estimate of the median survival time [14].
In previous work, we showed that certain percentiles of an overall survival (OS) curve provide a useful basis for estimating three scenarios for survival [15]. For example, the 90th percentile, the time when 90% of people are still alive and 10% have died, can approximate the worst-case scenario (shortest 10% of survival times) and the 10th percentile, the time when 10% of people are still alive and 90% have died, can approximate the best-case scenario (longest 10% of survival times). We have also shown that simple multiples (0.25, 0.5, 2, and 3) of an OS curve’s median can be used to estimate its percentiles [15,16,17,18,19,20,21,22,23]. To illustrate, the 90th percentile (representing the upper bound of the worst-case scenario) is approximately one-quarter of the median OS; the 75th percentile (lower bound of the most likely scenario) is approximately half the median OS; the 25th percentile (upper bound of the most likely scenario) is approximately double the median OS; and the 10 percentile (lower bound of the best-case scenario) is approximately three times the median OS. For example, if the median OS is 12 months then the worst-case scenario is less than 3 months (0.25 x 12), the most likely scenario is 6 to 24 months (0.5 to 2 x 12), and the best-case scenario is 36 months or longer (3 x 12).
Using these simple rules of thumb, we developed a web-based tool (iTool) to help oncologists estimate and explain individualized scenarios for survival to patients with incurable cancer seeking quantitative information about their prognosis. With consumer input, we developed a one-page summary to help explain this information to patients, family members or carers (FMs), and other healthcare professionals (HCPs).
The aim of this study was to evaluate the iTool for estimating and explaining personalized information about life expectancy in people with advanced cancer, their medical oncologists, FMs, and other HCPs.
Patients and methods
We conducted a multi-site, single-arm, phase 2 trial. The target population was adults with incurable cancer attending the clinic of a participating medical oncologist and indicating that they wanted quantitative information about their prognosis (either spontaneously or when their oncologist offered to discuss prognosis). FMs were eligible if present during the consultation when life expectancy was discussed. HCPs involved in a participating patient’s care and receiving letters from the oncologist as standard of care (e.g., general practitioner, referring surgeon, radiation oncologist) were also invited to participate.
Participating oncologists were provided with access to the iTool for the duration of the study (available at https://ctc.usyd.edu.au/3scenarios/). When a patient wanted information on their expected survival time, we asked the oncologist to estimate the patient’s life expectancy defined as “the median survival of a group of similar patients” based on studies of patients in the same situation, prognostic tools, or their personal clinical experience. The iTool calculated ranges for the three scenarios using simple multiples of the oncologist’s estimate based on our previous work [16]. This information was printed for the patient and FMs to take home (Supplementary Text 1), and copies were placed in the patient’s medical record and sent to HCPs with the oncologist’s standard letter.
Following the consultation, the oncologist entered the patient demographics and cancer details and completed a questionnaire about the perceived usefulness of the iTool for that patient, including if it was helpful, easy to use, stressful, or lengthened the consultation (Supplementary Text 2). After providing written, informed consent, patients completed a questionnaire about the prognostic information they received (Supplementary Text 3). FMs and HCPs completed similar questionnaires regarding the information they received (Supplementary Text 4 and 5). The study was approved by the health research ethics committee at all participating sites.
The primary measure of effect was the proportion of patients who agreed or strongly agreed that “having my life expectancy explained this way was helpful.” Other measures of effect included the proportions of patients who agreed or strongly agreed that “Having my life expectancy explained this way”: made sense, gave hope, or made them feel worried or anxious. Patients were asked if the information about their life expectancy was better, worse, or about the same as they had thought before the consultation. Patients were also asked if they agreed it was helpful to be told each of the scenarios (best-case, worst-case, and most likely).
Patients also completed three other questionnaires:
-
1.
The Short State Trait Anxiety Inventory (STAI), a six-item short form of the state scale of the Spielberger STAI [24]
-
2.
The Herth Hope Index, a 12-item adapted version of the Herth Hope Scale with three subscales measuring temporality and future, positive readiness and expectancy, and interconnectedness [25]
-
3.
The Life Orientation Test Revised (LOTR), a 10-item scale measuring levels of optimism [26]
A higher score indicated greater levels of either anxiety, hope, or optimism with each scale, respectively.
At the end of the study, participating oncologists completed a second questionnaire to determine their attitudes to using the iTool when discussing prognosis with their patients (Supplementary Text 6). Oncologists were sent emails asking them to update the survival status of each patient at time points corresponding to simple multiples of their estimated median survival time: 0.25, 0.5, 1.0, 2.0, 3.3, and 5.
For comparability with previous studies, we defined a point estimate of life expectancy (estimated median survival time of a group of similar patients) as precise if it was within 0.67 to 1.33 times the observed survival time [15] and hypothesized that approximately 20% to 30% of estimates would meet this definition. For each patient, we calculated the ratio of the observed survival time (OST) to their oncologist’s estimated survival time (EST) and used the Kaplan–Meier distribution of the ratio (OST/EST) to account for censored observations (patients still alive at their last follow-up). We expected oncologists’ EST to be well-calibrated (i.e., approximately equal proportions (50%) being longer than the observed survival time (OST/EST < 1) and shorter than the observed survival time (OST/EST > 1)).
Based on the broad concept of accuracy used in our previous work, we also hypothesized that approximately:
Five to ten percent of patients would die within one-quarter of their oncologists’ estimate (OST/EST ≤ 0.25).
Fifty percent of patients would have a survival time within half to double their oncologists’ estimate (0.5 ≤ OST/EST ≤ 2).
Ten percent of patients would live beyond three times their oncologist’s estimate (OST/EST ≥ 3) [20].
A sample of size of at least 70 patients was calculated to provide > 95% power to distinguish the observed proportion of patients finding the iTool helpful from hypothetical true proportions of 80% or more versus 60% or less with an allowance of 20% for incomplete data. Associations between baseline characteristics and responses to questions about the prognostic information were assessed with logistic regression. Statistical analyses were done using R version 4.0.4.
Results
Between August 2012 and May 2016, 33 oncologists used the iTool to explain life expectancy to 222 patients (Fig. 1), of whom 201 consented to participate in the evaluation part of the study and 146 returned completed questionnaires (response rate 73%). Completed questionnaires were returned by 102 FMs and 140 HCPs. All 33 participating oncologists completed a questionnaire following each patient consultation (oncologist questionnaire 1), and 21 of the 33 oncologists completed a questionnaire at the end of the study (oncologist questionnaire 2).
The baseline characteristics of participating patients are summarized in Table 1. The median age was 67 years, and the majority (61%) were male. For most patients, the iTool was used more than 8 weeks after their diagnosis of incurable cancer, and at a third or subsequent consultation. The median estimated survival time was 12 months (range 2 to 96 months).
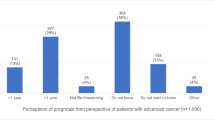
The vast majority (91%) of patients agreed or strongly agreed that the survival information presented by the iTool was helpful (Table 2). More patients preferred to hear each of the three scenarios (worst-case 81%, most likely 86%, and best-case 92%) than to be told the estimated median survival (78%). Seventy-seven percent of patients responded that the information about their prognosis explained as three scenarios for survival was about the same as, or better than, they expected before discussing it with their oncologist.
The attitudes of oncologists, HCPs, and FMs to having the information estimated and explained this way are summarized in Table 3. The median number of times each oncologist used the iTool was four (range 1 to 50). In 96% of consultations, oncologists agreed or strongly agreed that explaining life expectancy as three scenarios was helpful. There were very few consultations where oncologists agreed or strongly agreed that using the iTool significantly lengthened the consultation (9%). The majority of HCPs agreed or strongly agreed that having the information presented this way would be helpful for themselves (84%) and their patients (73%) and was more informative than the prognostic information they usually received (88%).
Associations between patients’ baseline characteristics and agreeing or strongly agreeing that presenting the life expectancy information as three scenarios was helpful are summarized in Table 4. Higher scores for hope were associated with a higher likelihood of agreeing that the information was helpful (OR 5.7, 95% CI 1.2 to 27, p = 0.03).
The median observed survival time was 9 months (range 0.5 to 43). Oncologists’ estimates were well-calibrated, with 54% (95% CI 46 to 61) of patients living longer than their EST and 46% (95% CI 39 to 54) living shorter than their EST. As hypothesized, 27% (95% CI 20 to 34) of oncologists’ point estimates of life expectancy met our arbitrary criterion for precision (within 0.67–1.33 times the OST). The proportions of patients with OSTs falling within prespecified ranges for the three scenarios corresponded closely with our a priori hypotheses: 7% (95% CI 3 to 10) of patients died within their estimated worst-case scenario; 51% (95% CI 43 to 59) lived within their estimated most likely scenario; and 13% (95% CI 8 to 23) lived within their estimated best-case scenario. Figure 2 shows the distribution of the OST/EST ratio for each patient.
At the end of the study, 81% (17/21) of responding oncologists agreed or strongly agreed that the iTool made discussing prognosis easier; 52% (11/21) agreed or strongly agreed that it made them more prepared to discuss prognosis; and 86% (18/21) agreed or strongly agreed that they would like to continue using the iTool beyond the study.
Discussion
The majority of responding patients, FMs, and HCPs found it helpful to receive personalized scenarios for survival generated by the iTool. While 40% of patients found the life expectancy information upsetting, the majority of patients and FMs still found it helpful to be told each of the three scenarios, including the worst-case scenario. Most responding patients (77%) reported that the life expectancy information they received was the same or better than they had expected before the consultation. A higher score for hope was associated with higher likelihood of responding that the survival information was helpful. As hypothesized, oncologists’ point estimates of life expectancy for individual patients were well-calibrated but imprecise. However, scenarios for survival time calculated by the iTool using simple multiples of the oncologists’ estimates corresponded closely with our a priori estimates: approximately 10% of patients died within one quarter of their EST, approximately 50% lived within half to double their EST, and approximately 10% lived longer than three times their EST [16].
These favorable attitudes to using the iTool were consistent with our previous findings that people with cancer prefer to receive prognostic information formatted as three scenarios (worst-case, most-likely, best-case) rather than a point estimate of the median survival time [14]. Our previous work involved a hypothetical patient so it was reassuring to find similar results when real patients were presented with a personalized estimate of their own prognosis in this format. Participating oncologists reported that the iTool was easy to use and made them better prepared to discuss prognosis.
Our data indicate that the iTool could help overcome commonly cited barriers to discussions about prognosis including: lack of tools, lack of time, not knowing what to say, and fear of upsetting patients and family members [8, 20, 21]. Oncologists reported that using the iTool prolonged less than 10% of consultations, an important finding given fear of prolonging consultations is a reported barrier to discussing prognosis [8, 27].
Most patients found it helpful to receive a printed summary of information about their prognosis. Similarly, more than 70% of HCPs agreed that the printed three scenarios for survival information they received was more informative than the prognostic information they usually receive from oncologists, and that this information would help them make management and treatment decisions with their patients. We previously reported that quantitative information about prognosis was rarely included in letters from medical oncologists to HCPs [9]. Providing the one-page printed summary to HCPs could help ensure members of the multidisciplinary care team are aware of the estimated prognosis, and of what the patient has been told. This should improve the consistency of information and perhaps even improve patient care.
Fear of upsetting the patient is a commonly reported barrier to discussing prognosis [8]. Interestingly, oncologists in this study agreed that patients would find the prognostic information upsetting in only 16% of consultations. This may be because they perceived the format of presenting three scenarios was less upsetting or perhaps that the patients they selected for the study were those less likely to be upset by the information. We found 40% of patients agreed that the prognostic information they received was upsetting, yet despite this, over 90% agreed that the information was helpful. We previously reported that providing patients with ranges for three scenarios was judged to offer more hope than providing a single point estimate of survival [14]. It is possible that providing ranges for three scenarios helps patients understand the uncertainty of survival estimates and allows them to hope for a realistic best-case scenario. Most patients found that the information presented about their life expectancy was either about the same as, or better than, they expected, even when given their worst-case scenario. Previous studies reporting that patients with advanced cancer are more likely to over-estimate their survival compared to their oncologists have generally compared a point estimate made by the patient with a point estimate made by the oncologist [2, 21, 28]. Another possible explanation is that the majority of patients in our study (59%) received their survival time scenarios at a third or subsequent consultation, and there may have been other, earlier discussions about prognosis.
This study and approach to discussing prognosis has several key strengths. We developed an easily accessible, web-based tool designed to help oncologists explain “worst-case, most likely, and best-case scenarios for survival time” to people affected by cancer. We studied the attitudes of patients receiving personalized information about their own life expectancy and also the attitudes of oncologists, FMs, and HCPs. We included patients with a wide range of ages, cancer types, and estimated life expectancies. This supports the applicability of the iTool in people with advanced cancer seeking quantitative information about their prognosis from receptive oncologists. Our data support the accuracy of scenarios for survival time based on simple multiples of their oncologist’s estimate of life expectancy.
The main limitations of this study are the biases inherent to a single-arm design. Participating oncologists may have had greater interest and expertise in discussing prognosis and may have selected patients they judged likely to welcome information presented this way. Our response rate for patient questionnaires was 73%; the 55 consenting patients who did not return a questionnaire may have had less favorable views. We did not assess patients’ understanding of the information presented about their prognosis. Our study involved only 33 oncologists. The generalizability of these findings requires further study, especially in the current era of increasing use of immunotherapy.
Future directions
Changing the behavior and practice of doctors is difficult. Australia has mandatory workshops on communicating prognosis for advanced trainees in medical oncology. Incorporating the iTool into this training offers an opportunity to increase its use. The www.cancersurvivalrates.com website is another useful resource for oncologists and people affected by cancer who seek quantitative information about prognosis. This website provides information based on recent data collected by the US SEER program and now provides information presented as three scenarios when the estimated median survival time is less than 3 years. These resources can help start and facilitate conversations about prognosis between patients and their doctors. Further research is needed to evaluate patients’ understanding of presented information about prognosis.
Conclusion
We have provided strong evidence supporting the recommendation that oncologists use three scenarios for survival time when thinking and talking about prognosis in advanced cancer. It was feasible, acceptable, helpful, and safe to use a web-based resource to do this.
Our web-based tool can be accessed via the link https://ctc.usyd.edu.au/3scenarios/
Data availability
The authors have full control of all primary data and agree to allow the journal to review their data if requested.
Code availability
Not applicable.
Change history
27 May 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00520-024-08597-x
References
Eidinger RN, Schapira DV (1984) Cancer patients’ insight into their treatment, prognosis, and unconventional therapies. Cancer 53(12):2736–2740
Weeks JC, Cook EF, O’Day SJ et al (1998) Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA 279(21):1709–1714. https://doi.org/10.1001/jama.279.21.1709
Wright AA, Zhang B, Ray A et al (2008) Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 300(14):1665–1673. https://doi.org/10.1001/jama.300.14.1665
Gordon EJ, Daugherty CK (2003) ‘Hitting you over the head’: oncologists’ disclosure of prognosis to advanced cancer patients. Bioethics 17(2):142–168
Helft PR (2005) Necessary collusion: prognostic communication with advanced cancer patients. J Clin Oncol 23(13):3146–3150. https://doi.org/10.1200/JCO.2005.07.003
Baile WF, Lenzi R, Parker PA, Buckman R, Cohen L (2002) Oncologists’ attitudes toward and practices in giving bad news: an exploratory study. J Clin Oncol 20(8):2189–2196. https://doi.org/10.1200/JCO.2002.08.004
Hancock K, Clayton JM, Parker SM et al (2007) Truth-telling in discussing prognosis in advanced life-limiting illnesses: a systematic review. Palliat Med 21(6):507–517. https://doi.org/10.1177/0269216307080823
Vasista A, Stockler MR, Martin A, Lawrence NJ, Kiely BE (2020) Communicating prognostic information: what do oncologists think patients with incurable cancer should be told? Intern Med J 50(12):1492–1499. https://doi.org/10.1111/imj.14739
McConnell D, Butow PN, Tattersall MH (1999) Improving the letters we write: an exploration of doctor-doctor communication in cancer care. Br J Cancer 80(3–4):427–437. https://doi.org/10.1038/sj.bjc.6690374
Moth EB, Parry J, Stockler MR et al (2015) Doctor-to-doctor communication of prognosis in metastatic cancer: a review of letters from medical oncologists to referring doctors. Intern Med J 45(9):909–915. https://doi.org/10.1111/imj.12776
Kaplowitz SA, Campo S, Chiu WT (2002) Cancer patients’ desires for communication of prognosis information. Health Commun 14(2):221–241. https://doi.org/10.1207/S15327027HC1402_4
Hagerty RG, Butow PN, Ellis PA et al (2004) Cancer patient preferences for communication of prognosis in the metastatic setting. J Clin Oncol 22(9):1721–1730. https://doi.org/10.1200/JCO.2004.04.095
Greisinger AJ, Lorimor RJ, Aday LA, Winn RJ, Baile WF (1997) Terminally ill cancer patients. Their most important concerns. Cancer Pract 5(3):147–154
Kiely BE, McCaughan G, Christodoulou S et al (2013) Using scenarios to explain life expectancy in advanced cancer: attitudes of people with a cancer experience. Support Care Cancer 21(2):369–376. https://doi.org/10.1007/s00520-012-1526-4
Stockler MR, Tattersall MH, Boyer MJ, Clarke SJ, Beale PJ, Simes RJ (2006) Disarming the guarded prognosis: predicting survival in newly referred patients with incurable cancer. Br J Cancer 94(2):208–212. https://doi.org/10.1038/sj.bjc.6602908
Kiely BE, Soon YY, Tattersall MH, Stockler MR (2011) How long have I got? Estimating typical, best-case, and worst-case scenarios for patients starting first-line chemotherapy for metastatic breast cancer: a systematic review of recent randomized trials. J Clin Oncol 29(4):456–463. https://doi.org/10.1200/JCO.2010.30.2174
Kiely BE, Martin AJ, Tattersall MH et al (2013) The median informs the message: accuracy of individualized scenarios for survival time based on oncologists’ estimates. J Clin Oncol 31(28):3565–3571. https://doi.org/10.1200/JCO.2012.44.7821
West TA, Kiely BE, Stockler MR (2014) Estimating scenarios for survival time in men starting systemic therapies for castration-resistant prostate cancer: a systematic review of randomised trials. Eur J Cancer 50(11):1916–1924. https://doi.org/10.1016/j.ejca.2014.04.004
Vasista A, Stockler M, Martin A et al (2019) Accuracy and prognostic significance of oncologists’ estimates and scenarios for survival time in advanced gastric cancer. Oncologist 24(11):e1102–e1107. https://doi.org/10.1634/theoncologist.2018-0613
Smith-Uffen MES, Johnson SB, Martin AJ et al (2020) Estimating survival in advanced cancer: a comparison of estimates made by oncologists and patients. Support Care Cancer 28(7):3399–3407. https://doi.org/10.1007/s00520-019-05158-5
Kiely BE, Alam M, Blinman P, Tattersall MH, Stockler MR (2012) Estimating typical, best-case and worst-case life expectancy scenarios for patients starting chemotherapy for advanced non-small-cell lung cancer: a systematic review of contemporary randomized trials. Lung Cancer 77(3):537–544. https://doi.org/10.1016/j.lungcan.2012.04.017
Vasista A, Stockler MR, West T, Wilcken N, Kiely BE (2017) More than just the median: Calculating survival times for patients with HER2 positive, metastatic breast cancer using data from recent randomised trials. Breast 31:99–104. https://doi.org/10.1016/j.breast.2016.10.007
Moth EB, Blinman P, Stefanic N et al (2020) Estimating survival time in older adults receiving chemotherapy for advanced cancer. J Geriatr Oncol 11:617–625
Marteau TM, Bekker H (1992) The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI). Br J Clin Psychol 31(3):301–306. https://doi.org/10.1111/j.2044-8260.1992.tb00997.x
Herth K (1992) Abbreviated instrument to measure hope: development and psychometric evaluation. J Adv Nurs 17(10):1251–1259. https://doi.org/10.1111/j.1365-2648.1992.tb01843.x
Scheier MF, Carver CS, Bridges MW (1994) Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol 67(6):1063–1078. https://doi.org/10.1037//0022-3514.67.6.1063
Granek L, Krzyzanowska MK, Tozer R, Mazzotta P (2013) Oncologists’ strategies and barriers to effective communication about the end of life. J Oncol Pract 9(4):e129–e135. https://doi.org/10.1200/JOP.2012.000800
Fenton JJ, Duberstein PR, Kravitz RL et al (2018) Impact of prognostic discussions on the patient-physician relationship: prospective cohort study. J Clin Oncol 36(3):225–230. https://doi.org/10.1200/JCO.2017.75.6288
Acknowledgements
We wish to thank participating patients, family members, and healthcare professionals in this study.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions Author B.K. has received research support from a Conquer Cancer Foundation of the American Society of Clinical Oncology (ASCO) Young Investigator Award; a Cancer Australia and beyondblue project grant; and a National Health and Medical Research Council (NHMRC) Australia Program Grant.
Author information
Authors and Affiliations
Contributions
SN contributed to the formal analysis; validation; verification of data; writing, original draft; and writing—review and editing. MS contributed to the conceptualization of the study, data curation, investigation, methodology, supervision, and writing—review and editing. AM contributed to formal analysis, software, and writing—review and editing. PG contributed to data curation, investigation, and writing—review and editing. PF contributed to data curation, investigation, and writing—review and editing. RZ contributed to data curation, investigation, and writing—review and editing. GH contributed to data curation, investigation, and writing—review and editing. MT contributed to the conceptualization of the study, data curation, investigation, and supervision. BK contributed to the conceptualization of the study; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; resources; supervision; validation; verification of data; writing, original draft; and writing—review and editing.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki and approved by the health research ethics committee at all participating sites.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This is in tribute to Prof Martin H.N. Tattersall 1941-2020 for his pioneering role in medical oncology and research to enhance patient-doctor communication and shared decision-making.
The original version of this article was revised. The correct statement should be: For example, if the median OS is 12 months then the worst-case scenario is less than 3 months (0.25 x 12), the most likely scenario is 6 to 24 months (0.5 to 2 x 12), and the best-case scenario is 36 months or longer (3 x 12).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nahm, S.H., Stockler, M.R., Martin, A.J. et al. Using three scenarios to explain life expectancy in advanced cancer: attitudes of patients, family members, and other healthcare professionals. Support Care Cancer 30, 7763–7772 (2022). https://doi.org/10.1007/s00520-022-07167-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07167-3