Abstract
Treatment of locally advanced head and neck carcinoma not amenable for surgical resection or resected with high-risk features is usually based on (chemo-)radiation treatment. Oral mucositis represents one of the main side effects of (chemo-)radiation, with an important impact on quality of life and causing approximately 20% of early interruption of treatment, leading to a suboptimal dose administered. Treatment and prevention of oral mucositis have a central role in the therapeutic pathways of head and neck cancer patients but remains quite challenging. Although extensive research is conducted to identify interventions for the management of mucositis, very few interventions had sufficient evidence to generate an international expert consensus. This may be partially explained by confounding factors that could influence the development and assessment of oral mucositis. Little is known about the confounding factors of oral mucositis, which, if not well balanced in an experimental study, could lead to non-solid results. The current paper aims to review the main oral mucositis confounding factors related to head and neck cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck cancer (HNC) is frequently diagnosed in locally advanced stages. Conventionally fractionated radiation therapy (RT) with concomitant chemotherapy (CT) or hyperfractionated RT combined with CT are the therapeutic standards in patients with locally advanced (LA) HNC not undergoing resection and in patients with resected high-risk LA HNC [1]. RT for HNC frequently causes oral mucositis (OM), chewing and swallowing difficulties, anorexia, xerostomia, and, consequently, weight loss. Cisplatin provides a benefit when added to RT with the cost of enhancement of treatment-related toxicities. OM is the most common side effect of RT alone or combined with chemotherapy (CRT), affecting nearly all patients (60–100%); due to OM, 20% of HNC patients discontinue RT treatment, and one out three patients therefore receive a suboptimal CT dose [2]. OM is clinically characterized by the onset of erythema, ulcers, delivering pain, eating difficulties, and, consequently, weight loss. Hence, readmission to hospital or prolongation of hospital stay is frequent due to various reasons, such as difficulty for the patient to take their domiciliary medications, the necessity to provide opioid therapy, need for total parenteral nutrition, or insert tube feeding with an important worsening in quality of life (QoL): these generate consequential economic and social costs [3, 4]. In the USA, it is estimated that the average increase in cost per HNC patient with an OM grade < 3 is up to US$1700 and for OM grade ≥ 2 is up to US$3600 from the provider perspective [2, 5].
Back to 2004, the Mucositis Group of the Multinational Association of Supportive Care in Cancer and the International Society of Oral Oncology (MASCC/ISOO) published the first clinical practice guidelines for mucositis and were reviewed periodically with the most recent update in 2020 [6]. While the guidelines are based on a systematic review, the group found very few interventions with sufficient evidence to support their use for the management of OM. These may be explained, in part, by the fact that most studies about interventions for OM are biased by confounding factors (CFs).
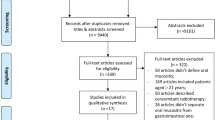
CFs are defined as variables that may compete with the exposure in explaining the outcome of a study. Therefore, it may mask or falsely demonstrate an apparent association. They occur when trying to determine the effect of exposure of possible risk factors on a disease; actually, the effect of another factor, a confounding variable, is measured. To be defined as a CF, the variable must satisfy three criteria: association with the disease (risk factor), association with the exposure, and not being an effect of the exposure [7]. If CFs are not well balanced in clinical trials, they may impair the quality of a study. Heterogeneity of HNC patients treated with RT or CRT exposes evaluation and assessment of OM to various CF; randomization is the way to balance CFs in the clinical trial; however, this is not always feasible in OM trials due to the small size and, frequently, the monocenter nature of the studies. CFs in OM studies could be classified into three classes: patient-related, treatment-related, and disease-related. Table 1 summarizes the main OM CFs. This paper aims to increase awareness of the importance of CFs in designing a clinical trial and in the evaluation of OM in HNC patients treated for LA disease and provide possible improvements for future trials.
Patient-related confounding factors
Patient-related CFs for OM in HNC patients include age, gender, oral hygiene, nutritional status, comorbidities, smoking status, biochemical parameters, salivary secretory function, and genetic factors, as will be detailed below. However, evidence in the literature is inconsistent to support each of these CFs.
The impact of age on the development of OM was evaluated in a few studies. Merlano et al. found no statistical differences in comparing younger and older patients (age limit 65 years old) with values of grade 3 “stomatitis” (38.8% and 33.3%, respectively) and grade 4 “stomatitis” (25.4% and 32.3%, respectively) [8]. On the contrary, other series reported a higher risk of OM in younger patients [9,10,11]. Recently, a higher incidence and severity of OM in HNC after CRT were observed in young patients (< 45 years) when compared with older patients (> 58 years; p < 0.01), despite the similarities in clinical staging and treatment protocols [12]. Although data are still scarce to consider young populations at a higher risk of OM, factors, such as a higher cell renewal rate, more rapid epithelial mitotic rate, and more epidermal growth factors receptors in the epithelium of younger patients, could explain the difference in OM susceptibility [13]. On the other hand, frequent comorbidities and lower healing repair capacity could enhance OM susceptibility in geriatric patients [14]. In particular, a high prevalence of diabetes is considered a risk factor for OM [5] due to changes in microvascular gingiva and alveolar mucosa, changes in oral microbiota composition, defect of polymorphonuclear function, and abnormal metabolism of collagen [15].
Data on gender impact on OM are not homogeneous. The majority of papers reported a higher risk for OM development in female patients [16,17,18]. The hormonal status could play an important role; it is well known how hormonal post-translational modifications could enhance the risk of cytotoxicity and OM [19]. However, more data are needed to address this issue better; in this regard, in contrast, a few papers showed data with a higher risk of OM in male patients [20].
Wuketic et al. [21], in a prospective study on outpatients receiving CT for solid tumors, including HNC, confirmed the role of oral hygiene as CFs: the median time period since the last dental checkup was more than twice as high among the patients with clinical relevant OM [7 vs 16 months]. Poor oral hygiene influences oral microbiota and could lead to an increase in Gram-negative bacilli (GNB). The impact of oral microbiota in the development of OM after CRT for HNC patients remains debated. The presence of obligate and facultative anaerobic GNB Bacteroidales G2, Capnocytophaga, Eikenella, Mycoplasma, and Sneathia, as well as anaerobic GNB (Porphyromonas and Tannerella) seems to be related to grade > 2 OM. Moreover, the abundance of GNB (Fusobacterium, Haemophilus, Tannerella, Porphyromonas, and Eikenella) may influence the predisposal to develop OM [22, 23]. A series of 82 HNC patients treated with (C)RT [24] showed higher levels of Cardiobacterium; Granulicatella; Prevotella; Fusobacterium; Strepotococco; and Megasphaere influence the onset of severe OM. In nasopharyngeal carcinoma, RT patients harboring severe OM present a lower bacterial alpha diversity and higher abundance of Actinobacillus [25]. A prospective randomized trial of LA nasopharyngeal cancer undergoing CRT demonstrated that concurrent administration of probiotics led to a reduction in the rate of severe OM [26].
Nutritional status influences the development of OM; in fact, HNC patients in treatment with RT or CRT not compliant with individual dietary counseling had a greater incidence of heavy OM (88.9% vs 11.1%; p < 0.009) [27]. Nutritional status, evaluated with Nutritional Risk Screening (NRS) 2002 score before the start of RT and body weight loss > 5%, had been demonstrated to influence the development of OM in nasopharyngeal carcinoma patients who received CRT [28, 29]. Considering body mass index (BMI) as an indicator of nutritional status, oral cancer patients with BMI > 22 had a higher probability of developing OM during RT treatment if compared with patients with normal BMI [30,31,32,33]. Mechanisms underlying OM development in low BMI patients may derive from alterations in the host immune responses and from reduced cell migration able to repair injured tissues [31].
The relation between smoking status and OM is debated in the literature. A retrospective study showed that RT could be more effective on tumors and, at the same time, more toxic on healthy mucosa in patients without a smoking history due to higher tissue oxygenation [34]. However, other series reported a higher risk of OM in current smokers due to the pro-inflammatory activity of smoking, which could increase the damage to the mucosa [21, 35]. Heterogeneous data could be due to the fact that trials generally did not differentiate the status of smoking in “current” or “previous” and by the fact that non-smokers are usually HPV-positive [36].
Even biochemical parameters before starting CRT, such as low levels of hemoglobin, lymphocyte count, white blood cells, platelet count, and creatinine levels, upper normal limits were found to be significantly associated with the development of severe OM [20, 35, 37], as they are involved in the inflammatory response and wound healing capability.
Saliva plays a crucial role in maintaining oral mucosa and teeth health. Many factors could alter the salivary flow, for example, previous surgery or RT to the head and neck district or drugs, such as opioids. Alterations in salivary flow rate or salivary components may affect oral/mucosal health and may influence the severity of OM [38]. Low salivary flow rates at baseline and during CT were identified as risk factors for OM in a study including 63 patients receiving 5-fluorouracil as CT for a different type of cancer [10]. The composition of saliva may impact the risk for OM too: an association in the univariable analysis between an early increase of salivary cytokines (interleukin [IL]-1β, IL-6, and tumor necrosis factor-α (TNF-α)) and the development of severe OM in HNC patients treated with CRT had been found. Intriguingly, the baseline level of salivary cytokines, on the contrary, was not associated with a high risk of development of severe OM [39].
Finally, important factors linked to the increased risk of development of OM are represented by genetic alterations. It is well known that the major damage induced by RT is represented by DNA double-strand breaks, and repair pathways are of extreme importance in the resolution of radiation damage in normal tissues; an alteration, also minor as single nucleotide polymorphisms (SNPs), in genes that regulated repair of DNA damage may interfere with their function and determine the basis for increased toxicity. In the literature, trials had explained the relationship between the development of acute adverse radiation in HNC patients treated with RT and polymorphisms in DNA repair genes [40]. Available data reported a risk of grade ≥ 2 mucositis significantly increased in patients with XRCC1-399Gln allele genotypes both for CRT (p = 0.035, HR = 1.72, 95% CI = 1.03–2.86) than for RT alone (p = 0.049, HR = 2.50, 95% CI = 0.97–6.47) groups [41]. Interestingly, this difference seems unrelated to biologically effective radiation dose. Venkatesh et al. [42] reported that the NBN gene variants and haplotypes are associated with the risk of developing OM on HNC patients undergoing CT/RT. The odds of patients experiencing severe OM (grade 2) with a recessive allele of NBN (rs1805794) was 4.72-times higher (95% CI: 1.384–16.151; p = 0.013). Wardill et al. [43] recently reviewed genetic predictors of OM risk. They identified genetic factors related to pharmacogenetic variants as mutations in drug-metabolizing pathways (i.e., methylenetetrahydrofolate reductase (MTHFR), cytochrome P459, dihydropyrimidine dehydrogenase (DPYD), thymidylate synthase (TYMS), ATP-binding cassette (ABC) transporters, and glucuronosyltransferase 1A (UGT1A)); genetic factors related to cell signaling pathways (i.e., NBN rs 1,805,794 CC genotype, high RPM1 gene expression, MDM2 (309 T > G), RB1rs2227311), genetic factors related to immunogenetic variants (i.e., TNFRSR1A-610/ > G, TNFA-1211 T > C (CC genotype), and GHLR-2531C > T); and genetic factors uncategorized (EDN1 rs1800541, ZNF24 rs11081899-A, APEH c.1521G > C, and miR-1206 rs2114358). The importance of these studies is given by the need to develop a risk analysis model that could predict acute radiation effects including physical dose parameters and genotypic information. Even if a growing volume of SNP data suggests the genetic basis for susceptibility to RT-induced acute effects, it is still less clear whether the SNPs can serve as a biomarker for improved efficacy of RT. The major critic is represented by the fact that human genetic variation is very wide and we do not completely understand how this diversity could influence the phenotypic expression; this could explain the large variability in the results of available data. Moreover, it is not clear if it could be more useful to detect rare alterations having large effects or more common ones with smaller effects.
Disease-related confounding factors
Advanced HNC may involve anatomical structures, muscles, nerves, vessels, and bones causing pain or difficulty chewing, swallowing, or moving the jaw or tongue, mucosal ulceration, and oral infections. Subsite of the primary disease plays a crucial role: incidence of OM during treatment is higher in oral and oropharyngeal tumors than hypopharynx and laryngeal tumors [44]. A retrospective analysis of 326 oropharyngeal and oral cavity squamous cell carcinoma who underwent RT with curative intent showed that patients with oropharyngeal cancer (either HPV positive or negative) had an increased risk of developing severe OM (p = 0.005) [20]. However, it is possible that the subsite of disease could be considered just as a proxy of total RT volume, thus influencing the risk of OM.
The impact of human papillomavirus (HPV) OM was investigated in a retrospective analysis of patients affected by oropharyngeal cancer with known HPV status treated with concurrent CT and RT [34]. HPV-positive patients had a 6.86-fold increase in the risk of having severe OM. This effect was preserved after adjusting for patient smoking status, nodal stage, RT technique, and RT maximum dose. Mechanisms of higher OM susceptibility for HPV-positive patients are unclear; maybe the same factors that contribute to the favorable response to RT (such as immune surveillance to viral-specific tumor antigens, an intact apoptotic response, absence of field cancerization) might facilitate an increased inflammatory response to (C)RT leading to a risk of OM [34].
Treatment-related confounding factors
Radiotherapy
Radical (C)RT is central in the treatment of LA HNC, and it is strictly related to the onset of OM. Despite technological improvement, patients developed unexpected toxicity in some cases, and it is still not clear why patients treated with the same schedule developed different toxicities. Several factors related to the onset of OM are a type of fractionation, dosimetric parameters, and RT techniques. It is known that altered fractionated (AF) RT was associated with a significant improvement in overall survival, progression-free survival, cancer mortality, local, and regional failure compared with standard fractionation radiotherapy. It is also established that AF demonstrated a higher OM incidence than the standard schedule [45]. In several randomized trials, HNC patients on AF gave the possibility to analyze the effect of different schedules on toxicity (in addition to oncological outcomes). For example, the CHART trial (54 Gy in 36 fractions over just 12 consecutive days compared to conventional schedule delivering 66 Gy in 33 fractions with five fractions per week) reported a higher incidence of confluent mucositis (75% vs 44%) and was in the CHART arm compared to the conventional one; moreover, also the peak prevalence of confluent mucositis was significantly higher (60% vs 34%) in the experimental arm with earlier onset (end of the third week vs end of the sixth week after the start of RT) [46]. Mortensen et al. [47] reported the analysis of the incidence and prevalence of acute and late morbidity observed in the 1476 patients in the DAHANCA 6 and 7 multicenter randomized trial [47]. Accelerated RT caused a significant increase in the peak incidence of OM (33% vs 53%) and the confluent OM persisted longer respect conventional group. Some data also reported the highest incidence of OM (for an accelerated schedule on 7 days per week) with a longer duration compared to the DAHANCA study (94% vs 53% with a mean duration of 4.2 vs 1.5 weeks) [48]. Moreover, with a regimen of AF-RT (radiation doses of 64.8 Gy in 3.5 weeks without CT, 1.8 Gy twice a day/5 days per week), the rate of severe OM was 84%, which was higher than observed with conventional CRT or accelerated CRT (69% and 76%, respectively) [49].
Another important factor that could confound OM registration is the wide variability in the countering of the oral cavity that could influence the reported dose and corresponding normal tissue complication probability (NTCP) model. The DAHANCA, EORTC, GORTEC, HKNPCSG, NCIC CTG, NCRI, NRG Oncology, and TROG consensus guidelines defined a surrogate structure named “extended oral cavity,” which was defined posterior to the internal arch of the mandible and maxilla [50]. This definition includes substructures not considered anatomically a part of the oral cavity; this would generate inconsistent dose–effect relationships between the dose distributions to anatomical structures involved in OM. To improve plan optimization and assure a proper interpretation and a reliable comparison of results, it is important to describe how the different structures are delineated. There has been a large effort to develop and validate accurate multifactorial NTCP models; however, the prediction of the severity of acute mucositis for individual patients is highly challenging.
The relationship between OM and dosimetric data derived from different methods of delineation (oral cavity contour, mucosal surface contours, oral cavity surface contour, oral/oropharyngeal surface contour) had been studied without finding any relation between dosimetric parameters and the duration of grade 3 OM or duration of opiate use; however, a trend towards significance between duration of strong opiate use and pretreatment weight had been shown [51]. Spatial dose distribution should be taken into account in parallel with a dose–volume histogram to predict regions where more severe OM is expected (non-keratinized vs keratinized area). Dean et al. [52] generated and validated a model to predict the severity of acute OM for individual patients and used it to establish RT dose–response associations for severe OM that could be used to inform improved RT planning.
Proton therapy is an alternative to intensity-modulated radiation therapy in treating LA HNC. Several studies showed that proton therapy significantly reduced toxicities, such as OM and dysphagia, when compared to photon-based therapy, independently by primary tumor subsites, without worsening clinical efficacy. However, currently is still unknown if clinical benefit is related to specific subsites or not [53,54,55].
Systemic therapy
It is well known that CT adds survival benefit in the treatment of LA HNC than RT therapy alone, although with an increasing of toxicities. It is demonstrated that CT increases the risk of severe OM over RT alone by four times [56]. CT-induced nausea and vomiting are CFs in the evaluation of OM, potentially causing a reduction in food intake. This CF is related to the dose intensity (three weekly/weekly) and the type of CT administered, which is generally cisplatin. In 2017, a meta-analysis by Szturz et al. [57] of literature comparing weekly and three-weekly cisplatin concomitant with RT both in the post-operative and definitive setting of LA HNC. They found no difference in treatment efficacy but fewer toxicities and more compliance with weekly administration. Concerning the incidence of OM, they found a lower incidence of severe OM in the post-operative setting but not for the definitive setting. To reduce toxicities in good risk LA HNC, trials have been oriented to substituting cisplatin with less toxic agents. Analyzing the studies comparing cetuximab with cisplatin added to RT in HPV-positive cancer, the literature report that the rate of OM was not different using one or the other drug [58,59,60]. Similarly, the addition of avelumab to (C)RT did not cause an increase in OM in the only randomized trial [61].
Other CFs
Humidification can play a role in the incidence of OM in patients treated with RT. Humidification can help mitigate OM symptom burden, can limit functional nutritional status decline during RT, and reduce hospitalization [62].
Outcome measures as a source of bias
Incidence and severity of OM can be assessed with different scales: World Health Organization (WHO), Oral Mucositis Assessment Scale (OMAS), European Organization for Research and Treatment Cancer Quality of Life Questionnaire (EORTC QLQ-C30), National Cancer Institute Common Toxicity Criteria (NCI-CTC), Oral Mucositis Daily Questionnaire (OMDQ), and Functional Assessment of Cancer Therapy (FACT-G) [15]. They all have clinical and functional parameters of evaluation. Most of the scales are anatomically based and highly dependent on the training of clinicians. The WHO scale combines signs of mucosal injury with functional damage. There is no evidence about the superiority of one scale over another. However, perceptions and assessments of OM during chemoradiotherapy can differ between the patient and the physician. It could be difficult for either physician or patient to distinguish mucosal injury and symptoms related to OM due to chemo-RT or previous exposition to factors that affect mucosal status. HNC usually had previous exposure to alcohol or smoke that can cause erythroplakia, oral ulcers, mucosal fibrosis, and xerostomia; moreover, the tumor itself could invade the oral cavity or oropharyngeal structures, such as muscles, nerves, vessels, and bone causing dysphagia and pain; normal mucosal status could be damaged by production pro-inflammatory cytokines by tumors itself; finally, normal structure or oral cavity could be altered by previous surgery or RT [63].
A Patient-Reported Outcome (PRO) Assessment is a measurement based on a patient’s health status that comes directly from the patient that a doctor or any other person cannot modify or interpret. PROs should report what matters to the patient, perception of adverse events, symptoms related to the disease, and general physical condition represents an important set of information useful for improving the efficacy and tolerability of anticancer therapies. The relevant symptoms most frequently complained by HNC patients in treatment undergoing CRT are dysgeusia, pain, and OM [64]. During (C)RT for locally advanced head and neck squamous cell carcinoma, the assessment of symptoms (including OM) as evaluated by the clinicians is lower than the same assessed by PROs, particularly for low or mild symptoms (65).
Possible solutions to overcome CF in OM studies
Based on the data mentioned above, it is clear how OM studies in HNC patients are biased by multiple CFs related to patients, disease, and treatment heterogeneity. Moreover, OM do not appear to be just a sum of CF, but a multifactorial events: in this way, large interventional studies are needed to demonstrate significant findings, where also other factors not previously considered could be taken into account and weighed in their added risk.
The first obvious way to reduce the risk of confounding factors is to conduct a randomized controlled trial that could ultimately address the diversity of included patients. Multicenter trials are needed to reach an adequate sample size and to improve the possibility to have solid data for a strong treatment recommendation for mucositis treatment, making these trials more appealing for funding. We therefore advocate that the scientific community of researchers involved in OM would join the efforts in this regard, so as to provide useable data.
Another strategy to be employed is the evaluation of new treatments for mucositis in a specific subgroup of patients, as being identified as having a higher risk of this adverse event. This could pave the way for a personalized approach according to the perceived risk. For instance, as HPV has been identified to be associated with a higher probability of developing severe mucositis, the implementation of therapeutic strategies in this subgroup of patients could be justified.
On the other side, international collaborations are eagerly awaited to support studies aimed at identifying patient, disease, and treatment characteristics that could increase the risk of mucositis. Thanks to this, it could be possible to plan future trials testing new treatments for OM prevention and/or treatment that would consider CFs as stratification factors when possible.
Conclusion
Severe OM remains an important side effect of (C)RT of HNC, leading to patients’ worsening QoL and limiting compliance with treatment. Trials regarding OM treatment and prevention are commonly biased by confounding factors; consequently, poor data with strong efficacy evidence could help clinicians in the treatment and prevention of OM. CFs need to be prevented or removed as much as possible to understand the importance of medical interventions better. Finally, PROs instruments of assessment and physician-assessed have to be used in clinical trials. The inclusion of PROs provides information that can improve clinical management and raise the quality level of clinical trials.
Data availability
Not applicable.
Code availability
Not applicable.
References
Machiels J-P, René Leemans C, Golusinski W, Grau C, Licitra L, Gregoire V (2020 Nov) Squamous cell carcinoma of the oral cavity, larynx, oropharynx and hypopharynx: EHNS–ESMO–ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 31(11):1462–1475
Berger K, Schopohl D, Bollig A, Strobach D, Rieger C, Rublee D et al (2018) Burden of oral mucositis: a systematic review and implications for Future Research. Oncol Res Treat 41(6):399–405
Ravasco P, Monteiro-Grillo I, Marques Vidal P, Camilo ME (2005) Impact of nutrition on outcome: a prospective randomized controlled trial in patients with head and neck cancer undergoing radiotherapy. Head Neck 27(8):659–668
Silander E, Nyman J, Bove M, Johansson L, Larsson S, Hammerlid E (2012) Impact of prophylactic percutaneous endoscopic gastrostomy on malnutrition and quality of life in patients with head and neck cancer - a randomized study. Head Neck 34(1):1–9
Elting LS, Cooksley CD, Chambers MS, Garden AS (2007) Risk, outcomes, and costs of radiation-induced oral mucositis among patients with head-and-neck malignancies. Int J Radiat Oncol 68(4):1110–1120
Elad S, Cheng KKF, Lalla RV, Yarom N, Hong C, Logan RM et al (2020) MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 126(19):4423–4431
Jager KJ, Zoccali C, MacLeod A, Dekker FW (2008) Confounding: what it is and how to deal with it. Kidney Int 73(3):256–260
Merlano MC, Monteverde M, Colantonio I, Denaro N, Lo Nigro C, Natoli G et al (2012) Impact of age on acute toxicity induced by bio- or chemo-radiotherapy in patients with head and neck cancer. Oral Oncol 48(10):1051–1057
Pico JL, Avila-Garavito A, Naccache P (1998) Mucositis: Its Occurrence, Consequences, and Treatment in the Oncology Setting. Oncologist 3(6):446–451
McCarthy GM, Awde JD, Ghandi H, Vincent M, Kocha WI (1998) Risk factors associated with mucositis in cancer patients receiving 5-fluorouracil. Oral Oncol 34(6):484–90. https://doi.org/10.1016/s1368-8375(98)00068-2
Zalcberg J, Kerr D, Seymour L, Palmer M (1998) Haematological and non-haematological toxicity after 5-fluorouracil and leucovorin in patients with advanced colorectal cancer is significantly associated with gender, increasing age and cycle number. Tomudex International Study Group. Eur J Cancer 34(12):1871–1875
Morais-Faria K, Palmier NR, de Lima CJ, de Castro JG, Dias RB, da Graça PH et al (2020) Young head and neck cancer patients are at increased risk of developing oral mucositis and trismus. Support Care Cancer 28(9):4345–4352
D’Hondt L, Lonchay C, Andrei M, Canon J-L (2006) Oral mucositis induced by anticancer treatments: physiopathology and treatments. Ther Clin Risk Manag 2(2):159–68
Bøje CR (2014) Impact of comorbidity on treatment outcome in head and neck squamous cell carcinoma – A systematic review. Radiother Oncol 110(1):81–90
De Sanctis V, Bossi P, Sanguineti G, Trippa F, Ferrari D, Bacigalupo A et al (2016) Mucositis in head and neck cancer patients treated with radiotherapy and systemic therapies: literature review and consensus statements. Crit Rev Oncol Hematol 100:147–166
Sonis ST, Elting LS, Keefe D, Peterson DE, Schubert M, Hauer-Jensen M et al (2004) Perspectives on cancer therapy-induced mucosal injury: pathogenesis, measurement, epidemiology, and consequences for patients. Cancer 100(S9):1995–2025
Vokurka S, Bystrická E, Koza V, Scudlová J, Pavlicová V, Valentová D et al (2006) Higher incidence of chemotherapy induced oral mucositis in females: a supplement of multivariate analysis to a randomized multicentre study. Support Care Cancer 14(9):974–976
Gebri E, Kiss A, Tóth F, Hortobágyi T (2020 Dec) Female sex as an independent prognostic factor in the development of oral mucositis during autologous peripheral stem cell transplantation. Sci Rep 10(1):15898
Huang RS, Kistner EO, Bleibel WK, Shukla SJ, Dolan ME (2007) Effect of population and gender on chemotherapeutic agent–induced cytotoxicity. Mol Cancer Ther 6(1):31–36
Nishii M, Soutome S, Kawakita A, Yutori H, Iwata E, Akashi M et al (2020) Factors associated with severe oral mucositis and candidiasis in patients undergoing radiotherapy for oral and oropharyngeal carcinomas: a retrospective multicenter study of 326 patients. Support Care Cancer 28(3):1069–1075
Wuketich S, Hienz SA, Marosi C (2012) Prevalence of clinically relevant oral mucositis in outpatients receiving myelosuppressive chemotherapy for solid tumors. Support Care Cancer 20(1):175–183
Vesty A, Gear K, Biswas K, Mackenzie BW, Taylor MW, Douglas RG (2020) Oral microbial influences on oral mucositis during radiotherapy treatment of head and neck cancer. Support Care Cancer 28(6):2683–2691
Hou J, Zheng H, Li P, Liu H, Zhou H, Yang X (2018 Oct) Distinct shifts in the oral microbiota are associated with the progression and aggravation of mucositis during radiotherapy. Radiother Oncol 129(1):44–51
Reyes-Gibby CC, Wang J, Zhang L, Peterson CB, Do K, Jenq RR et al (2020) Oral microbiome and onset of oral mucositis in patients with squamous cell carcinoma of the head and neck. Cancer 126(23):5124–5136
Zhu X-X, Yang X-J, Chao Y-L, Zheng H-M, Sheng H-F, Liu H-Y et al (2017) The potential effect of oral microbiota in the prediction of mucositis during radiotherapy for nasopharyngeal carcinoma. EBioMedicine 18:23–31
Jiang C, Wang H, Xia C, Dong Q, Chen E, Qiu Y et al (2019) A randomized, double-blind, placebo-controlled trial of probiotics to reduce the severity of oral mucositis induced by chemoradiotherapy for patients with nasopharyngeal carcinoma. Cancer 125(7):1081–1090
HopanciBicakli D, OzkayaAkagunduz O, MeseriDalak R, Esassolak M, Uslu R, Uyar M (2017) The effects of compliance with nutritional counselling on body composition parameters in head and neck cancer patients under radiotherapy. J Nutr Metab 2017:1–7
Li K, Yang L, Xin P, Chen Y, Hu Q, Chen X et al (2017) Impact of dose volume parameters and clinical factors on acute radiation oral mucositis for locally advanced nasopharyngeal carcinoma patients treated with concurrent intensity-modulated radiation therapy and chemoradiotherapy. Oral Oncol 72:32–37
Shu Z, Zeng Z, Yu B, Huang S, Hua Y, Jin T et al (2020) Nutritional status and its association with radiation-induced oral mucositis in patients with nasopharyngeal carcinoma during radiotherapy: a prospective study. Front Oncol 6(10):594687
Saito N, Imai Y, Muto T, Sairenchi T (2012) Low body mass index as a risk factor of moderate to severe oral mucositis in oral cancer patients with radiotherapy. Support Care Cancer 20(12):3373–3377
Raber-Durlacher JE, Weijl NI, Abu Saris M, de Koning B, Zwinderman AH, Osanto S (2000) Oral mucositis in patients treated with chemotherapy for solid tumors: a retrospective analysis of 150 cases. Support Care Cancer 8(5):366–371
Meyerhardt JA, Catalano PJ, Haller DG, Mayer RJ, Benson AB, Macdonald JS et al (2003) Influence of body mass index on outcomes and treatment-related toxicity in patients with colon carcinoma. Cancer 98(3):484–495
Meyerhardt JA, Tepper JE, Niedzwiecki D, Hollis DR, McCollum AD, Brady D et al (2004) Impact of body mass index on outcomes and treatment-related toxicity in patients with stage II and III rectal cancer: findings from intergroup trial 0114. J Clin Oncol 22(4):648–657
Vatca M, Lucas JT, Laudadio J, D’Agostino RB, Waltonen JD, Sullivan CA et al (2014) Retrospective analysis of the impact of HPV status and smoking on mucositis in patients with oropharyngeal squamous cell carcinoma treated with concurrent chemotherapy and radiotherapy. Oral Oncol 50(9):869–876
Tao Z, Gao J, Qian L, Huang Y, Zhou Y, Yang L et al (2017) Factors associated with acute oral mucosal reaction induced by radiotherapy in head and neck squamous cell carcinoma: a retrospective single-center experience. Medicine (Baltimore) 96(50):e8446
Zevallos JP, Mallen MJ, Lam CY, Karam-Hage M, Blalock J, Wetter DW et al (2009) Complications of radiotherapy in laryngopharyngeal cancer: effects of a prospective smoking cessation program. Cancer 115(19):4636–4644
Mizuno H, Miyai H, Yokoi A, Kobayashi T, Inabu C, Maruyama T et al (2019) Relationship between renal dysfunction and oral mucositis in patients undergoing concurrent chemoradiotherapy for pharyngeal cancer: a retrospective cohort study. In Vivo 33(1):183–189
Amerongen AN, Veerman E (2002) Saliva the defender of the oral cavity. Oral Dis 8(1):12–22
Bossi P, Bergamini C, Miceli R, Cova A, Orlandi E, Resteghini C et al (2016 Dec) Salivary cytokine levels and oral mucositis in head and neck cancer patients treated with chemotherapy and radiation therapy. Int J Radiat Oncol 96(5):959–966
Werbrouck J, De Ruyck K, Duprez F, Veldeman L, Claes K, Van Eijkeren M et al (2009) Acute normal tissue reactions in head-and-neck cancer patients treated with IMRT: influence of dose and association with genetic polymorphisms in DNA DSB repair genes. Int J Radiat Oncol 73(4):1187–1195
Pratesi N, Mangoni M, Mancini I, Paiar F, Simi L, Livi L et al (2011) Association between single nucleotide polymorphisms in the XRCC1 and RAD51 genes and clinical radiosensitivity in head and neck cancer. Radiother Oncol 99(3):356–361
Venkatesh GH, Manjunath VB, Mumbrekar KD, Negi H, Fernandes DJ, Sharan K et al (2014) 2014 Polymorphisms in radio-responsive genes and its association with acute toxicity among head and neck cancer patients Li JJ, editor. PLoS ONE 9(3):e89079
On behalf of The Mucositis Study Group of the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO), Wardill HR, Sonis ST, Blijlevens NMA, Van Sebille YZA, Ciorba MA, et al. 2020 Prediction of mucositis risk secondary to cancer therapy: a systematic review of current evidence and call to action. Support Care Cancer. 28(11):5059–73
van den Broek GB, Balm AJM, van den Brekel MWM, Hauptmann M, Schornagel JH, Rasch CRN (2006) Relationship between clinical factors and the incidence of toxicity after intra-arterial chemoradiation for head and neck cancer. Radiother Oncol 81(2):143–150
Lacas B, Bourhis J, Overgaard J, Zhang Q, Grégoire V, Nankivell M et al (2017) Role of radiotherapy fractionation in head and neck cancers (MARCH): an updated meta-analysis. Lancet Oncol 18(9):1221–1237
Bentzen SM, Saunders MI, Dische S, Bond SJ (2001) Radiotherapy-related early morbidity in head and neck cancer: quantitative clinical radiobiology as deduced from the CHART trial. Radiother Oncol 60(2):123–135
Mortensen HR, Overgaard J, Specht L, Overgaard M, Johansen J, Evensen JF et al (2012) Prevalence and peak incidence of acute and late normal tissue morbidity in the DAHANCA 6&7 randomised trial with accelerated radiotherapy for head and neck cancer. Radiother Oncol 103(1):69–75
Skladowski K, Maciejewski B, Golen M, Tarnawski R, Slosarek K, Suwinski R et al (2006) Continuous accelerated 7-days-a-week radiotherapy for head-and-neck cancer: long-term results of Phase III clinical trial. Int J Radiat Oncol 66(3):706–713
Bourhis J, Overgaard J, Audry H, Ang KK, Saunders M, Bernier J et al (2006) Hyperfractionated or accelerated radiotherapy in head and neck cancer: a meta-analysis. The Lancet 368(9538):843–854
Brouwer CL, Steenbakkers RJHM, Bourhis J, Budach W, Grau C, Grégoire V et al (2015) CT-based delineation of organs at risk in the head and neck region: DAHANCA, EORTC, GORTEC, HKNPCSG, NCIC CTG, NCRI, NRG Oncology and TROG consensus guidelines. Radiother Oncol 117(1):83–90
Yahya S, Benghiat H, Nightingale P, Tiffany M, Sanghera P, Hartley A (2016) Does dose to an oral mucosa organ at risk predict the duration of grade 3 mucositis after intensity-modulated radiotherapy for oropharyngeal cancer? Clin Oncol 28(12):e216–e219
Dean JA, Welsh LC, Wong KH, Aleksic A, Dunne E, Islam MR et al (2017) Normal tissue complication probability (NTCP) modelling of severe acute mucositis using a novel oral mucosal surface organ at risk. Clin Oncol 29(4):263–273
Jakobi A, Bandurska-Luque A, Stützer K, Haase R, Löck S, Wack L-J et al (2015) Identification of patient benefit from proton therapy for advanced head and neck cancer patients based on individual and subgroup normal tissue complication probability analysis. Int J Radiat Oncol 92(5):1165–1174
Romesser PB, Cahlon O, Scher E, Zhou Y, Berry SL, Rybkin A et al (2016) Proton beam radiation therapy results in significantly reduced toxicity compared with intensity-modulated radiation therapy for head and neck tumors that require ipsilateral radiation. Radiother Oncol 118(2):286–292
Moreno AC, Frank SJ, Garden AS, Rosenthal DI, Fuller CD, Gunn GB et al (2019) Intensity modulated proton therapy (IMPT) – The future of IMRT for head and neck cancer. Oral Oncol 88:66–74
Sanguineti G, Sormani MP, Marur S, Gunn GB, Rao N, Cianchetti M et al (2012) Effect of radiotherapy and chemotherapy on the risk of mucositis during intensity-modulated radiation therapy for oropharyngeal cancer. Int J Radiat Oncol 83(1):235–242
Szturz P, Wouters K, Kiyota N, Tahara M, Prabhash K, Noronha V et al (2017) Weekly low-dose versus three-weekly high-dose cisplatin for concurrent chemoradiation in locoregionally advanced non-nasopharyngeal head and neck cancer: a systematic review and meta-analysis of aggregate data. Oncologist 22(9):1056–1066
Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tân PF et al (2010) Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med 363(1):24–35
Mehanna H, Robinson M, Hartley A, Kong A, Foran B, Fulton-Lieuw T et al (2019) Radiotherapy plus cisplatin or cetuximab in low-risk human papillomavirus-positive oropharyngeal cancer (De-ESCALaTE HPV): an open-label randomised controlled phase 3 trial. The Lancet 393(10166):51–60
Gillison ML, Trotti AM, Harris J, Eisbruch A, Harari PM, Adelstein DJ et al (2019) Radiotherapy plus cetuximab or cisplatin in human papillomavirus-positive oropharyngeal cancer (NRG Oncology RTOG 1016): a randomised, multicentre, non-inferiority trial. The Lancet 393(10166):40–50
Lee NY, Ferris RL, Psyrri A, Haddad RI, Tahara M, Bourhis J et al (2021) Avelumab plus standard-of-care chemoradiotherapy versus chemoradiotherapy alone in patients with locally advanced squamous cell carcinoma of the head and neck: a randomised, double-blind, placebo-controlled, multicentre, phase 3 trial. Lancet Oncol 22(4):450–462
Macann A, Fauzi F, Simpson J, Sasso G, Krawitz H, Fraser-Browne C et al (2017) Humidification mitigates acute mucosal toxicity during radiotherapy when factoring volumetric parameters. Trans Tasman Radiation Oncology Group (TROG) RadioHUM 07.03 substudy. Oral Oncol. 75:75–80
Chung Y-L, Pui NNM (2017) Confounding factors associated with oral mucositis assessment in patients receiving chemoradiotherapy for head and neck cancer. Support Care Cancer 25(9):2743–2751
Hamilton SN, Tran E, Ho C, Berthelet E, Wu J, DeVries K et al (2021) Patient-reported outcome measures in patients undergoing radiotherapy for head and neck cancer. Support Care Cancer 29(5):2537–2547
Falchook AD, Green R, Knowles ME, Amdur RJ, Mendenhall W, Hayes DN et al (2016) Comparison of patient- and practitioner-reported toxic effects associated with chemoradiotherapy for head and neck cancer. JAMA Otolaryngol Neck Surg 142(6):517
Acknowledgements
Thanks to Aashni Shah and Luca Giacomelli (Polistudium, Italy) for their assistance. This support has been paid with internal funds.
Funding
Open access funding provided by Università degli Studi di Brescia within the CRUI-CARE Agreement. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Idea of the article: Paolo Bossi, Luigi Lorini, Francesco Perri, and Stefania Vecchio; literature research: Luigi Lorini, Francesco Perri, Liliana Belgioia, Paolo Bossi, Irene Brana; critical revision of the paper: Luigi Lorini, Paolo Bossi, Irene Brana, Liliana Belgioia, Francesco Perri, Marie Vinches, Sharon Elad, and Stefana Vecchio.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
PB Advisory board or conference honoraria: Merck, Sanofi-Regeneron, Merck Sharp & Dohme, Sun Pharma, Angelini, Molteni, Bristol-Myers Squibb, GSK, nestle.
Other authors have nothing to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lorini, L., Perri, F., Vecchio, S. et al. Confounding factors in the assessment of oral mucositis in head and neck cancer. Support Care Cancer 30, 8455–8463 (2022). https://doi.org/10.1007/s00520-022-07128-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07128-w