Abstract
Purpose
There is paucity of data on the prevalence of malnutrition among cancer patients in India and a brief tool to identify the same would be an asset. Our aim was to evaluate two nutrition screening tools and calf circumference (CC) with the European Society for Clinical Nutrition and Metabolism (ESPEN) consensus guidelines for malnutrition among patients with head and neck (H&N) and gastrointestinal (GI) cancers.
Methods
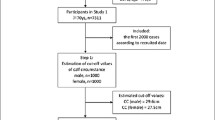
Nutritional evaluation was performed preoperatively using Malnutrition Universal Screening Tool (MUST), Short Form of Mini Nutritional Assessment (MNA-SF), and calf circumference (CC) in 206 patients. The diagnostic accuracy of these tools was compared with the ESPEN criteria for malnutrition. Patients evaluated were grouped as normal or malnourished. The incidence of infection, antibiotic days, antibiotic escalation, and length of stay was compared among the groups. Clavien-Dindo score at discharge, 30-day readmission, and mortality were also examined.
Results
A total of 28.6% were malnourished as per ESPEN criteria and 25.2% had CC less than the cut-off. With respect to ESPEN criteria, MUST and MNA-SF had 100% sensitivity and negative predictive value. CC had the highest specificity and positive predictive value for the total population (91.16%, 75% respectively). The agreement between the tools was acceptable except in MNA-SF (MNA-SF-ESPEN κ = 0.228, MUST-ESPEN κ = 0.565, CC-ESPEN κ = 0.594). There was no difference in postoperative outcomes between the malnourished and normal.
Conclusion
Thus, more than a quarter of patients with H&N and GI cancers are malnourished preoperatively. As the best agreement between the screening tools was for MUST-ESPEN and CC-ESPEN, either of them can be used to identify malnutrition at admission.



Similar content being viewed by others
Data availability
We have full control of data and we agree to the fact that the journal or reviewers can request to view the data. Data can be made available upon request to the corresponding author.
Code availability
Not applicable.
References
Muscaritoli M, Lucia S, Farcomeni A, Lorusso V, Saracino V, Barone C, Plastino F, Gori S, Magarotto R, Carteni G, Chiurazzi B, Pavese I, Marchetti L, Zagonel V, Bergo E, Tonini G, Imperatori M, Iacono C, Maiorana L, Pinto C, Rubino D, Cavanna L, Di Cicilia R, Gamucci T, Quadrini S, Palazzo S, Minardi S, Merlano M, Colucci G, Marchetti P, Premi OSG (2017) Prevalence of malnutrition in patients at first medical oncology visit: the PreMiO study. Oncotarget 8:79884–79896. https://doi.org/10.18632/oncotarget.20168
Attar A, Malka D, Sabate JM, Bonnetain F, Lecomte T, Aparicio T, Locher C, Laharie D, Ezenfis J, Taieb J (2012) Malnutrition is high and underestimated during chemotherapy in gastrointestinal cancer: an AGEO prospective cross-sectional multicenter study. Nutr Cancer 64:535–542. https://doi.org/10.1080/01635581.2012.670743
Walsh D, Szafranski M, Aktas A, Kadakia KC (2019) Malnutrition in cancer care: time to address the elephant in the room. J Oncol Pract 15:357–359. https://doi.org/10.1200/jop.19.00165
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Velasco C, Garcia E, Rodriguez V, Frias L, Garriga R, Alvarez J, Garcia-Peris P, Leon M (2011) Comparison of four nutritional screening tools to detect nutritional risk in hospitalized patients: a multicentre study. Eur J Clin Nutr 65:269–274. https://doi.org/10.1038/ejcn.2010.243
Dubhashi SP, Kayal A (2015) Preoperative nutritional assessment in elderly cancer patients undergoing elective surgery: MNA or PG-SGA? Indian J Surg 77:232–235. https://doi.org/10.1007/s12262-012-0780-5
Elia M (2003) The 'MUST' report. Nutritional screening for adults: a multidisciplinary responsibility. Development and use of the ‘Malnutrition Universal Screening Tool’ (MUST) for adults: BritishAssociation for Parenteral and Enteral Nutrition (BAPEN). In: Editor (ed)^(eds) Book The 'MUST' report. Nutritional screening for adults: a multidisciplinary responsibility. Development and use of the 'Malnutrition Universal Screening Tool' (MUST) for adults: BritishAssociation for Parenteral and Enteral Nutrition (BAPEN). City.
Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B (2001) Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci 56:M366-372. https://doi.org/10.1093/gerona/56.6.m366
Bonnefoy M, Jauffret M, Kostka T, Jusot JF (2002) Usefulness of calf circumference measurement in assessing the nutritional state of hospitalized elderly people. Gerontology 48:162–169. https://doi.org/10.1159/000052836
Selvaraj K, Jayalakshmy R, Yousuf A, Singh AK, Ramaswamy G, Palanivel C (2017) Can mid-upper arm circumference and calf circumference be the proxy measures to detect undernutrition among elderly? Findings of a community-based survey in rural Puducherry, India. J Family Med Prim Care 6:356–359. https://doi.org/10.4103/jfmpc.jfmpc_357_16
Maeda K, Koga T, Nasu T, Takaki M, Akagi J (2017) Predictive accuracy of calf circumference measurements to detect decreased skeletal muscle mass and European society for clinical nutrition and metabolism-defined malnutrition in hospitalized older patients. Ann Nutr Metab 71:10–15. https://doi.org/10.1159/000478707
Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, Klek S, Muscaritoli M, Nyulasi I, Ockenga J, Schneider SM, de van der Schueren MA, Singer P, (2015) Diagnostic criteria for malnutrition - an ESPEN consensus statement. Clin Nutr 34:335–340. https://doi.org/10.1016/j.clnu.2015.03.001
Holvoet E, Vanden Wyngaert K, Craenenbroeck A, Biesen W, Eloot S (2020) The screening score of Mini Nutritional Assessment (MNA) is a useful routine screening tool for malnutrition risk in patients on maintenance dialysis. PLoS ONE 15:e0229722. https://doi.org/10.1371/journal.pone.0229722
Ye XJ, Ji YB, Ma BW, Huang DD, Chen WZ, Pan ZY, Shen X, Zhuang CL, Yu Z (2018) Comparison of three common nutritional screening tools with the new European Society for Clinical Nutrition and Metabolism (ESPEN) criteria for malnutrition among patients with geriatric gastrointestinal cancer: a prospective study in China. BMJ Open 8:e019750. https://doi.org/10.1136/bmjopen-2017-019750
Sergeant, ESG (2018). In: Editor (ed)^(eds) Book, City, pp. Epitools Epidemiological Calculators. Ausvet.
McHugh ML (2012) Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 22:276–282
Shrout PE (1998) Measurement reliability and agreement in psychiatry. Stat Methods Med Res 7:301–317. https://doi.org/10.1177/096228029800700306
Yıldırım R, Candas B, Usta M, Erkul O, Türkyilmaz S, Guner A (2020) Comparison of nutritional screening tools in patients undergoing surgery for gastric cancer. Med Bull Haseki 58. https://doi.org/10.4274/haseki.galenos.2020.5779
Poulia KA, Klek S, Doundoulakis I, Bouras E, Karayiannis D, Baschali A, Passakiotou M, Chourdakis M (2017) The two most popular malnutrition screening tools in the light of the new ESPEN consensus definition of the diagnostic criteria for malnutrition. Clin Nutr 36:1130–1135. https://doi.org/10.1016/j.clnu.2016.07.014
Donini LM, Poggiogalle E, Molfino A, Rosano A, Lenzi A, Rossi Fanelli F, Muscaritoli M (2016) Mini-Nutritional Assessment, Malnutrition Universal Screening Tool, and Nutrition Risk Screening Tool for the Nutritional Evaluation of Older Nursing Home Residents. J Am Med Dir Assoc 17(959):e911-958. https://doi.org/10.1016/j.jamda.2016.06.028
Real GG, Fruhauf IR, Sedrez JHK, Dall’Aqua EJF, Gonzalez MC (2018) Calf circumference: a marker of muscle mass as a predictor of hospital readmission. JPEN J Parenter Enteral Nutr 42:1272–1279. https://doi.org/10.1002/jpen.1170
Baracos V, Kazemi-Bajestani SM (2013) Clinical outcomes related to muscle mass in humans with cancer and catabolic illnesses. Int J Biochem Cell Biol 45:2302–2308. https://doi.org/10.1016/j.biocel.2013.06.016
Lieffers JR, Bathe OF, Fassbender K, Winget M, Baracos VE (2012) Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer 107:931–936. https://doi.org/10.1038/bjc.2012.350
Trevethan R (2017) Sensitivity, specificity, and predictive values: foundations, pliabilities, and pitfalls in research and practice. Front Public Health 5:307. https://doi.org/10.3389/fpubh.2017.00307
Bhattacharjee A, Bahar I, Saikia A (2015) Nutritional assessment of patients with head and neck cancer in North-East India and dietary intervention. Indian J Palliat Care 21:289–295. https://doi.org/10.4103/0973-1075.164889
Sanchez-Lara K, Ugalde-Morales E, Motola-Kuba D, Green D (2013) Gastrointestinal symptoms and weight loss in cancer patients receiving chemotherapy. Br J Nutr 109:894–897. https://doi.org/10.1017/S0007114512002073
Jin S, Lu Q, Sun Y, Xiao S, Zheng B, Pang D, Yang P (2021) Nutrition impact symptoms and weight loss in head and neck cancer during radiotherapy: a longitudinal study. BMJ Support Palliat Care 11:17–24. https://doi.org/10.1136/bmjspcare-2019-002077
Cederholm T, Jensen GL, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T, Baptista G, Barazzoni R, Blaauw R, Coats A, Crivelli A, Evans DC, Gramlich L, Fuchs-Tarlovsky V, Keller H, Llido L, Malone A, Mogensen KM, Morley JE, Muscaritoli M, Nyulasi I, Pirlich M, Pisprasert V, de van der Schueren MAE, Siltharm S, Singer P, Tappenden K, Velasco N, Waitzberg D, Yamwong P, Yu J, Van Gossum A, Compher C, Committee GCL, Group GW (2019) GLIM criteria for the diagnosis of malnutrition - a consensus report from the global clinical nutrition community. Clin Nutr 38: 1-9. https://doi.org/10.1016/j.clnu.2018.08.002
Meissner C, Otto R, Fahlke J, Mueller M, Ridwelski K (2020) Relationship between nutritional status and length of hospital stay in oncological surgery. J Clin Oncol 38:e13591–e13591. https://doi.org/10.1200/JCO.2020.38.15_suppl.e13591
Pucciarelli S, Zorzi M, Gennaro N, Gagliardi G, Restivo A, Saugo M, Barina A, Rugge M, Zuin M, Maretto I, Nitti D (2017) In-hospital mortality, 30-day readmission, and length of hospital stay after surgery for primary colorectal cancer: a national population-based study. Eur J Surg Oncol 43:1312–1323. https://doi.org/10.1016/j.ejso.2017.03.003
Sousa IM, Bielemann RM, Gonzalez MC, da Rocha IMG, Barbalho ER, de Carvalho ALM, Dantas MAM, de Medeiros GOC, Silva FM, Fayh APT (2020) Low calf circumference is an independent predictor of mortality in cancer patients: a prospective cohort study. Nutrition 79–80:110816. https://doi.org/10.1016/j.nut.2020.110816
Kawakami R, Murakami H, Sanada K, Tanaka N, Sawada SS, Tabata I, Higuchi M, Miyachi M (2015) Calf circumference as a surrogate marker of muscle mass for diagnosing sarcopenia in Japanese men and women. Geriatr Gerontol Int 15:969–976. https://doi.org/10.1111/ggi.12377
Gonzalez MC, Mehrnezhad A, Razaviarab N, Barbosa-Silva TG, Heymsfield SB (2021) Calf circumference: cutoff values from the NHANES 1999–2006. Am J Clin Nutr. https://doi.org/10.1093/ajcn/nqab029
Acknowledgements
We sincerely thank Dr. Swaminathan Rajaram, Professor, Department of Tumor Registry and Biostatistics for helping us with the statistics and calculation of the sample size.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Dr. Nivedhyaa, Dr. Meenakshi, Dr. Thendral, Dr. Aishwarya, and Dr. Ajit. The first draft of the manuscript was written by Dr. Nivedhyaa, Dr. Meenakshi, and Dr. Kalpana. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The ethics approval was obtained from the institute ethics committee (IEC) (IEC 2019/Sept/01). The study was performed in accordance to the Declaration of Helsinki of 1975, revised in 2000.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable. Manuscript does not contain any individual images or videos.
Consent for publication
Not applicable. Manuscript does not contain any individual images or videos.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Srinivasaraghavan, N., Venketeswaran, M.V., Balakrishnan, K. et al. Comparison of nutrition screening tools and calf circumference in estimating the preoperative prevalence of malnutrition among patients with aerodigestive tract cancers—a prospective observational cohort study. Support Care Cancer 30, 6603–6612 (2022). https://doi.org/10.1007/s00520-022-07092-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07092-5