Abstract
Background
Treatment with immune checkpoint inhibitors (ICI) has greatly improved survival for patients with a number of malignant diseases in recent years. Neurological immune-related adverse events (n-irAE) of varying severity have been reported in the literature. We aimed to identify the incidence of n-irAE, focusing on immune-related encephalitis (IRE), in patients treated with ICI for multiple non-hematological malignancies in our institution.
Methods
All patients with histologically verified cancer that received treatment with ICI at the Sheba Medical Center between January 2017 and August 2019 were surveyed. Medical records for each patient were reviewed and information regarding n-irAE was recorded.
Results
In total, 1993 patients were included. Eleven cases of IRE were recorded, affecting 0.55% of patients overall, eight had non-melanoma cancer. Eight patients had made a full recovery.
Conclusions
IRE is a n-irAE more frequent than previously reported, particularly in non-melanoma patients. The diagnostic criteria and optimal treatment needs to be determined. ICI re-challenge after IRE can be considered for selected patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immunotherapy by checkpoint inhibitors (ICI) represents a great step forward in anticancer treatment. Numerous cancer types are treated by ICI, either as monotherapy or in combinations with different kinds of agents: tyrosine kinase inhibitors (TKIs), chemotherapies, different ICI, and radiotherapy [1].
Although ICI is very successful in eliminating cancer by promoting immune response against tumor-related antigens, the toxicity of ICI treatments is second only to its efficacy. Increased T cell and other parts of immune response activation by ICI therapy leads to immune-related adverse events (irAEs) that are frequent and lead to severe adverse events in a sizable proportion of patients (10–90% in recent surveys) with fatal events occurring at 0.3–1.3% of patients [2-4].
The spectrum of systemic irAE is different for each ICI agent: the most common reported pembrolizumab-induced toxicities are arthropathy, hepatitis, and pneumonitis; the most common nivolumab-induced toxicity is endocrinopathy; while ipilimumab mostly induces dermatological, GI, and renal toxicities [5]. In addition, there are reports that note different landscapes of toxicities according to the paradigm of ICI use: as a single agent, as combination with other ICI, or as combination with different agent classes [6–8]. The severity of adverse events seems to increase significantly in combined protocols [7-10].
The accumulated experience with ICI treatments in oncology has brought the understanding that ICI-induced toxicity usually has multi-organ impact and mostly develops during the first months of treatment [10]. In the case of anti CTLA-4 agents, the irAEs develop earlier and in a dose-dependent manner, but in case of anti PD-1 and PDl-1 agents, the irAEs develop later and in a dose-independent manner [7, 9]. The majority of irAEs are reversible and do not always demand treatment discontinuation [1, 8].
The incidence of organ damage as a side effect of ICI treatment is different across systems: dermatological toxicity, endocrinopathies, and visceral toxicity are common [7], while neurological irAEs (n-irAEs) are rare but harbor significant clinical complications [11, 12].
Several immune-related mechanisms were suggested as explanation for the pathophysiology of n-irAE [13–15]: ICI-induced anti-tumor immune response could produce cross-reactivity with CNS antigens, similarly to the pathogenesis of paraneoplastic syndromes; therapeutic antibodies could recognize their target molecules on resident CNS cells, and there is some evidence that ICI augments pre-existing CNS autoimmune responses [3].
After reviewing publications that address ICI n-irAE from the last 5 years, we conclude that while our awareness of n-irAE increased, there are different experiences of such events. Pan and Haggiagi [16] report n-irAE ranging from 1 to 6% for monotherapy and from 12 to 14% for combination therapy, based on three large works. Kao et al. 2017 [17] report 2.9% n-irAE on anti PD-1 treatment only, Cuzzubbo et al. 2017 [18] report, based on literature search of prospective clinical trials, n-irAE incidence in single use of anti CTLA-4 which was 3.8%, anti PD-1 which was 6.1%, and 12% n-irAE in ICI combination. Spain et al. [8] report on a melanoma cohort with an overall incidence of n-irAE in 2.8% of patients, anti CTLA-4 1%, anti PD-1 3% and combination reaching 14% n-irAE. ASCO practice guideline for the management of irAEs [19] cited the same numbers as the Cuzzubbo group. Bruna et al. [20] report a 2% incidence of n-irAE in their multi-malignancy cohort.
Encephalopathy, diffuse or/and focal brain dysfunction, is a common clinical situation in cancer patients. The clinical picture varies and includes mental, speech, and behavioral disturbances; epileptic seizures; involuntary movements; motor and sensory abnormality; gaze and eye movement disturbances. As in others group of patients, the etiological variability of encephalopathy in cancer patients is wide: metabolic, inflammatory, toxic, tumorous, vascular, and even degenerative. In some patient, an encephalopathy has multifactorial etiology. Encephalitis is an inflammatory brain disorder with acute or subacute onset; encephalopathy is often part of the clinical picture of encephalitis.
Galmiche et al. [21] report specifically on an immune-related encephalitis (IRE) as n-irAE with an incidence of 2.3% in a melanoma cohort. The reported incidence of encephalitis as n-irAE is 0.1–0.2% of all n-irAE but reach 19% of high-grade n-irAE [18, 19].
The landscape of n-irAE is diverse and involves all parts of the nervous system. Few information exists about dissimilarity of n-irAE profile between melanoma and non-melanoma cancer in general [7] and only one, to our knowledge, recently published [22] review addressed the possibility of change in landscape of n-irAE when ICI use was extended to “non-melanoma” cancers.
We would like to call the attention of the neuro-oncology community to the change in n-irAEs related to the movement from an era of “predominantly melanoma ICI use”, where most n-irAEs were neuro-muscular disturbances [23], to possibly different patterns of incidence in non-melanoma patients [7].
We describe our experience with IRE as n-irAE in ICI-treated patients with non-hematological malignancies in our institute.
Methods
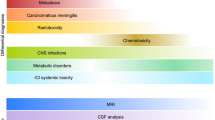
Patients treated at the Institute of Oncology in Sheba Tel HaShomer Medical Center during 2017–2019, with ICI, were identified from electronic medical record. All patients with new neurological symptoms, that developed during ICI treatment and were recognized by treating oncologists, were discussed with or personally examined by neuro-oncology team’s neurologist and underwent appropriate diagnostic procedures, according to standard of care. If there were any acute or subacute brain dysfunctions, in these patients, they were qualified as encephalitis after ruling out of other etiologies. Patients treated for IRE were identified from the working database of the Neuro-Oncology Unit of the Institute, and their charts were manually reviewed.
Treatment protocol
Five patients received standard therapy, while six patients were part of a clinical trial that included ICIs as the drug being investigated, or as baseline therapy with an additional investigational drug.
Results
One thousand nine hundred ninety-three patients were treated with ICI in our hospital between the years 2017 and 2019; most of them were melanoma patients (Table 1). The profile of n-irAE according to disease, grouped as melanoma or non-melanoma, is shown in Table 4. Out of these patients, 11 were diagnosed with ICI-induced encephalitis (IRE): patients’ characteristics are presented in Table 2 and clinical presentation symptoms are described in Table 3. Four additional patients receiving ICI had multi-organ irAEs with numerous concomitant brain pathologies (brain metastasis and previous ischemic damage), and in these cases, the possibility of IRE was in the differential diagnosis. Of the 11 patients that developed IRE, four patients received ICI as monotherapy, two patients received ICI combinations, four patients were treated by combination with chemotherapy, and one patient received ICI in combination with TKI. Five patients additionally suffered from non-neurological ICI toxicities: one patient had fatigue, two patients had skin toxicity, one patient had adrenal damage, and one patient had hepatitis.
The onset of clinical picture in these cases varied from 5 to 210 days from ICI start, with a median onset time of 20 days. The neurological picture was variable (Table 3). The most common symptom was confusional state (six patients), four patients presented with epileptic events (3 generalized and 1 partial), and three patients developed speech disturbances; headache and ataxia were seen in two patients each, while psychotic state, tremor, and opsoclonus were each seen in a single patient. The grade of disability was significant; the score according to modified Rankin Scale (mRS) was 5/4/3 points in 4/3/4 of the patients, respectively. All patients had high-grade AEs. In all but one patient (N7), the brain imaging (CT and MRI) was normal; the abnormal brain MRI had multiple white and gray matter abnormalities.
CSF examinations revealed mild protein elevation in 90% of patients and lymphocytic pleocytosis in 54.5% of patients (Table 3). Paraneoplastic antibodies were tested in 7 patients, using recombinant line assay, and all were found to be negative.
All except for one patient (N2) were treated with methylprednisolone pulse (1 g/day 5 days) followed by at least 4 weeks of prednisolone 1 mg/kg with slow tapering down. Two patients were treated with a second-line treatment: one patient with plasma exchange (N7) and one patient with plasma exchange and cyclophosphamide (N3). The patients that received only high-dose steroidal treatment responded within the first 5 days.
One patient (N2) received only low-dose steroids because of his advanced age (87 years old), and this patient died in hospice care 2 months later.
The neurological outcome was as follows (Table 3): two patients (N2 and N7) died from encephalitis. The mRS score in other patients was 1/3/0 points in 3/2/4 of the patients, respectively. Two patients, N3 and N7, recurred during steroid tapering off period. Patient N3 improved again after high-dose steroid re-treatment, while patient N7 continued to deteriorate and died despite treatment.
Oncological outcome for patients that survived IRE was good in 63.6% of patients. Only four patients had disease progression. Patient N1 with SCLC progressed 56 days after ICI discontinuation, and was treated with palliative care at recurrence. Patient N3 with uterine carcinoma progressed 150 days after ICI discontinuation and was treated with additional line of chemotherapy but died from disease progression; two other melanoma patients (N5 and N6) progressed 60 and 730 days after ICI discontinuation. Both of them were treated with ICI re-challenge: previous ICI with low-dose steroids (patient N5) and different ICI (patient N6). Both patients had partial response followed by stable disease without any neurological complications.
Postmortem evaluation was not performed on any one of the patients who died from IRE or cancer.
Discussion
Immune-related encephalitis (IRE) is not as common as other irAEs but we find that it is more frequent than previously reported. According to our data, the frequency of IRE is 0.55% and not 0.2% as was previously reported [21].
Similar to previous reports [24], 80% of our IRE cases (9/11) developed the clinical picture within 4 months from ICI treatment onset.
Analysis of our data and the currently available literature leads to several points of discussion.
First, nervous system ICI toxicity profile might be different between cancer types. Previous reports, mostly from melanoma patient cohorts, find more PNS than CNS n-irAE (e.g., Spain et al. [24] reporting 70% PNS and 30% CNS), and indeed in our melanoma patient cohort, 76% of n-irAE involved PNS (13/17). However, from our experience in non-melanoma cancer patients, 80% of n-irAE involve the CNS (17/21) (Table 4). In cohort described by Vogrig et al. [25], where most patients were with NSCLC, similar proportions were described.
The pathophysiological mechanism of ICI n-irAE and paraneoplastic syndrome could be partially similar. An analogy of the situation with different incidence of paraneoplastic syndromes in different kinds of cancers could be done. The reported incidence of neurological paraneoplastic syndromes in melanoma is low [13, 26]. At the same time, in lung (especially small cell lung cancer), gynecological malignancies are significantly higher [13, 26]. The same tendency was observed, according to our data, in distribution of the incidences of encephalitis as ICI n-irAE. Among melanoma cancer patients, the incidence of encephalitis as ICI n-irAE was relatively low in comparison to incidence of this n-irAE among non-melanoma cancer patients. In light of that, the relatively high incidence of encephalitis as ICI n-irAEs in the population of genitourinary cancer patients is surprising and will be better understood in future studies.
An additional explanation for different toxicity profile, between cancer types, could be due to different treatment approaches in different cancer types. As previously reported, the incidence of ICI irAEs is higher when ICI is used in combination with other agents. Combination of ICI with non-IPI agents is not used for treatment of melanoma cancer but they are used for the treatment of non-melanoma cancers. This approach might explain the increase in incidence of encephalitis, as ICI n-irAE, in some non-melanoma cancer patients, but not in genitourinary cancer patients.
Secondly, according to the data published by Vogrig et al. [22], paraneoplastic antibodies were positive in about 60% of patients with encephalitis as an ICI n-irAE, but other authors reported that in most patients with encephalitis, the paraneoplastic antibodies were negative with the exception of a few cases that were positive for anti NMDA antibodies [21, 27]. 63.6% of our patients were tested for paraneoplastic antibodies and were negative. The paraneoplastic antibody positivity in n-irAE patients is different probably due to different methods of testing. Evaluation of paraneoplastic antibody positivity as pre-treatment evaluation is currently not a common practice. Additionally, no consensus exists regarding the significance of follow-up, of these antibodies levels, in positive patients as a marker of treatment efficacy or oncological disease activity. Only sporadic studies addressed this topic [28]. It is possible that testing for paraneoplastic antibodies, prior to ICI therapy, will reveal the patients at risk to develop the ICI n-irAEs, even though only part of the patients that had paraneoplastic antibodies prior to ICI treatment continued to develop n-irAEs [28].
In recent years, providing a good quality of life for oncological patients, during treatment, has become an additional important treatment outcome. The neurological deficits, caused by nervous system damage, could significantly impair patients’ quality of life. They warrant increased awareness and attention of oncologists to neurological symptoms during treatment visits. The increased awareness of n-irAE might have influenced the increased number of reported cases of n-irAE.
The diagnosis of IRE remains a challenge and continues to be a diagnosis of exclusion. We did not find, in the literature, any specific (clinical, laboratory, or imaging) diagnostic criteria for IRE. As most patients with n-irAE have multi-system toxicity, it is possible that in cases with high-grade visceral toxicity, where metabolic disturbances are prominent, the signs of encephalopathy are not rare. This raises the possibility that patients diagnosed as non-neurological irAE might have nervous system toxicity as well, but accurate diagnosis was not possible. Therefore, it is possible that the real incidence of IRE is higher.
The treatment of IRE is based on experts’ opinion [11, 29] and for now is identical to non-ICI-related autoimmune encephalitis. From our experience, high-dose steroids are a sufficient treatment for the majority of patients and the response to this treatment could be a prognostic factor of recovery. The best second-line treatment and the right time for switching treatment lines are not known yet. The optimal duration of steroid treatment is also unknown. For our patients, after the completion of pulse methylprednisolone, prednisone treatment was prescribed for 1 month on average with slow tapering down.
The question of ICI re-challenge, following IRE, is very relevant. For most of our patients, IRE was a reversible condition, even though 18% of our patients died as a result of IRE (2 patients). When considering that ICI is the best or only oncological treatment, physicians need to make a calculated risk evaluation. We report that in our cohort, out of four progressed patients, two melanoma patients were treated with ICI re-challenge with no complication. Due to the small number of patients, we do not have the right tools to make a risk assessment conclusion.
Conclusion
We conclude that the real incidence of encephalitis as ICI n-irAE is higher than was previously suggested. We further conclude that the evolution of symptoms may be rapid and life-threatening, requiring early diagnosis and treatment decisions. Some patients with ICI-induced toxicity suffer from multi-system damages, which may mask a clinical picture of IRE.
So far, the diagnosis of IRE is clinical and per exclusion, and further research is needed in order to establish diagnostic criteria, optimal intervention, and calculated re-challenge to ICI treatment.
Prospective multi center studies with multidisciplinary approach are needed in order to define preventive and diagnostic criteria and establish the best treatment of this dangerous ICI complication.
Data availability
All data and material are available in uploaded tables; additional data that was not used in the tables are available on demand.
References
Postow MA, Sidlow R, Hellmann MD (2018) Immune-related adverse events associated with immune checkpoint blockade. N Engl J Med 378(2):158–168. https://doi.org/10.1056/NEJMra1703481
Dalmau J (2018) Looks can be deceiving: A B-cell–mediated encephalopathy with normal MRI? Neurol - Neuroimmunol Neuroinflammation 5(3):e461. https://doi.org/10.1212/NXI.0000000000000461
Yshii LM, Hohlfeld R, Liblau RS (2017) Inflammatory CNS disease caused by immune checkpoint inhibitors: status and perspectives. Nat Rev Neurol 13(12):755–763. https://doi.org/10.1038/nrneurol.2017.144
Diesendruck Y, Benhar I (2017) Novel immune check point inhibiting antibodies in cancer therapy—opportunities and challenges. Drug Resist Updat 2017(30):39–47. https://doi.org/10.1016/j.drup.2017.02.001
Martins F, Sofiya L, Sykiotis GP et al (2019) Adverse effects of immune-checkpoint inhibitors: epidemiology, management and surveillance. Nat Rev Clin Oncol 16(9):563–580. https://doi.org/10.1038/s41571-019-0218-0
Kennedy LB, Salama AKS (2020) A review of cancer immunotherapy toxicity. CA Cancer J Clin 70(2):86–104. https://doi.org/10.3322/caac.21596
Khoja L, Day D, Wei-Wu Chen T, Siu LL, Hansen AR (2017) Tumour- and class-specific patterns of immune-related adverse events of immune checkpoint inhibitors: a systematic review. Ann Oncol 28(10):2377–2385. https://doi.org/10.1093/annonc/mdx286
Spain L, Walls G, Julve M, O’Meara K, Schmid T, Kalaitzaki E, Turajlic S, Gore M, Rees J, Larkin J (2017) Neurotoxicity from immune-checkpoint inhibition in the treatment of melanoma: a single centre experience and review of the literature. EGFR Mutat Adv non-small-cell lung cancer overall Surviv data from LUX-Lung 7 trial Annals of Oncology 28: 377–385. https://doi.org/10.1093/annonc/mdw558
Sosa A, Lopez Cadena E, Simon Olive C, Karachaliou N, Rosell R (2018) Clinical assessment of immune-related adverse events. Ther Adv Med Oncol 10:1–11. https://doi.org/10.1177/1758835918764628
Genova C, Rossi G, Rijavec E et al (2017) Releasing the brake: safety profile of immune check-point inhibitors in non-small cell lung cancer. Expert Opin Drug Saf 16(5):573–585. https://doi.org/10.1080/14740338.2017.1313228
Haanen JBAG, Carbonnel F, Robert C et al (2017) Management of toxicities from immunotherapy: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 28(Supplement 4):iv119–iv142. https://doi.org/10.1093/annonc/mdx225
Thompson JA, Schneider BJ, Brahmer J et al (2019) Management of immunotherapy-related toxicities, version 1.2019. JNCCN J Natl Compr Cancer Netw 17(3):255–289. https://doi.org/10.6004/jnccn.2019.0013
Graus F, Dalmau J (2019) Paraneoplastic neurological syndromes in the era of immune-checkpoint inhibitors. Nat Rev Clin Oncol 16(9):535–548. https://doi.org/10.1038/s41571-019-0194-4
Dalakas MC (2018) Neurological complications of immune checkpoint inhibitors: what happens when you ‘take the brakes off’ the immune system. Ther Adv Neurol Disord 11:1–9. https://doi.org/10.1177/1756286418799864
Fellner A, Makranz C, Lotem M et al (2018) Neurologic complications of immune checkpoint inhibitors. J Neurooncol 137(3):601–609. https://doi.org/10.1007/s11060-018-2752-5
Pan PC, Haggiagi A (2019) Neurologic immune-related adverse events associated with immune checkpoint inhibition. Curr Oncol Rep 21:108
Kao JC, Liao B, Markovic SN et al (2017) Neurological complications associated with anti–programmed death 1 (PD-1) antibodies. JAMA Neurol 74(10):1216–1222. https://doi.org/10.1001/jamaneurol.2017.1912
Cuzzubbo S, Javeri F, Tissier M, Roumi A, Barlog C (2017) ScienceDirect Neurological adverse events associated with immune checkpoint inhibitors: review of the literature. Eur J Cancer 73:1–8. https://doi.org/10.1016/j.ejca.2016.12.001
Brahmer JR, Lacchetti C, Schneider BJ et al (2018) Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American society of clinical oncology clinical practice guideline. J Clin Oncol 36(17):1714–1768. https://doi.org/10.1200/JCO.2017.77.6385
Bruna J, Argyriou AA, Alemany M et al (2020) Incidence and characteristics of neurotoxicity in immune checkpoint inhibitors with focus on neuromuscular events: experience beyond the clinical trials. J Peripher Nerv Syst 25(1):171–177. https://doi.org/10.1111/jns.12371
Galmiche S, Lheure C, Kramkimel N et al (2019) Encephalitis induced by immune checkpoint inhibitors in metastatic melanoma: a monocentric retrospective study. J Eur Acad Dermatology Venereol 33(12):e440–e443. https://doi.org/10.1111/jdv.15756
Vogrig A, Muñiz-Castrillo S, Joubert B, Picard G, Rogemond V, Marchal C, Chiappa AM, Chanson E, Skowron F, Leblanc A, Ducray F, Honnorat J (2020) Central nervous system complications associated with immune checkpoint inhibitors. J Neurol Neurosurg Psychiatry 91(7):772–778. https://doi.org/10.1136/jnnp-2020-323055
Larkin J, Chmielowski B, Lao CD et al (2017) Neurologic serious adverse events associated with nivolumab plus ipilimumab or nivolumab alone in advanced melanoma, including a case series of encephalitis. Oncologist 22(6):709–718. https://doi.org/10.1634/theoncologist.2016-0487
Spain L, Walls G, Julve M et al (2017) Neurotoxicity from immune-checkpoint inhibition in the treatment of melanoma: a single centre experience and review of the literature. Ann Oncol 28(2):377–385. https://doi.org/10.1093/annonc/mdw558
Vogrig A, Muñiz-Castrillo S, Desestret V, Joubert B, Honnorat J (2020) Pathophysiology of paraneoplastic and autoimmune encephalitis: genes, infections, and checkpoint inhibitors. Ther Adv Neurol Disord 13:1–15. https://doi.org/10.1177/1756286420932797
Leypoldt F, Wandinger KP (2014) Paraneoplastic neurological syndromes. Clin Exp Immunol 175(3):336–348. https://doi.org/10.1111/cei.12185
Zekeridou A, Lennon VA (2019) Neurologic autoimmunity in the era of checkpoint inhibitor cancer immunotherapy. Mayo Clin Proc 94(9):1865–1878. https://doi.org/10.1016/j.mayocp.2019.02.003
Hardy-Werbin M, Arpí O, Taus A et al (2018) Assessment of neuronal autoantibodies in patients with small cell lung cancer treated with chemotherapy with or without ipilimumab. Oncoimmunology 7(2):e1395125. https://doi.org/10.1080/2162402X.2017.1395125
Spain L, Tippu Z, Larkin J, Carr A, Turajlic S (2019) How we treat neurological toxicity from immune checkpoint inhibitors. ESMO Open 4(e540):1–5. https://doi.org/10.1136/esmoopen-2019-000540
Author information
Authors and Affiliations
Contributions
The first author personally examined and treated the patients. The first, second, and last authors took part in writing the manuscript. All authors, except for the first and second, are treating oncologists and took part in editing the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The local Ethics Committee of Sheba Tel Hashomer MC waived ethical approval in view of the retrospective nature of the study, and all the procedures being performed were part of the routine care.
Consent to participate
All authors agreed to participate in this manuscript.
Consent for publication
All authors agreed to publish the manuscript.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Taliansky, A., Furman, O., Gadot, M. et al. Immune checkpoint inhibitors–related encephalitis in melanoma and non-melanoma cancer patients: a single center experience. Support Care Cancer 29, 7563–7568 (2021). https://doi.org/10.1007/s00520-021-06331-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06331-5