Abstract
Background
The Global Leadership Initiative on Malnutrition (GLIM) has the potential to gain global acceptance for diagnosing malnutrition. Of which, calf circumference (CC) was proposed as an alternative to evaluate the reduced muscle mass (RMM). The present study aimed to evaluate whether including the hand grip strength (HGS) was helpful for diagnosing malnutrition under the GLIM framework.
Methods
We performed a multicenter, observational cohort study including 3998 patients with cancer at two teaching hospitals. The RMM criterion was separately assessed using the calf circumference (CC), or the CC and HGS combined. Accordingly, two methods of GLIM diagnosis were independently developed to determine the nutritional status of the patients. The diagnostic concordance, baseline characteristics, and outcomes of patients were compared across the malnourished-CC-HGS, malnourished-CC+HGS, and well-nourished groups. The Patient-Generated Subjective Global Assessment (PG-SGA) was used as a comparator to identify the optimal method.
Results
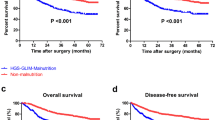
Malnutrition was identified in 1120 (28%) patients by the CC method and 1060 (26.5%) patients by the CC+HGS method. Compared to the well-nourished group, the malnourished-CC+HGS group (60 patients, 1.5%) had poorer nutritional characteristics, poorer Karnofsky Performance Status scores, poorer global quality of life scores, and higher Nutritional Risk Screening 2002 scores. The severity of malnutrition diagnosed using the CC method (Kappa = 0.136) showed higher agreement with the PG-SGA than the CC+HGS method (Kappa = 0.127).
Conclusion
Compared to CC+HGS, the CC alone appears to be adequate to evaluate RMM under the GLIM framework. A simpler method might facilitate the application of these criteria in clinical settings by increasing efficacy and minimizing missed diagnoses.



Similar content being viewed by others
Data availability
N/A.
Abbreviations
- GLIM:
-
Global Leadership Initiative on Malnutrition
- HGS:
-
Hand grip strength
- CC:
-
Calf circumference
- QOL:
-
Quality of life
- PG-SGA:
-
Patient-Generated Subjective Global Assessment
- AMC:
-
Arm muscle circumference
- RMM:
-
Reduced muscle mass
- INSCOC:
-
Investigation on Nutrition Status and its Clinical Outcome of Common Cancers
- KPS:
-
Karnofsky Performance Status
- MAC:
-
Mid-arm circumference
- TSF:
-
Triceps skinfold thickness
- p5:
-
Fifth percentile
- p15:
-
15th percentile
- COPD:
-
Chronic obstructive pulmonary disease
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J (2016) Cancer statistics in China, 2015. CA Cancer J Clin 66:115–132
Li Z, Chen W, Li H, Zhao B, Chinese Oncology Nutrition Survey G (2018) Nutrition support in hospitalized cancer patients with malnutrition in China. Asia Pac J Clin Nutr 27:1216–1224
Bell CL, Tamura BK, Masaki KH, Amella EJ (2013) Prevalence and measures of nutritional compromise among nursing home patients: weight loss, low body mass index, malnutrition, and feeding dependency, a systematic review of the literature. J Am Med Dir Assoc 14:94–100
Gioulbasanis I, Baracos VE, Giannousi Z, Xyrafas A, Martin L, Georgoulias V, Mavroudis D (2011) Baseline nutritional evaluation in metastatic lung cancer patients: mini nutritional assessment versus weight loss history. Ann Oncol 22:835–841
Almasaudi AS, McSorley ST, Dolan RD, Edwards CA, McMillan DC (2019) The relation between Malnutrition Universal Screening Tool (MUST), computed tomography-derived body composition, systemic inflammation, and clinical outcomes in patients undergoing surgery for colorectal cancer. Am J Clin Nutr 110:1327–1334
Li R, Wu J, Ma M, Pei J, Song Y, Zhang X, Han B (2011) Comparison of PG-SGA, SGA and body-composition measurement in detecting malnutrition among newly diagnosed lung cancer patients in stage IIIB/IV and benign conditions. Med Oncol 28:689–696
Vangelov B, Venchiarutti RL, Smee RI (2017) Critical weight loss in patients with oropharynx cancer during radiotherapy (+/- chemotherapy). Nutr Cancer 69:1211–1218
Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, Fearon K, Hütterer E, Isenring E, Kaasa S, Krznaric Z, Laird B, Larsson M, Laviano A, Mühlebach S, Muscaritoli M, Oldervoll L, Ravasco P, Solheim T, Strasser F, de van der Schueren M, Preiser JC (2017) ESPEN guidelines on nutrition in cancer patients. Clin Nutr 36:11–48
Pressoir M, Desne S, Berchery D, Rossignol G, Poiree B, Meslier M et al (2010) Prevalence, risk factors and clinical implications of malnutrition in French Comprehensive Cancer Centres. Br J Cancer 102:966–971
Hu WH, Eisenstein S, Parry L, Ramamoorthy S (2019) Preoperative malnutrition with mild hypoalbuminemia associated with postoperative mortality and morbidity of colorectal cancer: a propensity score matching study. Nutr J 18:33
Torricelli P, Antonelli F, Ferorelli P, Borromeo I, Shevchenko A, Lenzi S, de Martino A (2020) Oral nutritional supplement prevents weight loss and reduces side effects in patients in advanced lung cancer chemotherapy. Amino Acids 52:445–451
Aaldriks AA, van der Geest LG, Giltay EJ, le Cessie S, Portielje JE, Tanis BC et al (2013) Frailty and malnutrition predictive of mortality risk in older patients with advanced colorectal cancer receiving chemotherapy. J Geriatr Oncol 4:218–226
Yamano T, Yoshimura M, Kobayashi M, Beppu N, Hamanaka M, Babaya A, Tsukamoto K, Noda M, Matsubara N, Tomita N (2016) Malnutrition in rectal cancer patients receiving preoperative chemoradiotherapy is common and associated with treatment tolerability and anastomotic leakage. Int J Color Dis 31:877–884
Zhang X, Pang L, Sharma SV, Li R, Nyitray AG, Edwards BJ (2019) Prevalence and factors associated with malnutrition in older patients with cancer. J Geriatr Oncol 10:763–769
Brinksma A, Sanderman R, Roodbol PF, Sulkers E, Burgerhof JG, de Bont ES et al (2015) Malnutrition is associated with worse health-related quality of life in children with cancer. Support Care Cancer 23:3043–3052
Yang J, Zhang Q, Wang X (2018) Role of nutritional support for postoperative recovery of respiratory function in patients with primary lung cancer. Oncol Lett 16:5978–5982
Tagawa M, Myotoku M, Iwamoto C, Senaha H, Urashima Y, Hirotani Y, Imanaka N, Imanishi N, Hayashi M, Fukuzaki T, Azama T (2013) Nutritional assessment employing the malnutrition universal screening tool for patients with colorectal cancer undergoing outpatient chemotherapy. Gan To Kagaku Ryoho 40:1185–1188
Trabal J, Leyes P, Forga M, Maurel J (2010) Potential usefulness of an EPA-enriched nutritional supplement on chemotherapy tolerability in cancer patients without overt malnutrition. Nutr Hosp 25:736–740
Cederholm T, Jensen GL, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T et al (2019) GLIM criteria for the diagnosis of malnutrition - a consensus report from the global clinical nutrition community. Clin Nutr 38:1–9
Allard JP, Keller H, Gramlich L, Jeejeebhoy KN, Laporte M, Duerksen DR (2020) GLIM criteria has fair sensitivity and specificity for diagnosing malnutrition when using SGA as comparator. Clin Nutr 39:2771–2777
Maeda K, Ishida Y, Nonogaki T, Mori N (2020) Reference body mass index values and the prevalence of malnutrition according to the Global Leadership Initiative on Malnutrition criteria. Clin Nutr 39:180–184
Contreras-Bolivar V, Sanchez-Torralvo FJ, Ruiz-Vico M, Gonzalez-Almendros I, Barrios M, Padin S et al (2019) GLIM criteria using hand grip strength adequately predict six-month mortality in cancer inpatients. Nutrients 11:2043
Yin L, Lin X, Li N, Zhang M, He X, Liu J et al (2020) Evaluation of the global leadership initiative on malnutrition criteria using different muscle mass indices for diagnosing malnutrition and predicting survival in lung cancer patients. JPEN J Parenter Enteral Nutr. https://doi.org/10.1002/jpen.1873
Xu HX, Song CH, Wang C, Fu ZM, Guo ZQ, Lin Y et al (2020) Investigation on nutrition status and clinical outcome of patients with common cancers in Chinese patients: a multicenter prospective study protocol. Int J Clin Trials 7:94–10
Kondrup J, Allison SP, Elia M, Vellas B, Plauth M, Educational et al (2003) ESPEN guidelines for nutrition screening 2002. Clin Nutr 22:415–421
Wan C, Meng Q, Yang Z, Tu X, Feng C, Tang X, Zhang C (2008) Validation of the simplified Chinese version of EORTC QLQ-C30 from the measurements of five types of inpatients with cancer. Ann Oncol 19:2053–2060
Murri R, Scoppettuolo G, Damiano F, Ammassari A, Fantoni M, Antinori A (1996) Karnofsky performance status and assessment of global health status. J Acquir Immune Defic Syndr Hum Retrovirol 13:294–295
Ottery FD (1994) Rethinking nutritional support of the cancer patient: the new field of nutritional oncology. Semin Oncol 21:770–778
Jager-Wittenaar H, Ottery FD (2017) Assessing nutritional status in cancer: role of the Patient-Generated Subjective Global Assessment. Curr Opin Clin Nutr Metab Care 20:322–329
Chen C, Lu FC, Department of Disease Control Ministry of Health PRC (2004) The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci 17(Suppl):1–36
Buzby GP, Knox LS, Crosby LO, Eisenberg JM, Haakenson CM, McNeal GE et al (1988) Study protocol: a randomized clinical trial of total parenteral nutrition in malnourished surgical patients. Am J Clin Nutr 47:366–381
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Keller H, de van der Schueren MAE, Consortium G, Jensen GL, Barazzoni R, Compher C et al (2020) Global Leadership Initiative on Malnutrition (GLIM): guidance on validation of the operational criteria for the diagnosis of protein-energy malnutrition in adults. JPEN J Parenter Enteral Nutr 44:992–1003
Kawakami R, Murakami H, Sanada K, Tanaka N, Sawada SS, Tabata I, Higuchi M, Miyachi M (2015) Calf circumference as a surrogate marker of muscle mass for diagnosing sarcopenia in Japanese men and women. Geriatr Gerontol Int 15:969–976
Akin S, Mucuk S, Ozturk A, Mazicioglu M, Gocer S, Arguvanli S et al (2015) Muscle function-dependent sarcopenia and cut-off values of possible predictors in community-dwelling Turkish elderly: calf circumference, midarm muscle circumference and walking speed. Eur J Clin Nutr 69:1087–1090
Kusaka S, Takahashi T, Hiyama Y, Kusumoto Y, Tsuchiya J, Umeda M (2017) Large calf circumference indicates non-sarcopenia despite body mass. J Phys Ther Sci 29:1925–1928
Abro A, Delicata LA, Vongsanim S, Davenport A (2018) Differences in the prevalence of sarcopenia in peritoneal dialysis patients using hand grip strength and appendicular lean mass: depends upon guideline definitions. Eur J Clin Nutr 72:993–999
Tangvoraphonkchai K, Hung R, Sadeghi-Alavijeh O, Davenport A (2018) Differences in prevalence of muscle weakness (sarcopenia) in haemodialysis patients determined by hand grip strength due to variation in guideline definitions of sarcopenia. Nutr Clin Pract 33:255–260
Masanes F, Rojano ILX, Salva A, Serra-Rexach JA, Artaza I, Formiga F et al (2017) Cut-off points for muscle mass - not grip strength or gait speed - determine variations in sarcopenia prevalence. J Nutr Health Aging 21:825–829
Ha YC, Yoo JI, Park YJ, Lee CH, Park KS (2018) Measurement of uncertainty using standardized protocol of hand grip strength measurement in patients with sarcopenia. J Bone Metab 25:243–249
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, Chou MY, Chen LY, Hsu PS, Krairit O, Lee JSW, Lee WJ, Lee Y, Liang CK, Limpawattana P, Lin CS, Peng LN, Satake S, Suzuki T, Won CW, Wu CH, Wu SN, Zhang T, Zeng P, Akishita M, Arai H (2014) Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc 15:95–101
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31
Acknowledgments
We thank all of the committee and board members of the Chinese Society of Nutritional Oncology (CSNO). We would also like to thank WINCOME Computer and Technology Corporation for establishing the Electronic Data Capture (EDC) System for the present study. We also thank the INSCOC project members for their substantial work on data collection and patient follow-up.
Funding
This work was supported by the National Natural Science Foundation of China (81673167, Hongxia Xu), the Chongqing Technology Innovation and Application Demonstration Project for Social Livelihood (cstc2018jscx-msybX0094, Jie Liu), and the National Key Research and Development Program (2017YFC1309200, Hanping Shi).
Author information
Authors and Affiliations
Contributions
LYY, JL, CHS, HPS, and HXX designed the research; LYY and HXX conducted the research; LYY performed the statistical analysis and wrote the manuscript; XL, ZPZ, NL, XMH, MYZ, JY, ZQG, ZNL, KHW, MW, MHC, SYL, TL, HM, YB, WL, and JWC critically reviewed the manuscript; and all authors interpreted the data, provided critical input, and read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The study protocol was approved by the institutional review board at Daping Hospital (no. 2018-22).
Consent to participate
All patients provided written consent for the scientific use of their data.
Consent for publication
N/A.
Code availability
N/A.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 19 kb)
Rights and permissions
About this article
Cite this article
Yin, L., Lin, X., Zhao, Z. et al. Is hand grip strength a necessary supportive index in the phenotypic criteria of the GLIM-based diagnosis of malnutrition in patients with cancer?. Support Care Cancer 29, 4001–4013 (2021). https://doi.org/10.1007/s00520-020-05975-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05975-z