Abstract
Background
Breast cancer (BC) is the most common cancer among women in developed countries. Several types of surgical interventions are commonly used in BC, such as mastectomy and quadrantectomy, followed by radiation or not. Today, BC rehabilitation can help survivors obtain and maintain the highest physical, social, psychological, and vocational functioning possible, within the limits that are created by cancer and its treatments.
Objective
To verify, before and after a specific rehabilitation protocol treatment, the recovery of the fluidity of the reaching movement.
Methods
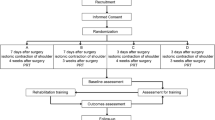
Patients after BC surgery were enrolled and assigned by cluster randomization into 2 groups through a block randomization list: mastectomy (Mas) and quadrantectomy (Quad). Evaluation scales (DASH and VAS) were administered, and biomechanical evaluations were performed for each group before treatment (T0 = baseline), at the end of the rehabilitative treatment (T1 = 12 sessions, 2/week), and after 3 months of follow-up (T2).
Results
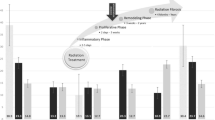
Fifty-nine (Mas group = 29; Quad group = 30) after BC surgery were enrolled. VAS scores improved along the evaluation times at T0–T1 and T0–T2 (p < 0.001), without a statistically significant difference between groups. With regard to the normalized jerk, there was no significant interaction between time group (F = 2.029; p = 0.136). There was a significant decrease between T0–T1 and T1–T2 (F = 60.189; p < 0.001). Velocity improved significantly between T0–T1 and T1–T2 (F = 10.322; p < 0.001). There was a significant interaction for the elbow angle at the end of movement between time and group at T2 (F = 5.022; p = 0.029).
Conclusion
The integrated, low-intensity, rehabilitative intervention is effective, even if it is not performed in the first period after BC surgery, without any difference between mastectomy and quadrantectomy.



Similar content being viewed by others
References
Fisher B, Jeong JH, Anderson S, Bryant J, Fisher ER, Wolmark N (2002) Twenty-five-year follow-up of a randomized trial comparing radical mastectomy, total mastectomy, and total mastectomy followed by irradiation. N Engl J Med 347(8):567–575
Sada A, Day CN, Hoskin TL, Degnim AC, Habermann EB, Hieken TJ (2019) Mastectomy and immediate breast reconstruction in the elderly: trends and outcomes. Surgery
Puliti D, Bucchi L, Mancini S, Paci E, Baracco S, Campari C, Canuti D, Cirilli C, Collina N, Conti GM, Di Felice E, Falcini F, Michiara M, Negri R, Ravaioli A, Sassoli De’ Bianchi P, Serafini M, Zorzi M, Caldarella A, Cataliotti L, Zappa M, IMPACT COHORT Working Group (2017) Advanced breast cancer rates in the epoch of service screening: the 400,000 women cohort study from Italy. Eur J Cancer 75:109–116
Corso G, Veronesi P, Sacchini V, Galimberti V, Luini A (2017) The Veronesi quadrantectomy: an historical overview. Ecancermedicalscience. 11:743
Huang Y, Wu H, Luo Z (2017) A retrospective study of optimal surgical management for occult breast carcinoma: mastectomy or quadrantectomy? Medicine (Baltimore) 96(52):e9490
Storm-Dickerson T, Sigalove N (2017) Prepectoral breast reconstruction: the breast surgeon's perspective. Plast Reconstr Surg 140(6S Prepectoral Breast Reconstruction):43S–48S
Herring B, Paraskeva N, Tollow P, Harcourt D (2019) Women's initial experiences of their appearance after mastectomy and/or breast reconstruction: a qualitative study. Psychooncology 28:2076–2082
Mangone M, Bernetti A, Agostini F, Paoloni M, De Cicco FA, Capobianco SV, Bai AV, Bonifacino A, Santilli V, Paolucci T (2019 Jul 30) Changes in spine alignment and postural balance after breast cancer surgery: a rehabilitative point of view. Biores Open Access. 8(1):121–128
de Sire A, Invernizzi M, Lippi L, Cisari C, Özçakar L, Franchignoni F (2019) Blurred lines between axillary web syndrome and Mondor's disease after breast cancer surgery: a case report. Ann Phys Rehabil Med
Invernizzi M, Runza L, De Sire A, Lippi L, Blundo C, Gambini D, Boldorini R, Ferrero S, Fusco N (2020) Integrating augmented reality tools in breast cancer related lymphedema prognostication and diagnosis. J Vis Exp ;(156)
Losco L, Cigna E (2018 Feb 17) Aesthetic refinements in C-V flap: raising a perfect cylinder. Aesthet Surg J 38(2):NP26–NP28
Michelotti A, Invernizzi M, Lopez G, Lorenzini D, Nesa F, De Sire A, Fusco N (2019 Apr) Tackling the diversity of breast cancer related lymphedema: perspectives on diagnosis, risk assessment, and clinical management. Breast. 44:15–23
Thong MSY, van Noorden CJF, Steindorf K, Arndt V (2020 Feb 5) Cancer-related fatigue: causes and current treatment options. Curr Treat Options in Oncol 21(2):17
Yang EJ, Kwon Y (2018) Changes in shoulder muscle activity pattern on surface electromyography after breast cancer surgery. J Surg Oncol 117(2):116–123
Rizzi SK, Haddad CA, Giron PS, Pinheiro TL, Nazário AC, Facina G (2016) Winged scapula incidence and upper limb morbidity after surgery for breast cancer with axillary dissection. Support Care Cancer 24(6):2707–2715
Stubblefield MD (2017) The underutilization of rehabilitation to treat physical impairments in breast cancer survivors. PM R 9(9S2):S317–S323
Leclerc AF, Foidart-Dessalle M, Tomasella M, Coucke P, Devos M, Bruyère O, Bury T, Deflandre D, Jerusalem G, Lifrange E, Kaux JF, Crielaard JM, Maquet D (2017) Multidisciplinary rehabilitation program after breast cancer: benefits on physical function, anthropometry and quality of life. Eur J Phys Rehabil Med 53(5):633–642
Morone G, Iosa M, Fusco A et al (2014) Effects of a multidisciplinary educational rehabilitative intervention in breast cancer survivors: the role of body image on quality of life outcomes. ScientificWorldJournal. 2014:451935
Larsson IM, Ahm Sørensen J, Bille C (2017) The post-mastectomy pain syndrome - a systematic review of the treatment modalities. Breast J 23(3):338–343
Gutman H, Kersz T, Barzilai T, Haddad M, Reiss R (1990) Achievements of physical therapy in patients after modified radical mastectomy compared with quadrantectomy, axillary dissection, and radiation for carcinoma of the breast. Arch Surg 125(3):389–391
de Rezende LF, Franco RL, de Rezende MF, Beletti PO, Morais SS, Gurgel MS (2006) Two exercise schemes in postoperative breast cancer: comparison of effects on shoulder movement and lymphatic disturbance. Tumori. 92(1):55–61
Elder EE, Brandberg Y, Björklund T, Rylander R, Lagergren J, Jurell G, Wickman M, Sandelin K (2005) Quality of life and patient satisfaction in breast cancer patients after immediate breast reconstruction: a prospective study. Breast 14(3):201–208
Shallwani SM, King J, Thomas R, Thevenot O, De Angelis G, Aburub AS, Brosseau L (2019) Methodological quality of clinical practice guidelines with physical activity recommendations for people diagnosed with cancer: a systematic critical appraisal using the AGREE II tool. PLoS One 14(4):e0214846
Castagna A, Frittoli S, Ferrarin M, Del Sorbo F, Romito LM, Elia AE, Albanese A (2016) Quantitative gait analysis in parkin disease: possible role of dystonia. Mov Disord 31(11):1720–1728
Gattellari M, Leung DY, Ukoumunne OC, Zwar N, Grimshaw J, Worthington JM (2011) Study protocol: the DESPATCH study: delivering stroke prevention for patients with atrial fibrillation - a cluster randomised controlled trial in primary healthcare. Implement Sci 6:48
Campbell MJ, Donner A, Klar N (2007) Developments in cluster randomized trials and statistics in medicine. Stat Med 26:2–19
Lo Torto F, Marcasciano M, Kaciulyte J, Redi U, Barellini L, De Luca A, Perra A, Frattaroli JM, Cavalieri E, Di Taranto G, Greco M, Casella D (2020) Prepectoral breast reconstruction with TiLoop® Bra Pocket: a single center prospective study. Eur Rev Med Pharmacol Sci 24(3):991–999
Marcasciano M, Frattaroli J, Mori FLR, Lo Torto F, Fioramonti P, Cavalieri E, Kaciulyte J, Greco M, Casella D, Ribuffo D (2019) The new trend of pre-pectoral breast reconstruction: an objective evaluation of the quality of online information for patients undergoing breast reconstruction. Aesthet Plast Surg 43(3):593–599
Casella D, Di Taranto G, Lo Torto F, Marcasciano M, Kaciulyte J, Greco M, Onesti MG, Ribuffo D (2020) Body mass index can predict outcomes in direct-to-implant prepectoral breast reconstruction. Plast Reconstr Surg 145(4):867e–868e
Crum RM, Anthony JC, Bassett SS, Folstein MF (1993) Population- based norms for the mini-mental state examination by age and educational level. JAMA 269:2386–2391
Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. BMC Med 8:18
Wingate L, Croghan I, Natarajan N, Michalek AM, Jordan C (1989) Rehabilitation of the mastectomy patient: a randomized, blind, prospective study. Arch Phys Med Rehabil 70(1):21–24
Ciesla N, Dinglas V, Fan E, Kho M, Kuramoto J, Needham D (2011) Manual muscle testing: a method of measuring extremity muscle strength applied to critically ill patients. J Vis Exp (50)
Hudak PL, Amadio PC, Bombardier C (1996) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand). The Upper Extremity Collaborative Group (UECG). Am J Ind Med 29(6):602–608
Padua R, Padua L, Ceccarelli E, Romanini E, Zanoli G, Amadio PC, Campi A (2003) Italian version of the disability of the arm, shoulder and hand (DASH) questionnaire: cross-cultural adaptation and validation. J Hand Surg 28(2):179–186
Phan NQ, Blome C, Fritz F, Gerss J, Reich A, Ebata T, Augustin M, Szepietowski JC, Ständer S (2012) Assessment of pruritus intensity: prospective study on validity and reliability of the visual analogue scale, numerical rating scale and verbal rating scale in 471 patients with chronic pruritus. Acta Derm Venereol 92(5):502–507
Postacchini R, Paoloni M, Carbone S, Fini M, Santilli V, Postacchini F, Mangone M (2015) Kinematic analysis of reaching movements of the upper limb after total or reverse shoulder arthroplasty. J Biomech 48(12):3192–3198
Caimmi M, Guanziroli E, Malosio M, Pedrocchi N, Vicentini F, Molinari Tosatti L, Molteni F (2015) Normative data for an instrumental assessment of the upper-limb functionality. Biomed Res Int:484131
Leduc O, Leduc A, Bourgeois P, Belgrado JP (1998) The physical treatment of upper limb edema. Cancer. 83(12 Suppl American):2835-9;
Morone G, Iosa M, Fusco A, Scappaticci A, Alcuri MR, Saraceni VM, Paolucci S, Paolucci T (2014) Effects of a multidisciplinary educational rehabilitative intervention in breast cancer survivors: the role of body image on quality of life outcomes. ScientificWorldJournal. 451935
Paolucci T, Bernetti A, Paoloni M, Capobianco SV, Bai AV, Lai C, Pierro L, Rotundi M, Damiani C, Santilli V, Agostini F, Mangone M (2019) Therapeutic alliance in a single versus group rehabilitative setting after breast cancer surgery: psychological profile and performance rehabilitation. Biores Open Access 8(1):101–110
De Groef A, Van Kampen M, Verlvoesem N, Dieltjens E, Vos L, De Vrieze T, Christiaens MR, Neven P, Geraerts I, Devoogdt N (2017) Effect of myofascial techniques for treatment of upper limb dysfunctions in breast cancer survivors: randomized controlled trial. Support Care Cancer 25(7):2119–2127
Scano A, Chiavenna A, Malosio M, Molinari Tosatti L, Molteni F (2017) Muscle synergies-based characterization and clustering of poststroke patients in reaching movements. Front Bioeng Biotechnol 5:62
Gummesson C, Atroshi I, Ekdahl C (2003) The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord 4:11
Kelly AM (2001) The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J 18(3):205–207
Marazzi F, Masiello V, Marchesano D, Boldrini L, Luzi S, Ferrara PE, Amabile E, Piccari D, Landi F, Moschella F, Franceschini G, Masetti R, Mantini G, Valentini V, Smaniotto D (2019) Shoulder girdle impairment in breast cancer survivors: the role of range of motion as predictive factor for dose distribution and clinical outcome. Tumori. 105(4):319–330
De Groef A, Meeus M, De Vrieze T, Vos L, Van Kampen M, Christiaens MR, Neven P, Geraerts I, Devoogdt N (2017) Pain characteristics as important contributing factors to upper limb dysfunctions in breast cancer survivors at long term. Musculoskelet Sci Pract 29:52–59
Hayes SC, Johansson K, Stout NL, Prosnitz R, Armer JM, Gabram S, Schmitz KH (2012) Upper-body morbidity after breast cancer: incidence and evidence for evaluation, prevention, and management within a prospective surveillance model of care. Cancer. 118(8 Suppl):2237–2249
Ezzo J, Manheimer E, McNeely ML, Howell DM, Weiss R, Johansson KI, Bao T, Bily L, Tuppo CM, Williams AF, Karadibak D (2015) Manual lymphatic drainage for lymphedema following breast cancer treatment. Cochrane Database Syst Rev. (5):CD003475
Franceschini G, Martin Sanchez A, Di Leone A, Magno S, Moschella F, Accetta C, Masetti R (2015) New trends in breast cancer surgery: a therapeutic approach increasingly efficacy and respectful of the patient. G Chir 36(4):145–152
D’Egidio V, Sestili C, Mancino M, Sciarra I, Cocchiara R, Backhaus I, Mannocci A, De Luca A, Frusone F, Monti M, La Torre G, RETURN TO BREAST Collaborative group (2017) Counseling interventions delivered in women with breast cancer to improve health-related quality of life: a systematic review. Qual Life Res 26(10):2573–2592
Acknowledgments
We thank the students in the physiotherapy course at Sapienza University of Rome (Italy)—Lana Zeidan, Pablo Gnessi and Adriano Cecchini—and Francesco De Cicco, a young medical doctor who graduated with a thesis on rehabilitation in breast cancer.
In addition, we thank the Breast Unit of S. Andrea Hospital, Sapienza University of Rome, and specifically, Prof. A. Bonifacino and her team for their valuable collaboration. Finally, we thank the Association of Patients “Incontra Donna,” and all of the women who participated in our research.
Availability of data and materials
Available.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by MM, FA, and AB. The first draft of the manuscript was written by TP,, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Paolucci, T., Bernetti, A., Bai, A.V. et al. The sequelae of mastectomy and quadrantectomy with respect to the reaching movement in breast cancer survivors: evidence for an integrated rehabilitation protocol during oncological care. Support Care Cancer 29, 899–908 (2021). https://doi.org/10.1007/s00520-020-05567-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05567-x