Abstract
Purpose
Loss of appetite is a common side effect of cancer and cancer treatments resulting in risk of malnutrition and cancer cachexia. This review aimed to systematically determine nutrition interventions that improve appetite and nutrition-related outcomes of adults with cancer undergoing cancer treatments, and to identify appetite assessment tools used to measure appetite.
Methods
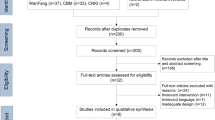
Inclusion criteria included randomised controlled trials of adults with cancer undergoing chemotherapy, radiotherapy or immunotherapy treatments, nutrition interventions and appetite assessed by an appetite assessment tool or quality of life tool. The search strategy was applied to four databases and two researchers systematically assessed for eligibility. Following data extraction, quality of the included library was assessed using the Quality Criteria Checklist: Primary Research. A narrative synthesis of results was undertaken.
Results
After title/abstract screening, 24 full texts were assessed for eligibility; five trials of n = 472 participants were included in the final library. Nutrition interventions that improved appetite were oral nutrition supplements, fish oil supplements and dietary counselling. Appetite was assessed via visual analogue scales (n = 1) and EORTC QLQ C30 questionnaire (n = 4). Quality was assessed as neutral in 2 studies and positive in 3 studies.
Conclusion
The use of oral nutrition supplements and dietary counselling and increases in EPA from fish oil supplementation improved the appetite and nutrition outcomes of patients with cancer undergoing cancer treatments. Validated assessment tools in the oncology setting are needed to determine which nutrition interventions positively influence appetite outcomes.

Similar content being viewed by others
References
Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, Jatoi A, Loprinzi C, MacDonald N, Mantovani G, Davis M, Muscaritoli M, Ottery F, Radbruch L, Ravasco P, Walsh D, Wilcock A, Kaasa S, Baracos VE (2011) Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 12(5):489–495. https://doi.org/10.1016/s1470-2045(10)70218-7
Tarricone R, Ricca G, Nyanzi-Wakholi B, Medina-Lara A (2016) Impact of cancer anorexia-cachexia syndrome on health-related quality of life and resource utilisation: a systematic review. Crit Rev Oncol Hematol 99:49–62. https://doi.org/10.1016/j.critrevonc.2015.12.008
Fearon K, Voss A, Hustead D (2006) Definition of cancer cachexia: effect of weight loss, reduced food intake, and systemic inflammation on functional status and prognosis. Am J Clin Nutr 83(6):1345–1350. https://doi.org/10.1093/ajcn/83.6.1345
Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, Fearon K, Hutterer E, Isenring E, Kaasa S, Krznaric Z, Laird B, Larsson M, Laviano A, Muhlebach S, Muscaritoli M, Oldervoll L, Ravasco P, Solheim T, Strasser F, de van der Schueren M, Preiser JC (2017) ESPEN guidelines on nutrition in cancer patients. Clin Nutr 36(1):11–48. https://doi.org/10.1016/j.clnu.2016.07.015
Dewys WD, Begg C, Lavin PT, Band PR, Bennett JM, Bertino JR, Cohen MH, Douglass HO, Jr., Engstrom PF, Ezdinli EZ, Horton J, Johnson GJ, Moertel CG, Oken MM, Perlia C, Rosenbaum C, Silverstein MN, Skeel RT, Sponzo RW, Tormey DC (1980) Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am J Med 69 (4):491–497. doi:https://doi.org/10.1016/s0149-2918(05)80001-3
Baracos V, Kazemi-Bajestani SM (2013) Clinical outcomes related to muscle mass in humans with cancer and catabolic illnesses. Int J Biochem Cell Biol 45(10):2302–2308. https://doi.org/10.1016/j.biocel.2013.06.016
Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ, Murphy R, Ghosh S, Sawyer MB, Baracos VE (2013) Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol 31(12):1539–1547. https://doi.org/10.1200/jco.2012.45.2722
Aredes MA, Garcez MR, Chaves GV (2018) Influence of chemoradiotherapy on nutritional status, functional capacity, quality of life and toxicity of treatment for patients with cervical cancer. Nutr Diet 75(3):263–270. https://doi.org/10.1111/1747-0080.12414
Botero L, Agarwal E, Berry R, Gillespie K, Isenring E, McCarthy AL (2019) Nutrition risk and mortality in older oncology patients: an exploratory study. Nutr Diet. https://doi.org/10.1111/1747-0080.12547
Hopkinson JB, Wright DN, McDonald JW, Corner JL (2006) The prevalence of concern about weight loss and change in eating habits in people with advanced cancer. J Pain Symptom Manag 32(4):322–331. https://doi.org/10.1016/j.jpainsymman.2006.05.012
Quinten C, Coens C, Mauer M, Comte S, Sprangers MA, Cleeland C, Osoba D, Bjordal K, Bottomley A (2009) Baseline quality of life as a prognostic indicator of survival: a meta-analysis of individual patient data from EORTC clinical trials. Lancet Oncol 10(9):865–871. https://doi.org/10.1016/s1470-2045(09)70200-1
Castillo-Martínez L, Castro-Eguiluz D, Copca-Mendoza ET, Pérez-Camargo DA, Reyes-Torres CA, Ávila EA-D, López-Córdova G, Fuentes-Hernández MR, Cetina-Pérez L, Milke-García MDP (2018) Nutritional assessment tools for the identification of malnutrition and nutritional risk associated with cancer treatment. Rev Investig Clin 70(3):121–125. https://doi.org/10.24875/RIC.18002524
Ozorio GA, de Almeida M, Faria SO, Cardenas TC, Waitzberg DL (2019) Appetite assessment of hospitalized cancer patients in Brazil - a validation study. Clinics (Sao Paulo) 74:e1257. https://doi.org/10.6061/clinics/2019/e1257
Zhang F, Shen A, Jin Y, Qiang W (2018) The management strategies of cancer-associated anorexia: a critical appraisal of systematic reviews. BMC Complement Altern Med 18(1):236–236. https://doi.org/10.1186/s12906-018-2304-8
Baldwin C, Spiro A, Ahern R, Emery PW (2012) Oral nutritional interventions in malnourished patients with cancer: a systematic review and meta-analysis. J Natl Cancer Inst 104(5):371–385. https://doi.org/10.1093/jnci/djr556
Cox NJ, Ibrahim K, Sayer AA, Robinson SM, Roberts HC (2019) Assessment and treatment of the anorexia of aging: a systematic review. Nutrients 11(1). https://doi.org/10.3390/nu11010144
Childs DS, Jatoi A (2019) A hunger for hunger: a review of palliative therapies for cancer-associated anorexia. Ann Palliat Med 8(1):50–58. https://doi.org/10.21037/apm.2018.05.08
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Academy of Nutrition and Dietetics: Evidence analysis manual: steps in the academy evidence analysis process. (2016) Chicago, IL: Academy of Nutrition and Dietetics.
Ravasco P, Monteiro-Grillo I, Marques Vidal P, Camilo ME (2005) Impact of nutrition on outcome: a prospective randomized controlled trial in patients with head and neck cancer undergoing radiotherapy. Head Neck 27(8):659–668. https://doi.org/10.1002/hed.20221
Ravasco P, Monteiro-Grillo I, Vidal PM, Camilo ME (2005) Dietary counseling improves patient outcomes: a prospective, randomized, controlled trial in colorectal cancer patients undergoing radiotherapy. J Clin Oncol 23(7):1431–1438
Werner K, Kullenberg de Gaudry D, Taylor LA, Keck T, Unger C, Hopt UT, Massing U (2017) Dietary supplementation with n-3-fatty acids in patients with pancreatic cancer and cachexia: marine phospholipids versus fish oil - a randomized controlled double-blind trial. Lipids Health Dis 16(1):104
Sanchez-Lara K, Turcott JG, Juarez-Hernandez E, Nunez-Valencia C, Villanueva G, Guevara P, De la Torre-Vallejo M, Mohar A, Arrieta O (2014) Effects of an oral nutritional supplement containing eicosapentaenoic acid on nutritional and clinical outcomes in patients with advanced non-small cell lung cancer: randomised trial. Clin Nutr 33(6):1017–1023
Ziętarska M, Krawczyk-Lipiec J, Kraj L, Zaucha R, Małgorzewicz S (2017) Chemotherapy-related toxicity, nutritional status and quality of life in precachectic oncologic patients with, or without, high protein nutritional support. A prospective, randomized study. Nutrients 9(10). https://doi.org/10.3390/nu9101108
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376. https://doi.org/10.1093/jnci/85.5.365
Barajas Galindo DE, Vidal-Casariego A, Calleja-Fernández A, Hernández-Moreno A, Pintor de La Maza B, Pedraza-Lorenzo M, Rodríguez-García MA, Ávila-Turcios DM, Alejo-Ramos M, Villar-Taibo R (2017) Appetite disorders in cancer patients: impact on nutritional status and quality of life. Appetite 114:23–27. https://doi.org/10.1016/j.appet.2017.03.020
Ijpma I, Renken R, Horst G, Reyners A (2016) The palatability of oral nutritional supplements: before, during, and after chemotherapy. Support Care Cancer 24(10):4301–4308. https://doi.org/10.1007/s00520-016-3263-6
Bauer J, Capra S, Ferguson M (2002) Use of the scored Patient-Generated Subjective Global Assessment (PG-SGA) as a nutrition assessment tool in patients with cancer. Eur J Clin Nutr 56(8):779–785. https://doi.org/10.1038/sj.ejcn.1601412
Ferguson M, Capra S, Bauer J, Banks M (1999) Development of a valid and reliable malnutrition screening tool for adult acute hospital patients. Nutrition 15(6):458–464. https://doi.org/10.1016/s0899-9007(99)00084-2
Acknowledgements
Eastern Health Stepping into Research Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 92 kb)
Rights and permissions
About this article
Cite this article
Ukovic, B., Porter, J. Nutrition interventions to improve the appetite of adults undergoing cancer treatment: a systematic review. Support Care Cancer 28, 4575–4583 (2020). https://doi.org/10.1007/s00520-020-05475-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05475-0